The Chemical Approach of Methotrexate Targeting
Loay Abdulrahman1, *, Oladapo Bakare1, Maiada Abdulrahman2
1Chemistry Department, Howard University, Washington DC, USA
2Department of Health, Stratford University, Alexandria, USA
Abstract
"Cancer is the second most deadly disease that kills half a million Americans each year, the first being heart diseases. National Center for health statistics from the year 2009 shows that as many as 1,555 people die each day of some cancer" [1]. Around the world the discovery and development of anticancer agent become the key focus of several pharmaceutical companies and organizations which invested in prevention, diagnosis, and treatment of this disease. Methotrexate (MTX) has used for many years in the treatment of patients with cancer as a cytotoxic agent and as an anti-inflammatory drug for the treatment of inflammatory diseases, such as rheumatoid arthritis (RA). The objective of this article is to produce an update and review the amount of effort in developing a new candidate of this clinically used the drug to minimize the side effect and enhance the therapeutic index. Researchers have linked MTX to various polymeric drug carriers. Coupled MTX led to the incorporation of medication with different modes of toxicity towards the healthy tissue. Proposal for the new candidate of this new drug suggested, with high precision and low advers effect, the scientists say, the conjugates could make cancer drugs already on the market more efficient and give new life to cancer drugs that shelved for being too toxic.
Keywords
Methotrexate, PEGylated MTX, Dendrimer, Polysaccharide, Nanoparticles, Carbon Based Nanotubes, Nanocage Protein
Received: October 27, 2016
Accepted: November 10, 2016
Published online: January 9, 2017
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Background
Cancer is a disease of abnormal and uncontrolled cell growth. Cells grow by replicating themselves and dividing. Mutations occur during DNA replication and cell division. As cancer progresses, the tumor makeup becomes a more heterogeneous mix; due to the result of mutations. The new-found variety makes treatment more difficult if resistant lines have developed in the changing mosaic of cells.
Dihydrofolate reductase DHFR a medium sized enzyme is an essential for the biosynthesis of DNA and cellular replication, with a molecular weight of 20,000. It has used as a target for antineoplastic, antiprotozoal, antifungal, and antimicrobial [2]. It found in all eukaryotic and prokaryotic organisms, DHFR catalyzes the transfer of a hydride from NADPH to dihydrofolate with an associated protonation to produce tetrahydrofolate [3]. The classical dihydrofolate inhibitor having structural similarity with folic acid are MTX (figure 1) and its polyglutamate, inhibit the DHFR enzyme and restricts the growth of cell or DNA synthesis, causes cell death.
The shortcomings observed with MTX, namely, the systemic toxicity and cell non-specificity, led to the development of various strategies. First, the search for analogs, structural modification of MTX was reported aiming to create new agents with altered therapeutic efforts [4]. For example, an amendment on the glutamate side by using different amino acid analogs or preparing polyglutamate. Two isomers may produced due to the two reactive carboxylic acid; researchers found that the relative reactivity of the γ-isomers is 2.3 times higher than α-isomers [5], while others reported that the α-derivatization of MTX to be more important than the γ- derivatives with respect to the internalization of MTX [6].
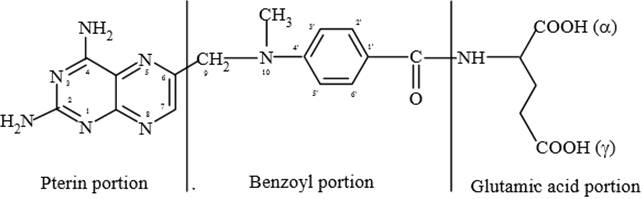
Figure 1. Methotrexate.
The currently licensed new candidate antifolate drugs for therapeutic use despite being nephrotoxic
"Raltitraxed" [7] (figure 2), represents the modification occurred on the p-amino benzoic acid moiety (PABA). Several analogs reported] [8-10] based on the structural activity relationship of pteridine ring in consideration the nature and the length of the bridge between the pteridin ring and PABA. For example the recently reported pemetrexate (figure 3) approved for treatment of malignant pleural mesothelioma [11].
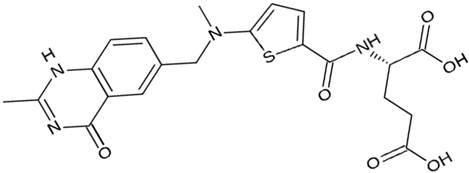
Figure 2. Raltitraxed.
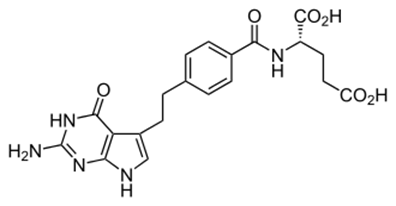
Figure 3. Pemetrexate.
The second strategy, in an attempt to improve the therapeutic profile, combination therapy were employed based on the application of several principles: biochemical synergy, the tumor cell kinetics, the non-overlapping toxicity, the increase of fractional cell kill, and the non-cross resistant agents (tumor cell resistant) [12]. The combination therapy refers to either the simultaneous administration of two or more pharmacologically active agents, for example, anthracycline combined with adrinamycin and cyclophosphamide or leucovorin and 5-fluorouracil [13] or using two unlike types of therapy like chemotherapy and radiotherapy [14]. Unlike single agent therapy, multi-agent therapy can modulate different signaling pathways in diseased cells, maximizing the therapeutic effect and possibly, overcoming mechanisms of resistance.
The third strategy concerned with the delivery of a single and / or multiple therapeutic agent using polymer-drug conjugate. The later act as a transport parameter to allow the development of ultra-specific targeted macromolecular drugs. These macromolecular drugs have the advantage of increasing the potency while simultaneously reducing resistance to therapy and toxic effects of current anticancer drugs [15, 16]. This review summarizes the main conjugated polymer that added a unique value when conjugated to MTX. Consequently, the right linkage strategy still a challenge and depends on strongly a suitable polymer, which discussed in the following section.
