Use of Mannitol Salt Agar (MSA) and Cefoxitin as a Selective Culture Medium for Growing MRSA Strains
Abdulhadi Sale Kumurya*
Department of Medical Laboratory Science, Faculty of Allied Health Sciences, Bayero University, Kano, Nigeria
Abstract
Where laboratories are performing antimicrobial susceptibility testing using cefoxitin, Staphylococcus aureus will likely be correctly identified as methicillin-resistant Staphylococcus aureus (MRSA). Importantly, cefoxitin has been found to be more reliable than oxacillin in disc diffusion, broth microdilution, and agar dilution assays. A balanced opening out of this attempt is the inclusion of cefoxitin into media which is selective for MRSA. This work illustrates the testing of mannitol salt agar containing 4 mg/liter cefoxitin with a unique set of well-characterized MRSA strains and an equal number of known methicillin susceptible Staphylococcus aureus (MSSA) strains. The agar supported the growth of 96.6% of the MRSA strains in the set and inhibited the growth of 100% of the MSSA strains. The study indicates that selective media based on cefoxitin are better to those based on oxacillin for the detection of MRSA. The findings of this study demonstrate that cefoxitin is far superior to oxacillin when it is used in mannitol salt medium. By the use of a 48-h incubation and a 102-CFU/ml inoculum, the sensitivity and specificity of the cefoxitin MSA plate method were 100% (compared to 90.7% with oxacillin) and 100% (compared to 96.0% for oxacillin), respectively, when the comparison was made for the strains used in both studies.
Keywords
MRSA, MSA, Cefoxitin, Selective Media, Growth, Staphylococcus aureus
Received: January 1, 2017
Accepted: January 17, 2017
Published online: February 28, 2017
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
The conventional culture media which can be selective for growing of methicillin-resistant Staphylococcus aureus (MRSA) include mannitol salt agar (MSA), blood agar, or Baird-Parker agar containing methicillin or oxacillin alone or in combination with other antibiotics. An enrichment step consisting of culture in nutrient broth with up to 7.5% sodium chloride prior to inoculation of one of the selective agars mentioned above has also been supported. There are many literatures [2, 3, 5, 7, 10] describing screening media for MRSA, and this probably reveals the fact that phenotypic methods based on methicillin or oxacillin have never achieved levels of sensitivity and specificity which have been totally satisfactory. Nevertheless, I have continued to base my screening media on these agents simply because I have had nothing better. Some reports [4, 8, 9] have revealed that cefoxitin is a better agent for forecast of methicillin resistance in S. aureus, and disk susceptibility testing with cefoxitin now replaces disk susceptibility testing with methicillin and oxacillin in many centers. This work describes the use of an assortment of well-characterized MRSA strains in the growth of MRSA on selective medium which substitutes oxacillin with cefoxitin.
Where laboratories are performing antimicrobial susceptibility testing, mecC MRSA will likely be correctly identified as MRSA. Importantly, cefoxitin has been found to be more reliable than oxacillin in disc diffusion, broth microdilution, and agar dilution assays [13]. However, significant differences in the reliability of agars from different manufacturers have been described [13]. Similarly, mecC MRSA produce a distinctive antibiotic susceptibility profile compared to mecA MRSA when assayed using the automated Vitek 2 system from BioMérieux [14]. Where both oxacillin and cefoxitin are included, mecA MRSA, as might be expected, typically display resistance to both. By contrast, the majorities of mecC MRSA show resistance to cefoxitin, and are therefore reported as MRSA, but however show susceptibility to oxacillin. Testing of a panel of 896 S. aureus isolates (comprising mecA MRSA, mecC MRSA, and mec-negative MSSA) found that this oxacillin-sensitive/cefoxitin-resistant profile had a sensitivity of 88.7% and a specificity of 99.5% for the identification of mecC MRSA isolates from MSSA and mecA MRSA [14]. This profile therefore provides a zero-cost screening method for identification of mecC-positive MRSA strains in the many clinical laboratories already using Vitek 2, although subsequent PCR would be needed to confirm mecC status.
