Aggressively Presenting Colloid Cyst (C C) in a 10-Year Boy: Correlation of Density Appearance on CT scan and Role of Emergency External Ventricular Drain
Guru Dutta Satyarthee1, *, Shikha Satyarthee2, Amit Handa3,
Shushil Kumar3
1Department of Neurosurgery, Neurosciences Centre, AIIMS New Delhi, India
2Summer Training, St Stephen’s Hospital, Delhi, India
3Department of Neurosurgery, St Stephen’s Hospital, Delhi, India
Abstract
Keywords
Pediatric Colloid Cyst, Aggressive Course, External Ventricular Drain, Hyperdense
Received: June 4, 2016
Accepted: July 22, 2016
Published online: August 16, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Colloid cysts are rare benign intracranial non-neoplastic cysts occurring in the third ventricle. It usually presents in second or third decades of life, but also occasionally reported in paediatric population. Its incidence is about three persons per million per year [1]. Although classically CC occurs during third to fifth decades of life, rarely may occur also in children and young age. The colloid cyst usually unilocular mass in the region of Foramen Monro [1, 2, 3, 4] It is lined with a single layer thick columnar epithelial, which secret mucin inside the cyst, which progressively accumulate and dislodge the entire cyst to block foramen of Monro producing sudden obstruction of the CSF pathway [5,6]. The content of colloid cyst includes mucin, cholesterol, and bleed. Colloid cysts may present with a spectrum of clinical presentation and range varying from mild intermittent headaches to non-specific symptoms and occasionally sudden deaths. Although headache is the most common symptom of CC. Cases of sudden death due to colloid cysts could be failure of notice headache as ominous symptoms. The variety and composition of the content of the colloid cyst is basically responsible for spectrum of imaging finding on magnetic resonance imaging study.
2. Case- Illustration
A10 –year- old boy presented with altered sensorium for one day with past history of progressive headache for last three weeks. On Examination, a GCS score was E3V4M5 with pupil sluggishly reacting and papilloedema bilaterally and rest of examination were normal. CT scan head revealed well defined mass lesion of size 2.7x2.2x2.5 cm located in the anterior third ventricle near foramen of Monro. (Fig-1) MRI brain corroborated above finding of well defined, rounded lesion with altered signal intensity hyperintense to CSF with some foci of hyperintense foci on T1W image, homogeneous hyperintense signal with foci of hypointense on T2W image and no contrast enhancement. Suggestive of Colloid cyst with foci of bleed, which was showing hyperintense signal on T1W imaging and also hyperintense signal on T2W imaging within spenium of corpus callosum with diffuse effacement of cortical sulci along with presence of obstructive hydrocephalus. He needed an urgent external ventricular drain and was placed in causality.
Definitive surgery was carried out two days later, using right fronto- parietal craniotomy utilizing anterior transcallosal-transforaminal corridor after incision over corpus callosum, lateral ventricle and dilated foramen of Munro was observed and near-total excision done. External ventricular drainage was removed on fifth days. Postoperative CT scan showed complete excision of cyst with small contusion over right frontal lobe. (Fig-2) Magnetic resonance imaging done during follow-up shows no residual with subsidence of obstructive hydrocephalus. (Fig-3) In the post-operative period he developed left sided hemiparesis of 4/5 in which recovered over three weeks.
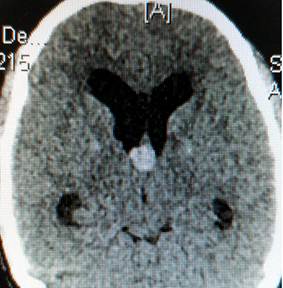
Fig. 1. Non-contrast computed tomography scan showing hyperdense mass in third ventricle, blocking foramen Monro causing obstructive hydrocephalus.

Fig. 2. Non-contrast computed tomography scan of head, in the postoperative period showing evidence of brurrhole and complete excision of colloid cyst of in the third ventricle, with opening of foramen Monro with of partial relief obstructive hydrocephalus.
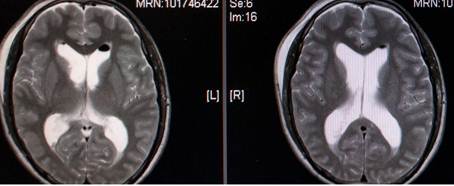
Fig. 3. Non-contrast magnetic resonance imaging brain in the post-operative phase, axial section, T2w image, showing no residual of colloid cyst in third ventricle, with air pocket in the frontal horn of the right lateral ventricle, with re-opening of foramen Monro causing amelioration of pre-operative obstructive hydrocephalus.