2. Case Studies
2.1. MTX Conjugated Polyethylene Glycol (PEGylated MTX)
Polyethylene glycol (PEG) is the most used polymer in drug discovery, the reasons for its success reside in many advantageous properties, such as its hydrophilicity, non-toxicity, and non-immunogenicity. The approval of PEG use in humans by Food and Drug Administration marked the beginning of its safe use in clinical practice. Consideration of PEG as the first choice was continued to improve the biocompatibility, half-life and safety of proteins, nanoparticles, liposomes, micelles and other drug delivery systems, a view that has been supported by some of studies confirming that it has limited toxicity in animals and humans [17].
The process of attaching a PEG chain to a protein has become a well-established technology for the use of proteins as drugs, especially as anti-cancer agents [18, 19]. The successful clinical use of PEGylated macromolecular drug has promoted the application of this technology to develop an architecture in H-shape with four arms PEG conjugated system forming biodegradable polymeric micelles (figure 4). MTX linked to bond end PEG central via disulfide linkers was prepared in two ways ester and/or amide using equimolar (1:1) drug–polymer conjugates and the characterization methods including UV, IR, NMR, DSC and GPC were successfully used to determine the physical and chemical properties of the produced conjugates. The conjugates studied for drug delivery to the site of the tumor as they possess thermodynamics, stability, and ability to encapsulate and solubilize a hydrophobic guest molecule, biodegradability, as well as the size and surface characteristics that facilitate rapid clearance by the reticuloendothelial system.
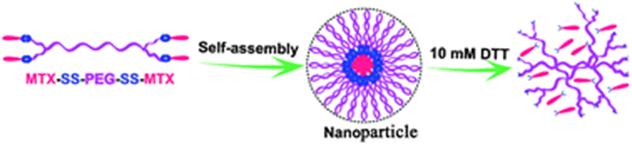
Figure 4. The process of attaching a PEG chain to a protein.
The cleavable disulfide linkers allow the conjugated MTX to exert its therapeutic activity because of the fast cleavage of disulfide linkers when exposed to the intracellular concentration of glutathione (GSH) [20]. Riebeseel and coworker’s synthesized a series of MTX-PEG conjugate with a molecular weight ranging from MW750 to 40,000 (figure 5) [21, 22]. Another group of research indicated that the rate of drug release from amide derivative was slower than ester derivative [23], and both derivatives alter the hydrophobicity of the conjugate.
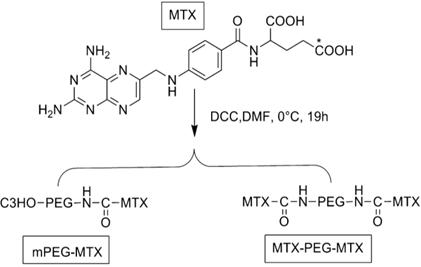
Figure 5. MTX-PEG conjugate.
The results indicated the additional release of MTX from polymer to obtain sufficient interaction with active DHFR, and in vitro, the IC50 increased with the increased size of the drug-polymer conjugate. Other workers explored the validity of using MTX playing an early-phase cancer-specific targeting ligand assisted with a late-phase therapeutic anticancer agent based on the PEGylated chitosan (CS) nanoparticles (NPs) as drug carriers. The nanoparticles surfaces indicated two or more distinct physical properties and allow two types of chemical reaction to occur at once (Janus-like agent), The (MTX + PEG)-CS-NPs (figure 6). The PEGylated chitosan and (NPs) represent the nanoparticles which can ensure the minimal premature release of MTX at off-target site to reduce the side effects to healthy tissue; also NPs can operate as a prodrug formulation, releasing biologically active MTX inside the cells. The conjugate showed a greater cellular uptake and demonstrated a superior cytotoxicity compare to the free MTX [24].
Multi-walled carbon nanotubes (MWCNT) as a carrier reacted with PEG-MTX to produce nanoconjugate of the similar formula MWCNT-mPEG-MTX, which show the faster release of drug in the acidic medium than neutral PH. However, in both neutral and acidic media, the release was continuous over the period of 48 hours [25].
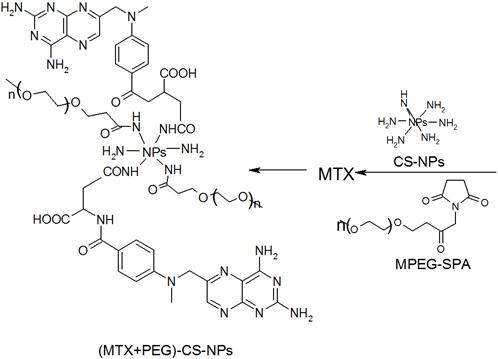
Figure 6. Synthesis of (MTX + PEG)-CS-NPs.
Clinically, a series of the different molecular weight of PEG synthesized by choosing folic acid as targeting prodrug and marketed as Gemcitabine (dfdc) (figure 7), which used in the treatment of solid tumors and small-cell lung cancer, pancreatic cancer. The prodrug suffers from defects such as short plasma half-life, rapid metabolism and low selectivity toward tumor tissue [26].
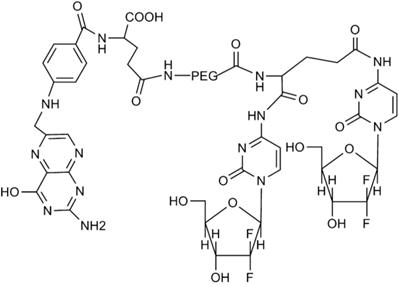
Figure 7. Gemcitabine.
2.2. MTX Conjugate Dendrimer
The design strategies of drug delivery system is a vital aspect often based on interdisciplinary approaches that combine polymer science, molecular biology, and pharmaceutics to improve the therapeutic properties of drugs need to reach the target site at the right time. Dendrimer (a spherical hyperbranched polymer molecules) designs (figure 8) [27], which share several characteristic with protein due to the similarities in their 3D structure, were reported to physically entrapped drug molecules by covalent bond formation [28-31]. Two methods of dendrimer drug delivery reported, the first was encapsulation depending on the exterior interaction of dendrimer and drug. The second was the conjugate formation with the drug [32-34].