The differences in oxacillin and cefoxitin sensitivities displayed by mecC MRSA isolates are consistent with the findings of Kim et al. discussed above, demonstrating that the mecC-encoded PBP2a, unlike the mecA-encoded counterpart, has a higher relative affinity for oxacillin than for cefoxitin, leading to higher levels of resistance to cefoxitin than to oxacillin [12]. mecC MRSA appear to grow reliably on commercial chromogenic agar plates designed to identify MRSA, although there are indications that some MRSA agars may perform better than others for the recovery of mecC MRSA [15]. mecC MRSA typically have lower MICs to oxacillin and cefoxitin than their mecA counterparts, and this may affect their recovery on selective agars.
2. Materials and Methods
2.1. Bacterial Strains
A total of 25 methicillin-susceptible Staphylococcus aureus and 25 methicillin-resistant Staphylococcus aureus strains, and two control strains of Staphylococcus aureus; one methicillin-resistant Staphylococcus aureus strain (ATCC 33591) and one methicillin-susceptible Staphylococcus aureus strain (ATCC 29213) were used in the study.
2.2. Polymerase Chain Reaction (PCR)
The presence or absence of the mecA gene was determined for all isolates by PCR which was used in categorizing the MSSA and MRSA strains. PCR assays were all directly performed from the bacterial suspension obtained after the rapid DNA extraction method described previously [16, 17, 18, 19]. An aliquot of 5 µl of this suspension was added to 95 µl of PCR mixture consisting of 1× reaction buffer [16 mM (NH4)2SO4, 67 mMTris-HCl (pH 8.8)], a 0.5 mM concentration of each of the four deoxyribonucleoside triphosphates (dATP, dCTP, dGTP, and dTTP) (Inqaba Biotechnical Industries (Pty) Ltd., South Africa), 1.0μM of each primer, and mecA primer (described in Table 1), and 1.25 U of The Dream Taq™ Green PCR Master Mix (2x) (Fermentas Life Sciences, supplied by Inqaba Biotechnical Industries (Pty) Ltd., South Africa) is a ready-to-use solution containing Dream Taq™ DNA polymerase, optimized Dream Taq™ Green buffer and 4mMMgCl2. For each sample, one reaction was performed with the pair of primers to identify S. aureus specific sequence gene and with the mecA pairs of primers to detect both resistance gene (mecA). In order to reduce the formation of nonspecific extension products, a hot-start PCR protocol was used; the tubes were placed in the thermal cycler when the denaturing temperature was reached. All PCR assays were carried out with a negative control containing all of the reagents without DNA template. DNA amplification was carried out in a Techne PCR system TC-5000 thermo cycler (Bibby Scientific Ltd.) with the following thermal cycling profile: initial denaturation step at 94°C for 5 min was followed by 1 cycle of amplification this was followed by denaturation at 94°C for 30 s, annealing at 55°C for 30 s, and extension at 72°C for 60 s ending with a final extension step at 72°C for 5 min. After PCR amplification, 5 µl was removed and subjected to agarose gel electrophoresis (1.5% agarose, 1× Tris-borate-EDTA, 100 V, 40 min) to estimate the sizes of the amplification products by comparison with a 100-bp O’ GeneRuler™ 100bp molecular size standard DNA Ladder, ready-to-use designed by Fermentas Life sciences (supplied by Inqaba Biotechnical Industries (Pty) Ltd., South Africa) The gel was stained with ethidium bromide, and the amplicons were visualized using a UV light box. This protocol, including the rapid DNA extraction method from a single colony and electrophoretic analysis of the amplified products on an agarose gel, was performed in less than 4 hours.
2.3. MIC and Strains Growth
The MICs for the 50-strain collection were determined by using Etest (AB Biodisk, Solna, Sweden) on Iso-Sensitest Agar (Oxoid, Basingstoke, United Kingdom).