3. Discussion
Colloid cyst is rare benign intracranial lesions of endodermis origin, accounting approximately for 0.2-2.0% of all intracranial tumors. [7] It originates due to aberrant folding of the primitive neuroepithelium [5, 6] arise from the inferior aspect of septum pellucidum and protrude into the anterior portion of the third ventricle between columns of fornix. CC is considered as non-neoplastic, true epithelium lined cysts of the central neuraxis. Usually CC is smooth outlined, round lesions located at the antero-superior aspect of the third ventricle and size can range from 3–40 mm in diameter [8-12].
It is commonly presents during the second or third decade of life with chronic symptoms but also reported occasionally in childhood. It runs usually more aggressive clinical course with increased propensity to cause rapid and progressive deterioration in neurological status in children comparing to the adult hood colloid cyst cases. [1,2] It can present with a spectrum of clinical presentation varying from being completely asymptomatic or occasional headaches to rapid onset and progressive decline in consciousness, and even sudden death. CC generally presents with ventricular outflow obstruction manifestations, as consequence of peculiar location at the foramen of Monro in the anterior aspect of the third ventricle. The chief presenting complaint of CC is headache. Headache is attributed to transient obstruction secondary to ball valve mechanism at the foramen of Monro. An associated symptom of CC includes memory deficit, diplopia and vertigo. [5,9,11,13,15]
So, high index of clinical suspicion and timely intervention is warranted as a life saving measure. Other commonly encountered symptoms include headache, vertigo, memory deficit and diplopia and associated behavioural disturbances. [17] Headache is classically episodic, intermittent, occasional very severe intensity and used to get relieved on lying down which is unusual for a headache caused due to an intracranial mass lesion. As such headache is neither characteristic nor specific for colloid cyst.
Mechanisms of rapid clinically deterioration or even sudden death as previously postulated include sudden blockage at the foramen of Monro by lodgement of colloid cyst by occluding CSF flow leading to acute attack of hydrocephalus and sudden hydrocephalus development, bleed into cyst cavity or sudden venous hypertension in sagittal sinus or even reflex originating from cardiovascular centres located in the vicinity of third ventricle are incriminated. [1, 3] Various risk factor associated with rapid deterioration are younger age at presentation, associated hydrocephalus, density of colloid cyst, size, and rate of increase in the size of colloid cyst and associated bleed inside the colloid cyst [1,2,4].
Histologically lining of cyst wall of CC is lined by cuboidal, columnar or pseudostratified and mucus-secreting epithelial cells. CC contains mucinous and gelatinous material as content. Occasionally hemosiderin pigment and xanthogranulomas are also observed.
Cranial CT scan shows typically rounded single locular, hyperdense mass lesion at the roof of the third ventricle and commonly producing obstructive hydrocephalus with calcification presence is very uncommon. [5] Important differential of third ventricle roof lesions are calcified meningioma, astrocytoma, or remains of past bleed at foramen of Monro. [6] Urso et al. tried to correlated the aggressive behaviour of colloid cyst with hydration status of colloid cyst contents and observed CT scan density findings and suggested rapidly progression of symptoms in children may be attributed to presence of relatively higher water content as compared to adult counterpart and also related to relative rapid progression of cyst enlargement [4] Further Kapu et al. also observed hyperdensity of the colloid cyst correlated well with aggressive clinical course [7] Magnetic resonance imaging shows CC as hyperintense signal T1 as well as T2 weighted image sequences [8]
Management of colloid cyst is challenging, depends size, associated hydrocephalus, facility of endoscopic surgery, surgeons preference and experiences, familiarity with various approaches and patient preferences. [13, 15, 16] In emergency, temporary CSF diversion can be achieved with placement of external ventricular drain; however with facility of endoscopic surgery, it can obviate the risk of external ventricular drain placement with excision of Colloid cyst and, which also relieves hydrocephalus. [15,17,18] However various transcranial surgery approaches are interhemispheric transcallosal or transcortical with its appropriate indication and its associated sequlae. However, minimally invasive surgical technique is currently vogue. So aspiration under stereotactic guidance is a useful diagnostic tool [8]. However, endoscopic assisted colloid cyst excision plays a pivotal role in the management of CC.
Pollock et al analyzed 162 patients to analyze the natural history of incidentally discovered colloid cysts, sixty-eight patients (42%) were thought to be asymptomatic with regard to their colloid cyst and observation with serial neuroimaging was recommended. [19] The mean patient age was 57 years at the time of diagnosis; mean size of the colloid cyst was 8 mm with the range 4–18 mm. The CT scan head showed a hyperdense cyst in 84% cases clinical follow-up evaluation was available at a mean of 79 months in the remaining 58 patients. The numbers of patients who were followed-up at 2, 5, and 10 years after diagnosis were 40, 28, and 14, respectively. The incidences of symptomatic progression related to the cyst were 0%, 0%, and 8% at 2, 5, and 10 years, respectively. None of the patient died suddenly during the follow-up interval. Those patients with asymptomatic colloid cysts are diagnosed can be followed up safely with observation and serial neuroimaging. However, if a patient becomes symptomatic, or cyst enlargement occurs, or developing gross hydrocephalus s, prompts neurosurgical intervention is necessary to prevent the neurological morbidity and mortality [14].