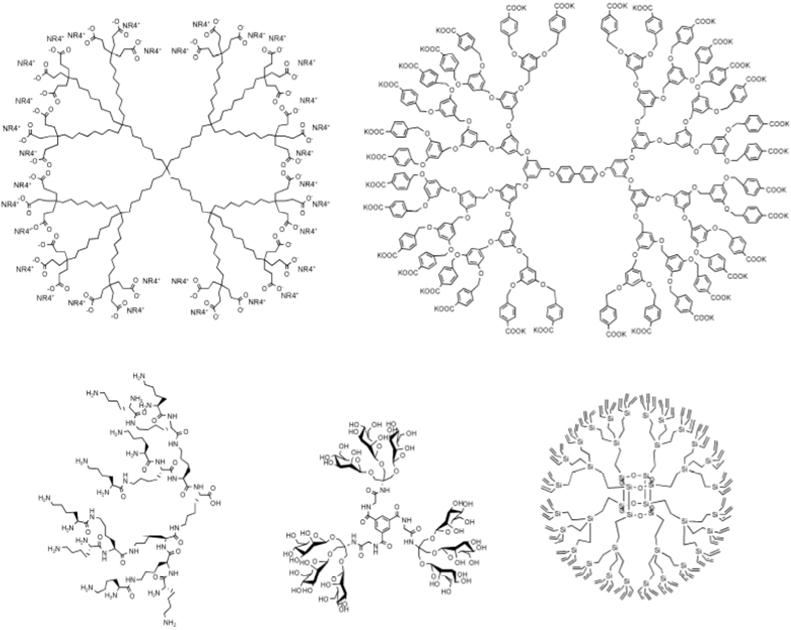
Figure 8. Types of the dendrimer.
Surface modification of dendrimers with functional groups can markedly influence the activity, at present, probably the best-known dendritic system is the commercially available polyamidoamine (PAMAM) [35]. Conjugation of MTX with G5= PAMAM or PLA (polylactic acid) (figure 9) revealed G5-MTX and with G5-FA to give the corresponding structure G5-FA-MTX. The polycationic character of the conjugated structure improved the drug forms by increasing therapeutic effect, alteration of a toxicity profile, selective targeting of a therapeutic agent to tissue of interest, and resistant to degradation in the body [36-39]. The incorporation of the drug conjugates into the tumor cells was confirmed by confocal microscopy [40].
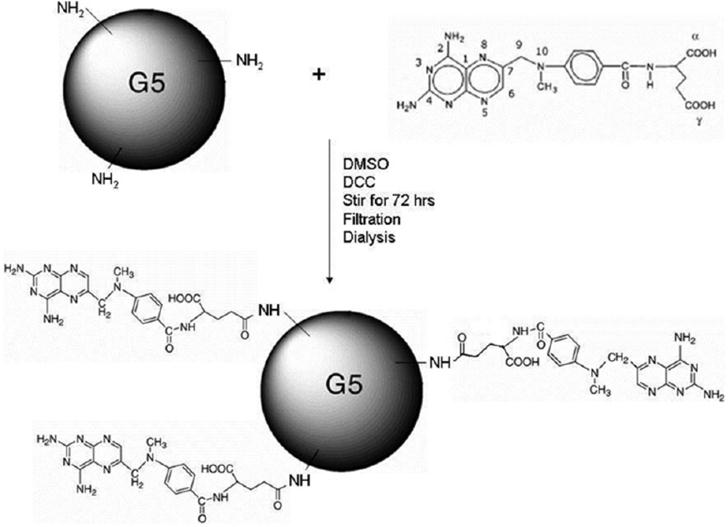
Figure 9. MTX- polyamidoamine (PAMAM) conjugate.
In a novel, simple, feasible for large scale, and reproducible one pot approach, a conjugate of (PAMAM) dendrimer, methotrexate (MTX), and folic acid (FA), has been successfully synthesized [41]. Cytotoxicity screens performed, tests conducted against HeLa human cervica lcarcinoma cell line treated to be drug-sensitive, and against two variants of the rather refractory Colo 320DM, a human colon adenocarcinoma line [42] and uterine sarcoma cell line [43].
MTX conjugated to poly (l-lactic acid) (PLLA) microspheres using the solvent evaporation method. The method characterized in terms of molecular weight, size, thermal properties, and release rates into phosphate buffered saline (PBS) (pH 7.4) at 37°C [44] in an attempt to treat rheumatoid arthritis (RA).
Promising preliminary studies [45, 46] were investigated the condensation of MTX with the poly aryl ether dendrimers, a novel family of multivalent drug carriers was the primary goal.
2.3. MTX Conjugate Polysaccharide
In contrast to many synthetic polymers, polysaccharides have very low (if any) toxicity levels[47-50]. Dependent upon the nature of the monosaccharide unit, polysaccharides can have a linear or branched architecture. In addition to structural diversity, polysaccharides have a number of reactive groups, including hydroxyl, amino, and carboxylic acid groups (figure 10), indicating the possibility for extremely amenable to chemical modification [51, 60]. Moreover, varying of its molecular weight increased their diversity [52]. Also owing to their natural presence within the body, most polysaccharides are subject to enzymatic degradation.
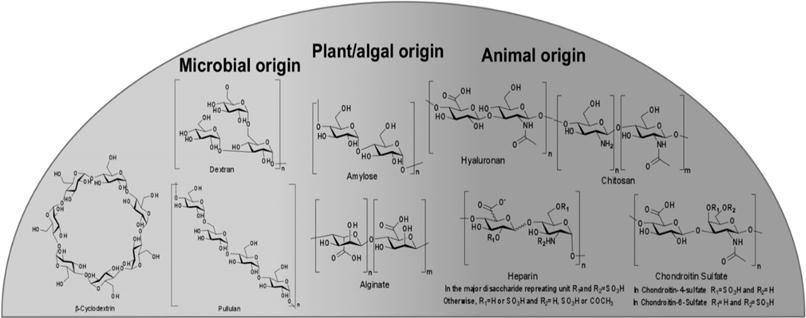
Figure 10. Carbohydrate types and origin.