MSA (DM160D) (Mast Diagnostics, Merseyside, United Kingdom) plates were prepared with cefoxitin (Sigma-Aldrich, Solna, Sweden) at concentrations of 2, 3, or 4 mg/liter. The test strains were applied at concentrations of 102 and 105 viable organisms in the following way: the suspensions were prepared by using fresh overnight cultures on blood agar, matched to a McFarland standard, and diluted in phosphate-buffered saline to suspensions such that when 1 μl was applied with a disposable loop and spread over an area of approximately 6 cm by 2 cm, a count of either 100 or 100,000 colonies was achieved. A control plate of blood agar was used for each strain and dilution. Incubation was carried out in air at 35°C for 48 h, and the result was read at 18 and 48 h. The growth of any visible colonies after incubation was recorded as a positive result. The remaining strains were tested as described above, but only on MSA containing 4 mg/liter cefoxitin.
3. Results
The MIC results for the 50-strain collection were as follows: all 25 MSSA strains exhibited cefoxitin MICs of ≤2 mg/liter. Seven mecA-positive strains had MICs of 4 mg/liter, and the remaining 68 MRSA strains had MICs >4 mg/liter.
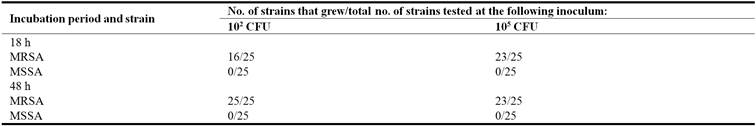
MSA plates with 2 mg/liter cefoxitin allowed the growth of all MRSA and MSSA strains after 48 h incubation. MSA with 3 mg/liter cefoxitin allowed the growth of only four MSSA strains and all of the MRSA strains. None of the 25 MSSA strains grew on MSA containing 4 mg/liter cefoxitin but all 75 MRSA strains grew on it. The growth of all strains at 18 h and at 48 h is shown in Table 1.
Table 1. Growth of MSSA and MRSA strains on MSA containing 4 mg/liter cefoxitin.
4. Discussion
There are many laboratory methods for detection of methicillin resistant in S. aureus. Most laboratories use disk diffusion methods for routine testing. The goal standard, for antimicrobial susceptibility testing has been the MIC determination by a dilution or E – test method. In recent years MIC methods has been replaced by molecular methods that detect mecA gene. However, the use of this assay is largely restricted to reference centers [20]. For many years methicillin or oxacillin has been the agent of choice in selective media like mannitol salt agar for the detection of methicillin resistance in Staphylococcus aureus. Mannitol and salt have frequently been combined as an aid in identification and a selective agent, respectively. Mannitol salt agar with 1 mg/liter oxacillin was revealed to have a sensitivity of 92.0% and a specificity of 96.0% [10] for the strains used in this study. A similar medium, oxacillin resistant screening agar [1], which is also based on mannitol, salt, and lithium chloride but which contains 2 mg/liter oxacillin, was shown to have a sensitivity of 64% when it was used to test patient specimens plated directly, although its sensitivity increased when it was combined with an enrichment broth.
In recent years cephalosporins have been reported to be particularly successful when they are used as an alternative to oxacillin. A phenyl red mannitol broth containing aztreonam and ceftizoxime [11] allowed the growth of all reference MRSA strains tested, although only a small number of strains were tested. Disks containing the cephamycins cefoxitin and moxalactam on Mueller-Hinton agar were shown to be 100% sensitive and specific for the differentiation of MRSA and MSSA [4]. By the use of Iso-Sensitest agar and a 30-μg cefoxitin disk, a similarly high sensitivity and specificity were reported for a total of 457 Staphylococcus aureus strains, many of which exhibited low-level resistance to oxacillin [8]. A recent report that described the use of a chromogenic medium and cefoxitin [6] indicated that this medium showed a sensitivity of 89% and a specificity of 99.5% for the detection of MRSA in clinical material.