4. Conclusion
A possibility and high index of suspicion should be kept for colloids cyst in every children, who presents with rapid progression of raised intracranial pressure features with presence of typical characteristic headache, which is intermittent, episodic, intense and severe, which usually gets relief on lying down and bending forward like posture used while tying shoe laces in bending forward pose.
References
- Hernesniemi J, Leivo S. Management outcome in third ventricular colloid cysts in a defined population; a series of 40 patients treated mainly by transcallosal microsurgery. Surg Neurol. 1996;45:2-14.
- Kelly R. Colloid cysts of the third ventricle: Analysis of twenty-nine cases. Brain 1951; 74:23-65.
- Opeskin K, McD Anderson R, Lee KA. Colloid cyst of the 3rd ventricle as a cause of acute neurological deterioration and sudden death. J Paediatr Child Health 1993;29:476-7.
- Urso JA, Ross GJ, Parker RK, Patrizi JD, Stewart B. Colloid cyst of the third ventricle: Radiologic-pathologic correlation. J Comput Assist Tomogr 1998; 22:524-728.
- Waggenspack GA, Guinto FC. MR and CT of masses of the anterosuperior third ventricle. AJR Am J Roentgenol. 1989;152 (3):609-14.
- Osborn AG, Preece MT. Intracranial cysts: radiologic-pathologic correlation and imaging approach. Radiology. 2006;239: 650-64.
- Kapu R, Symss NP, Pande A, Vasudevan MC, Ramamurthi R. Management of pediatric colloid cysts of anterior third ventricle: A review of five cases. J Pediatr Neurosci 2012;7:90-96.
- Abernathey CD, Davis DH, Kelly PJ. Treatment of colloid cysts of the third ventricle by stereotaxic microsurgical laser craniotomy. J Neurosurg. 1989; 70:525–529.
- Colice GL. Neurogenic pulmonary oedema. Clin Chest Med. 1985;Mamourian AC, Cromwell LD, Harbaugh RE. Colloid cyst of the third ventricle: sometimes more conspicuous on CT than MR. AJNR Am J Neuroradiol. 1998;19:875–878.
- Hadley DM. Colloid cyst of the III ventricle. Neurol Neurosurg Psychiatry. 2002;72:15–15.
- Smith WS, Matthay MA. Evidence for a hydrostatic mechanism in human neurogenic pulmonary oedema. Chest. 1997; 111:1326–1333.
- Hamlat A, Pasqualini E, Askar B. Hypothesis about the physiopathology of acute deterioration and sudden death caused by colloid cysts of the third ventricle. Med Hypotheses. 2004;63:1014–1017.
- Rosenblum MK. Neuromuscular system: central nervous system. In: Rosai J, editor. Rosai and Ackerman's Surgical Pathology. 9. Vol. 2. Philadelphia: Mosby; 2004. pp. 2467–2468.
- Pollock BE, Huston J., 3rd Natural history of asymptomatic colloid cysts of the ventricle. J Neurosurg. 1999;91:364–369.
- Partington MW, Bookalil AJ. Familial colloid cysts of the third ventricle. Clin Genet. 2004;13:473–475.
- Satyarthee GD, Mahapatra A.K. Migration and subgaleal coiling of distal components of a V-P shunt in a 2-year boy: Does electrical stimulation as part of physiotherapy is cause or casual association?Romanian neurosurgery 2015;29 (2):195-198.
- Satyarthee Guru Dutta, Satyarthee S. Spontaneous CSF Rhinorrhoea as Presenting Symptom of Neglected Aqueductal of Sylvian Stenosis and Obstructive Hydrocephalus: Management Review American Journal of Clinical Neurology and Neurosurgery2016; 2:14-17.
- Satyarthee G D, Gopal K. Post - Traumatic Thick Acute Subdural Hematoma in Child Showing Rapid Deterioration Managed with Burr - Hole Evacuation Surgery with Drain: A Novel Rescue Technique A J Cli Neurol Neurosurg 2016; 2:18-21.
- Pollock BE, Huston J 3rd J Neurosurg. Natural history of asymptomatic colloid cysts of the third ventricle.1999 Sep;91(3):364-9.