Dextrans are glucose polymers, soluble in water, neutral in their native form [53] were conjugated to MTX by either direct attachment or through a carrier linked with molecular weights ranging from 10 kDa to 500 kDa [54] to increase the longevity of therapeutic agents in the circulation and reduce their immunogenicity.
The in vitro studies revealed that D-MTX conjugates (figure 11) [54] had 4- to 10-fold lower antiproliferative effects against neoplastic cell lines compared to free MTX. The toxicity of the conjugates was greater in comparison with the parent drug, and the molecular size is of pivotal importance for pharmacological property [55].
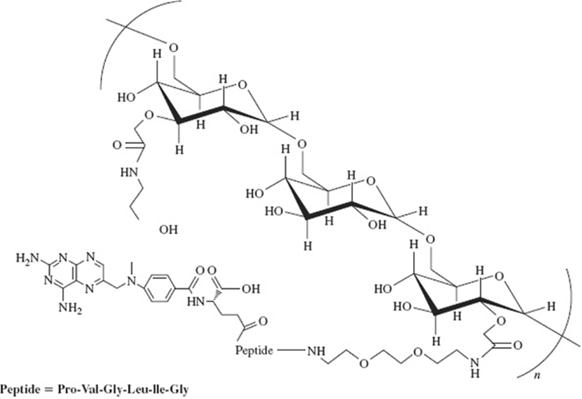
Figure 11. Dextran-MTX conjugate.
Dextran conjugation was characterized by: (i) the good retention of protein activity even for insulin or antibodies proteins requiring interaction with others proteins to perform their biological functions; (ii) pharmacokinetics dependent on dextran’s MW; and (iii) the ability to reduce the immunogenicity of heterologous proteins.
Different cancer cell line were used to determine in the biological activity of MTX conjugate to hydroxyethyl starch (HES) [59] in vitro and in vivo to give the low molecular conjugate HES-MTX with a major limitations such as fast metabolism and excretion from the body, unprofitable biodistribution and low selectivity, and unfavorable uptake by healthy tissue. The compounds characterized in term of MTX content, hydrodynamic size, zeta potential, and drug release kinetics.
In vitro, the biological activity determined using cancer cell and CDFI mice intraperitoneally inoculated with P388 murine leukemia cells. In vivo, the experiment revealed the significant higher antitumor efficacy of HES-MTX conjugate in comparison with the unconjugated MTX.
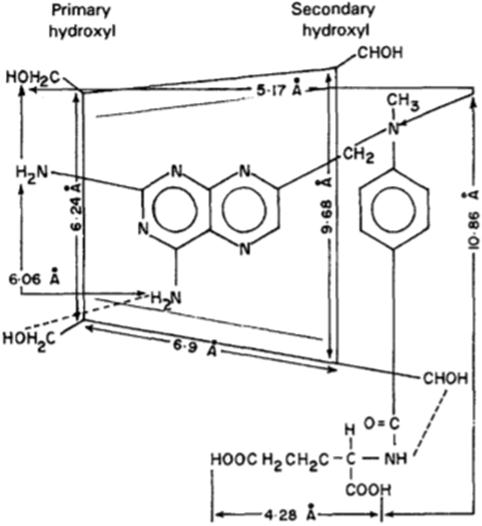
Figure 12. MTX-CyD molecular model.
A proposed configuration of molecular model for MTX conjugate to β-cyclodextrin (CyD) published (figure 12) [60] applying neutralization method. The amino group of MTX interacted with the hydroxyl function of β-CyD on complexation. The complex showed better bioavailability and antitumor efficacy than MTX.
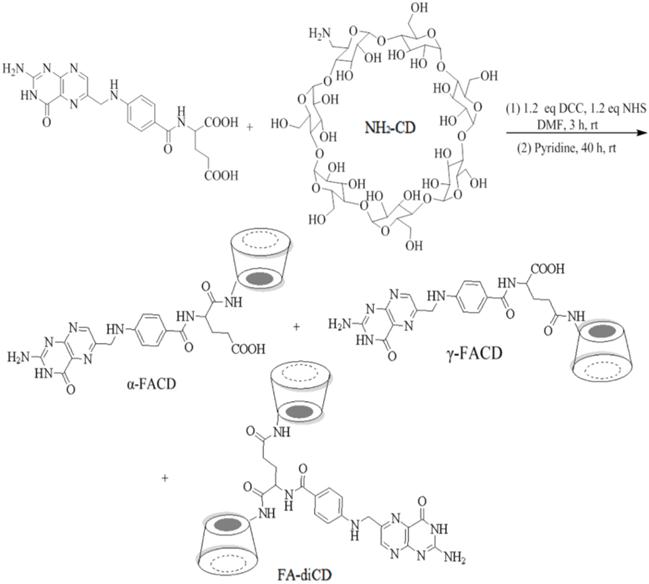
Figure 13. FA- CyD structure.
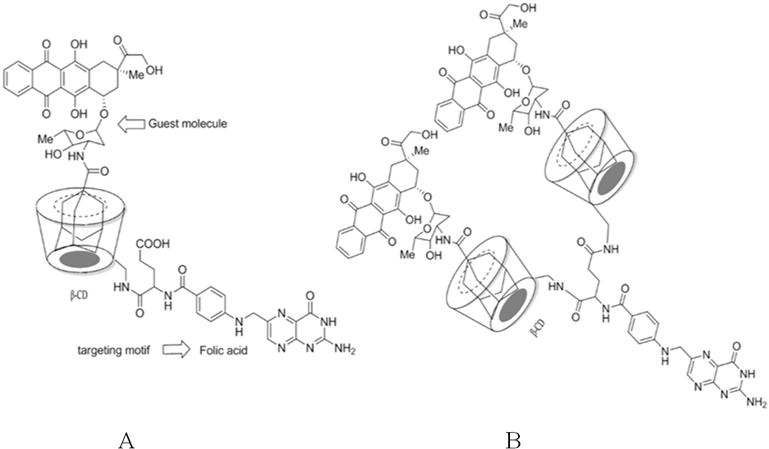
Figure 14. FA-CD-Ada-Dox (a) FA-diCD-Ada-Dox (b) structures.