The findings of this study clearly demonstrate that cefoxitin is far superior to oxacillin when \it is used in this particular mannitol salt medium. By the use of a 48-h incubation and a 102-CFU/ml inoculum, the sensitivity and specificity of the cefoxitin MSA plate method were 100% (compared to 92.0% with oxacillin) and 100% (compared to 96.0% for oxacillin), respectively, when the comparison was made for the strains used in both studies. The strains of MRSA used give inhibition zones which fall within ±3 mm of the recommended zone breakpoint for cefoxitin [9].
It is good to understand, nonetheless, that all MSA media are not similar; their salt contents vary, and this may influence the growth of some strains [10]. The particular MSA used in the present study contains 3% salt, whereas most other commercially produced MSA media contain 7.5% salt, and the results reported in this study may not be achievable with other brands.
The use of two inocula serves to demonstrate the "inoculum effect" on the time to detection. Small numbers of bacteria take longer to produce visible growth, up to 48 h in this study, while heavier inocula, such as those produced after overnight incubation in enrichment broth; can produce growth on solid media 24hours prior [1]. The selection of the two inocula was based on the probable numbers of bacteria in specimens without enrichment (102) and after enrichment (105). The medium used requires 48 h of incubation without the use of an enrichment stage.
The medium used in this study has proved to be strong and consistent for routine use. Clinical sample is plated straight on the medium, and the plates are examined after 24 hours of incubation. Yellow colonies are tested by free coagulase and cefoxitin susceptibility tests. Those strains that test positive for coagulase and that are resistant to cefoxitin can further be tested by the MRSA latex test, and then a presumptive detection of MRSA is prepared. At this point, many laboratories would use a PCR test for the mecA gene for confirmation, and in areas where MRSA is frequently detected, it may be good enough to belief the results of the cefoxitin disk test. Plates which are negative at 18 h are incubated for a further 24 h before they are discarded. The number of Staphylococcus aureus strains which are mannitol negative is not known, but as far as this study is able to discover, the number is low and none of the strains in the collection (which were not selected by using MSA medium) were mannitol negative. However, ever more frequently patient specimens contain methicillin-resistant (and cefoxitin-resistant) coagulase-negative staphylococci (CoNS). These are capable of growth on the medium, but S. epidermidis produces pink colonies, which are easily distinguishable from the yellow (mannitol-positive) colonies of S. aureus. A number of CoNS other than S. epidermidis are mannitol positive and therefore produce yellow colonies. In an area with a higher prevalence, MRSA will completely dominate the findings and CoNS will not be supposed as a problem. Irrespective of the prevalence of MRSA, since one has to do the cefoxitin test at this point anyway, the addition of a few negative coagulase tube tests which can be discarded before further work is done is of little significance.
5. Conclusion
The study indicates that selective media based on cefoxitin are better to those based on oxacillin for the detection of MRSA. The findings of this study demonstrate that cefoxitin is far superior to oxacillin when it is used in mannitol salt medium. By the use of a 48-h incubation and a 102-CFU/ml inoculum, the sensitivity and specificity of the cefoxitin MSA plate method were 100% (compared to 92.0% with oxacillin) and 100% (compared to 96.0% for oxacillin), respectively, when the comparison was made for the strains used in both studies.
References
- Blanc, D. S., A. Wenger, and J. Bille. 2003. Evaluation of a novel medium for screening specimens from hospitalized patients to detect methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 41: 3499-3502.
- Cuny, C., and W. Witte. 1998. Methicillin-resistant Staphylococcus aureus—diagnostic aspects. Biotest Bull. 6: 51-57.
- Davies, S., and P. M. Zadik. 1997. Comparison of methods for the isolation of methicillin resistant Staphylococcus aureus. J. Clin. Pathol. 50: 257-258.
- Felton, A., B. Grandry, P. H. Lagrange, and I. Casin. 2002. Evaluation of three techniques for detection of low-level methicillin-resistant Staphylococcus aureus (MRSA): a disk diffusion method with cefoxitin and moxalactam, the Vitek 2 System, and the MRSA-screen latex agglutination test. J. Clin. Microbiol. 40: 2766-2771.
- Jayaratne, P., and C. Rutherford. 1999. Detection of methicillin-resistant Staphylococcus aureus (MRSA) from growth on mannitol salt oxacillin agar using PCR for nosocomial surveillance. Diagn. Microbiol. Infect. Dis. 35: 13-18.