The novel and effective complex of folic acid (FA) with β-cyclodextrin (CyD) (figure 13), also conjugation of the cytotoxic agent adamentyl doxorubicin (Ada-Dox) into a complex with mono or di-β-cyclodextrin-FA (figure 14) were synthesized by the multistep reaction. The complexes showed an increase in stability of the conjugate in circulation and ensured cleavability to release the drug [61].
The simple linear structure of repeating disaccharide units composed of D- glucuronic acid and N-acetyl-D-glucosamine (hyaluronic acid, HA) conjugated to MTX by the esterification reaction in the presences of dicyclohexyldiimide DCC and DMCP [62] (figure 15A). Homma and co-workers reported the synthesis of HA-MTX in an attempt of coupling MTX first with lysosomal enzyme-sensitive peptide Asn-Phe-Phe, and Gly-Phe-Leu-Gly as linker. The MTX- linker coupled to HA as a spacer [63] (figure 15B), their biological activity showed a tendency to inhibit knee swelling depending on the peptide sequence [64].
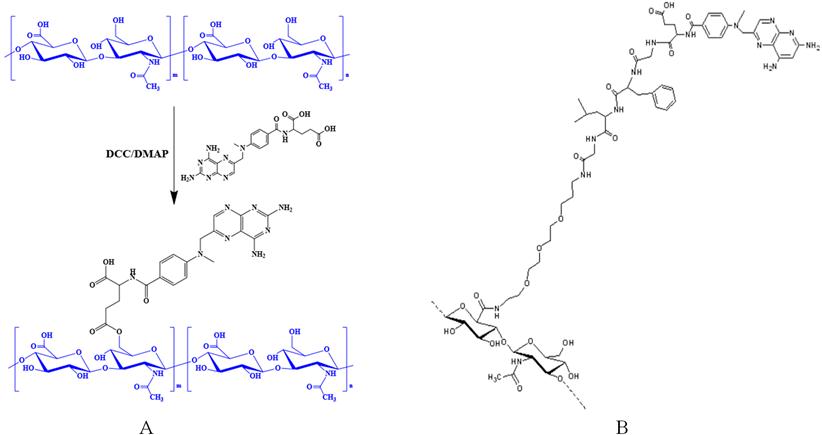
Figure 15. MTX conjugate to hyaluronic acid.
A serologically similar to structures found on a mammalian glycoprotein, a linear polymer of the sugar mannose (plant polysaccharide) used as a homing device to direct the drug into macrophages. Mannose is recognized by mannose receptor and internalized into cells giving the reason to be used for targeted delivery. MTX conjugated to mannose to give Mann-MTX which show significant improve antitumor activity of leukemia compared to free MTX [65].
2.4. MTX Conjugate Lipid
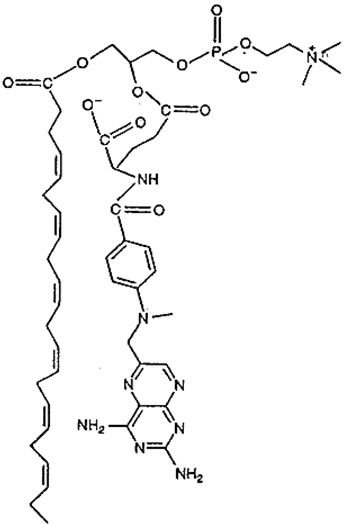
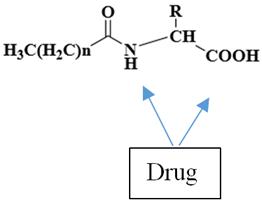
Figure 16. MTX-lipids.
Lipid nanoparticles have a higher degree of biocompatibility and versatility; they are commercially viable to formulate pharmaceuticals for topical, oral, pulmonary or parenteral delivery. Lipids used for the production of nanoparticles may be arranged into two: bilayer and non-bilayer lipids, their function either increase passive diffusion across epithelial barriers or can increase uptake into the lymphatic system [64].
MTX conjugated to the Tris-lipidation via glycine linker and mono-, di-, and tri- palmitate esters to give Lipophilic (MTX)-lipoamino acid, synthesis took place with amide or ester (figure 16) [66], The inhibitory activity of the conjugates was assessed using MTX-sensitive human lymphoblastoid CCRF-CEM cells and an MTX-resistant sub-line (CEM/MTX). The alpha, gamma, or alpha, gamma amide conjugates showed different activity in inhibiting the growth of parent cells. CEM/MTX cells were much less susceptible than CCRF-CEM cells to inhibition by alpha or alpha, gamma-substituted lipoamino acid conjugates, whereas both cell lines were almost equally sensitive to the MTX-gamma conjugates [67].
A single-step approach with a strategy of generating microbubbles from a mixture of CO2, a small amount of gases having low solubility in water, exist in an aqueous solution of protein, a polysaccharides and anionic lipid-based nanoparticle (LNPs) [68] (figure 17), have been developed as drug carriers for the noninvasive and brain-targeted delivery of therapeutics, and in vivo imaging in a constructed structure. Their application for diagnostic imaging are known as theranostic nanoparticles (TNPs) is limited by their low drug-loading capacity [69]. Avoiding the high systemic doses, which cause severe long-term neurotoxicity, or intrathecal administration, which is highly obtrusive and may lead to infections or hemorrhagic complications, MTX-liposome-coupled microbubbles had a high drug-loading capacity of 8.91%±0.86%, and their size (2.64±0.93 µm in diameter) was suitable for intravenous injection. When used with ultrasound, they showed more potent in vitro cytotoxicity against Walker-256 cancer cells than MTX alone or MTX-loaded liposomes.