- Perry, J. D., A. Davies, L. A. Butterworth, A. L. J. Hopley, A. Nicholson, and F. K. Gould. 2004. Development and evaluation of a chromogenic agar medium for methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 42: 4519-4523.
- Perry, P. L., G. W. Coombs, J. D. Boehm, and J. W. Pearman. 1998. A rapid (20h) solid screening medium for detecting methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 40: 67-72.
- Skov, R., R. Smyth, M. Clausen, A. R. Larsen, N. Frimodt-Möller, B. Olsson-Liljequist, and G. Kahlmeter. 2003. Evaluation of a cefoxitin 30 μg disc on IsoSensitest agar for detection of methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 52: 204-207.
- Skov, R., R. Smyth, A. R. Larsen, N. Frimodt-Möller, and G. Kahlmeter. 2005. Evaluation of cefoxitin 5 and 10 μg discs for the detection of methicillin resistance in staphylococci. J. Antimicrob. Chemother. 55: 157-161.
- Smyth, R. W., G. Kahlmeter, B. Olsson Liljequist, and B. Hoffman. 2001. Methods for identifying methicillin resistance in Staphylococcus aureus. J. Hosp. Infect. 48: 103-107.
- Wertheim, H., H. A. Verbrugh, C. van Pelt, P. de Man, A. van Belkum, and M. C. Vos. 2001. Improved detection of methicillin-resistant Staphylococcus aureus using phenyl mannitol broth containing aztreonam and ceftizoxime. J. Clin. Microbiol. 39: 2660-2662.
- Kim, C. (2012). Properties of a novel PBP2A protein homolog from Staphylococcus aureus strain LGA251 and its contribution to the beta-lactam-resistant phenotype. J. Biol. Chem. 287: 36854–36863.
- Skov, R. (2013). Phenotypic detection of mecC-MRSA: cefoxitin is more reliable than oxacillin. J. Antimicrob. Chemother. 68: 2949–2950.
- Cartwright, E. J. P. (2013). Use of Vitek 2 antimicrobial susceptibility profile to identify mecC in methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 51: 2732–2734.
- Cuny, C. (2011). Rare occurrence of methicillin-resistant Staphylococcus aureus CC130 with a novel mecA homologue in humans in Germany. PLoS ONE. 6: e24360.
- Anna-Kaarina, J., Sanna Laakso, P., Anne sAittakorpi, M., Lindfors, L., Huopaniemi, H. and Minna, M. (2009). Rapid identification of bacterial pathogens using a PCR- and microarray-based assay. BMC Microbiology 9: 161.
- Bignardi, G. E., Woodford, N., Chapman, A., Johnson, A. P. and Speller, D. C. E. (1996). Detection of the mec-A gene and pbenotypic detection of resistance In Staphylococcus aureus isolates with border ine or low-level methicillin Resistance. Journal of Antimicrobial Chemotherapy 37: 53—63.
- Cavassini, M. A., Wenger, K., Jaton, D. S., Blane, and J. Bille. (1999). Evaluation of MRSA Screen, a simple an t i-PBP-2a slide latex agglutination kit, for rapid detection of methicillin resistance in Staphylococcus aureus. J ournal of Clinical Microbiol ogy.37: 1591-1594.
- Perez, R. E., Claverie, M. F., Villar, J. and Méndez, Á. (2001). Multiplex PCR for Simultaneous Identification of Staphylococcus aureus and Detection of Methicillin and Mupirocin Resistance. Journal of Clinical Microbiology. 39 (11): 4037-4041.
- Tiemersma, E. W., Brozwaer, S. L., Lyytikainen, O., Degener, J. E., Schrijnemakers. P., Bruinsma, N., Monen, J., Witte, W. and Grundman, H. (2004). Methicillin-resistant Staphylococcus aureusin Europe. 1999-2002. EmergingInfectious Dis eases.10: 1627-1634.