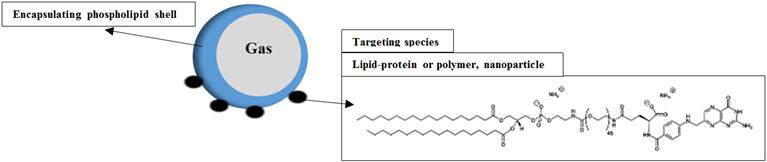
Figure 17. MTX-microbubbles conjugate.
2.5. MTX Conjugate Antibody
The antibody directed enzyme prodrug therapy (ADEPT) is a new class of drugs designed as a targeted therapy for the treatment of cancer, it has attracted considerable interest since the concept first described in 1987. Antibody drug conjugate ADC building block consist of three component as shown in (figure 18).
The ideal mechanism of action of ADC is their binding to a cell-surface antigen, followed by the endocytic internalization of the conjugates and then the release of the drugs or their biologically active low molecular weight derivatives from the conjugates in the endosomes or secondary lysosomes.
Different derivatives approaches have been developed based on a covalent linkage. Various classes of crosslinking reagents have been synthesized, with the aim of improving the characteristics of the conjugates [70]. The linker must attach to the monoclonal antibody without affecting antibody-antigen binding function, and to the drug in a way that enables efficient release from the antibody only after internalization in the target cell. Chemical conjugation takes place between drug-linker and antibody is either with lysine or thiol groups on an antibody [70]. It has reported that conjugation of the drug limited by the peptide sequence of the antibody, which therefore restricts control over the number and position of attached cytotoxic drugs, this will play a significant role in the toxicity, stability and potency of ADC. One important point to take into account is that the linkage method must be selected so as to avoid both the formation of homopolymers of antibody or agent and aggregation of the conjugate [71].
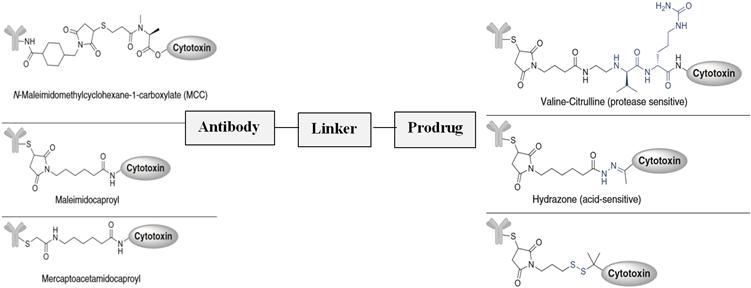
Figure 18. The building block component of MTX-antibody conjugate.
MTX conjugated to a monoclonal antibody via different active cleavable and non-cleavable linker intermediates, albumin [68], GSH [70], maleinmidocaproyl [72] prepared by either the carbodiimide or the active ester method. Antibody-MTX conjugate was revealed to be as effective as a free drug in causing cell death and a significant reduction in tumor growth rates [73, 74], and reported to be 100-1000 times more potent than conventional chemotherapeutics and preferably have sub-Nano-molar potency [75].
2.6. MTX Conjugate Gadolinium Texaphyrin
Texaphyrin, the pentaza shiff’s -base expanded porphyrins were first reported in late 1980’s (figure 19). Texaphyrin was formed stable complex with metal ion gadolinium; the complex conjugated to MTX in an attempt to overcome tumor resistance and lower MTX uptake.
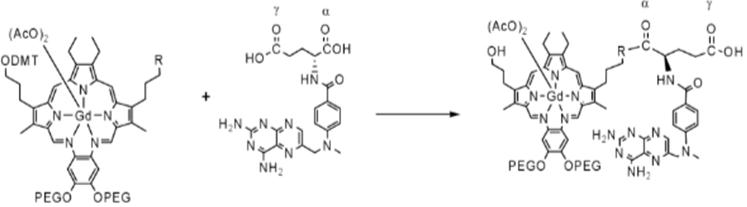
Figure 19. MTX conjugate Gadolinium texaphyrin.
The conjugate was prepared by three ways, 1-the amide preparation, 2-direct mediated coupling, 3- via an intermediate linker PEG. In all cases α, γ-isomers was obtained during the coupling and esterification steps of MTX [76]. The other avenue of these complex, they play a tumor selective radiation sensitizer and demonstrate contrast agent for localization in MRI [77].
2.7. MTX Conjugate Carbon Based Nanotubes
These new carbon allotropes raised high interest in the artificial world due to their unique structural and electronic properties [78], they showed strong antioxidant and are characterized as "radical sponges." Their biomedicinal application has achieved significant progress. They demonstrated a great capacity to penetrate into cell, large surface area, there are some reactive functional groups on its basal plane and edges, such as hydroxyl, epoxide and carboxylic acid, which could be modified or conjugated with polymers to improve its solubility and biocompatibility [79]. Different nano carbon (figure 20) such as carbon nanotubes CNT, graphene, fullerene, nanodiamond and carbon nanoparticles (CNPs) have developed as delivery vehicles for imaging and therapeutic agents [80]. These nanoparticles generally composed of an inner core with encapsulated therapeutic agents surrounded by hydrophilic, detachable shell [81]. The detachable process take place at a specific manner dependent on the linker between outer shell and inner core. The linker can be acid-, redox- and enzyme- cleavable according to the aim of the design or condition of the delivery process [82].
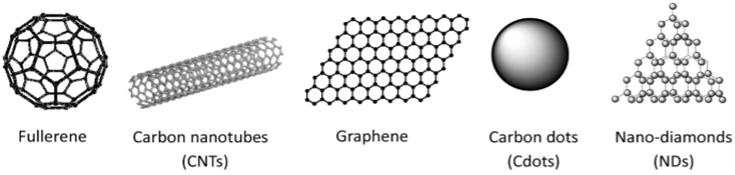
Figure 20. Types of Carbon based nanotubes.
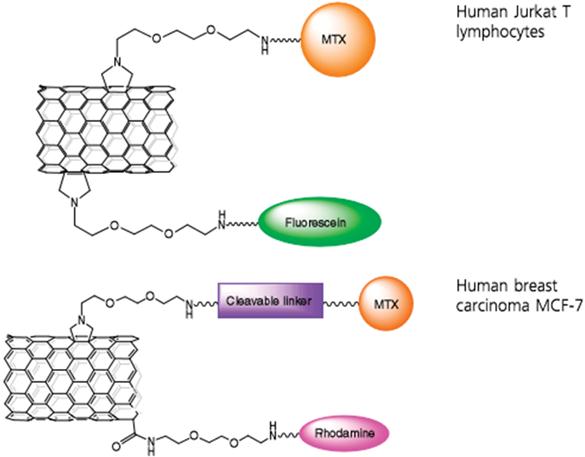
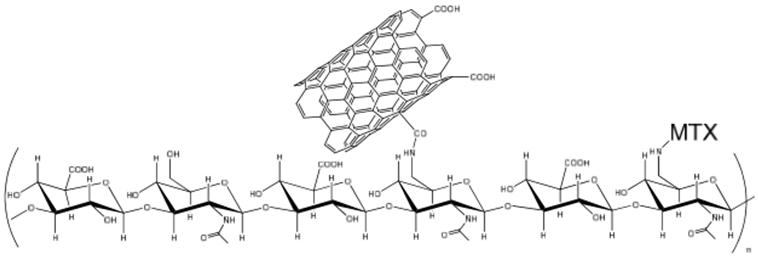
Figure 21. MTX – MWCNTs.
MTX covalently coupled to nanomaterials consisting of quantum dots QDs; the biological activity studies was taken up effectively by HeLa cells and shown to have a dose-dependent antiproliferative effect in cancer cells [83]. Other workers evaluated their internalization and cytotoxicity in the KB cells with/without resistance to MTX based on the photoluminescence (PL) properties of QDs [84].
MTX - MWCNTs (multi-walled carbon nanotubes, MWCNTs) prepared via different linkers (figure 21) [85-88], including functional groups sensitive to intracellular enzymes. The stable amide bond between the MTX and the tubes could be the reason for the lack of enhanced efficacy, releasing the drug too slowly from CNT into the cytoplasm. The cytotoxic activity of the MTX--MWCNT conjugates was strongly dependent on the type of linker; indeed, MTX grafted via a tetrapeptide presented the highest activity.
Fullerene derivatives, the 20 hexagonal and 12 pentagonal rings, in which every carbon atom was sp2 hybridized and bonded to three other carbons act as antioxidant, were employed to enhance the therapeutic efficacy of a lipophilic slow-release drug delivery system [89].
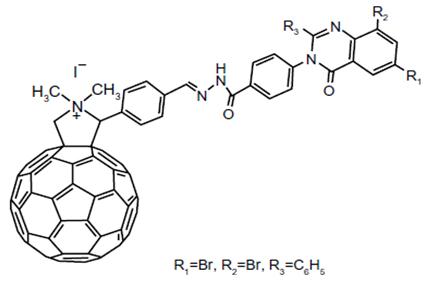
Figure 22. The structure of MTX analog conjugate graphene oxide (GO).
Graphene, a single layer of carbon atoms arranged in a honeycomb lattice, its derivatives such as graphene oxide (GO) (figure 22), reduced graphene oxide (RGO) and GO-nanocomposites have widely used as novel nanocarriers for drug and gene delivery, due to their peerless physical and chemical properties. Single-layered graphene’s show ultra-high surface area is available for efficient molecular loading and bioconjugation. Graphene’s conjugate demonstrated to serve both as a drug carrier for controlled drug delivery and as a contrast improvement agent in magnetic resonance imaging, targeted at cancer diagnostics and therapeutics. In an attempt to study the interaction between graphene and drug molecules, and the effects of surface functionalization, focusing on the various sizes of graphene sheets as well as the types, numbers, and loading modes of drugs. Graphene-MTX complex models showed that the limited sizes of graphene sheets restrict the movement of drug molecules. Multiple drug molecules may form bunch that slow down the diffusion on graphene sheets [90]. Antineoplastic action of MTX-GO and empty graphene oxide against human breast adenocarcinoma cell line MCF7 reported [91].
2.8. MTX Conjugate Nanocage Protein
Over the past decade, nanocages have played a vital role in the development and implementation of many useful tools for studies involving biology, chemistry, and material sciences as well as nanomedicine. Its applications including drug delivery, due to their high surface/volume ratio, surface tolerability, multi-functionality and intrinsic properties. Its advantages concern with their ability to minimize premature drug degradation or interaction with its biological environment and to transport cargo to specific tissues, their versatility for incorporation of new and/or multi-functional moieties at a uniform and precise loci and with desired density by simple chemical and genetic modification. Thus, indicated the versatility of nanocages as well as diversity and accuracy in modification and functionalization. Many protein nanocage based applications in drug delivery are actively pursued not only in the laboratory but also in the preclinical and clinical stages. Caging drugs by protein shells can also circumvent existing resistance as shown in the study of MTX-loaded polyoma virus capsids [92]. Green fluorescent protein GEP and MTX were encapsulated by covalent linkage to a domain of an inner core protein in the lumen of the virus capsids. The caged GEP and MTX internalized into leukemia T cells and MTX-transport resistant cells, allowing the cytostatic effects of MTX to be manifest [93].
The serum iron transport protein transferrin (Tf) has been investigated as a potential drug carrier to allow precise targeting to cancer cells since the transferrin receptor (TfR) overexpressed in a broad range of cancers. Tf conjugates with methotrexate MTX have been reported greater cytotoxicity than MTX conjugates [94, 95].
Albumin is the most abundant protein in plasma, accounting for more than half of human plasma protein. Albumin is essential for various physiological processes such as solubilizing long chain fatty acids, providing colloidal osmotic pressure,, delivery of nutrients to cells, and balancing plasma pH. Albumin has widely studied as a protein carrier for drug delivery. Albumin is biodegradable in nature, non-toxic and nonimmunogenic, stable over a wide pH range. The half-life of albumin is 19 days in blood circulation, act as a carrier in improving the pharmacokinetic property of peptides or protein-based drugs, and small drug molecules, [96].
The rationale for the use
1. Localized inside cells with high protein intake
2. Improve activity due to the interaction of macromolecular attached-drug at the site of action.
A better anti-arthritic effect than MTX reported [97] when methotrexate-albumin conjugate (MTX-HSA) and (MTX prodrug-HAS) [MTXpro=EMC-d-Ala-Phe-Lys-LysMTX] (EMC= 6-maleimidocaproic acid) developed by direct coupling of MTX or its prodrugs to lysine residues of HAS (figure 23). Their therapeutic effects have proved in clinic or preclinical studies [98, 99].
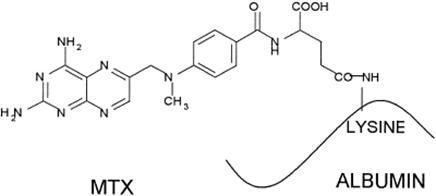
Figure 23. MTX-HSA conjugate.
Reduction by 17.6% of the initial tumor volume, increased the survival of tumor-bearing mice to 47.5 ± 0.71 days and increased their life span up to 216.7% was reported when Biotin molecules conjugated on the surface of MTX-HSA NPs [100].
2.9. MTX Conjugate Layered Double Hydroxide
Layered Double Hydroxides (LDHs) with a general formula M(II)1-x M(III)x (OH)2 (An-)x/n × y H2O (figure 24) are generally minerals located between organic material with a surface layers compose of positively charged brucite type. The layer constructed with mixed metal hydroxides of divalent and trivalent metals with convertable intercalated negatively charged categories in between the two surface layers which offset for the positive charge of the brucite layer. LDH shows overwhelming promise in its function as a controlled drug delivery system due to its ability to introduce drug molecule in its interlayer space and its non-toxicity in living tissues.
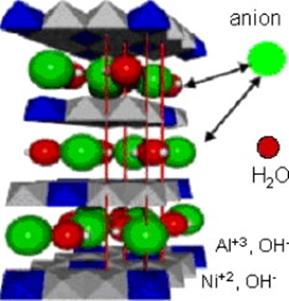
Figure 24. Layered Double Hydroxides.
Manjusha Chakraborty et al [101, 102] synthesized nano-vector for delivery of anticancerous drug containing methotrexate (MTX) in ZnAl-layered double hydroxide (LDH) by anion exchange method. Using thermogravimetric analysis they showed that the thermal stability of the MTX increase when it intercalated in the LDH.
Jae-Min Oh et al [103] intercalated methotrexate (MTX) into MgAl layered double hydroxide by co-precipitation method. The anticancerous activity of MTX-LDH nanoparticles was determined using MTT and BrdU bioassay with the bone cancer cell culture lines (Saos-2 and MG-63) and proved that the anticancerous efficacy of MTX-LDH is much higher than that of pristine LDH.
2.10. Combination of MTX Conjugation
The use of multiple drugs with different cellular targets and different mechanisms of entry into cells allows for effective chemotherapy and high cure rates. In an efforts to develop effective strategies that increase the therapeutic potential of anticancer drugs with less systemic toxicity, are being directed towards the investigation of dietary supplements and other phytotherapeutic agents for their synergistic efficacy in combination with anticancer drugs. The synthesis of two derivatives of methotrexate which are: -Schiff base methotrexate-silibinin conjugate and Methotrexate-silibinin conjugate (figure 25), the anticancer activity were investigated by HEP-2 cell line (Larynx carcinoma), which showed higher activity than methotrexate or silibinin alone [104].
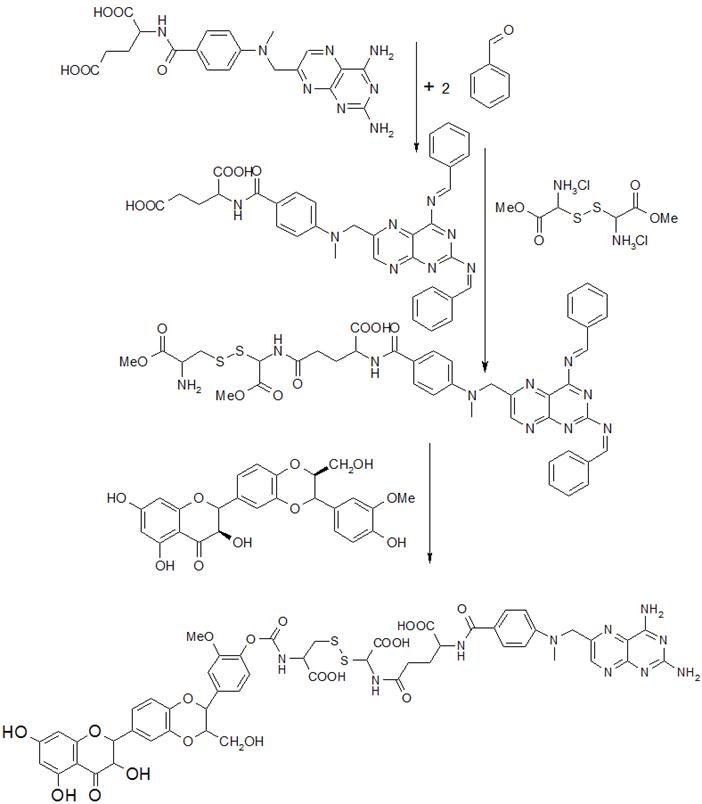
Figure 25. Methotrexate-silibinin conjugate.
A greater applicability of chlorotoxin (CTX), a peptide originally isolated from Leiurus quinquestriatus scorpion venom, demonstrated the targeting specificity for a wide variety of tumors, including prostate cancer, intestinal cancer, and sarcoma. The tumor cell-specific targeting of the NP-MTX-CTX conjugate was synthesized and evaluated in vivo and in-vitro using mice bearing xenograft tumors, poly (ethylene glycol) (PEG) layer was also integrated to serve both as a biocompatible coating and linking molecule for the covalent attachment of the functional ligands to the iron oxide core. NP-MTX-CTX showed enhancement in MRI contrast and demonstrated the ability to inhibit cell growth over the first 12 hrs after treatment [105, 106].
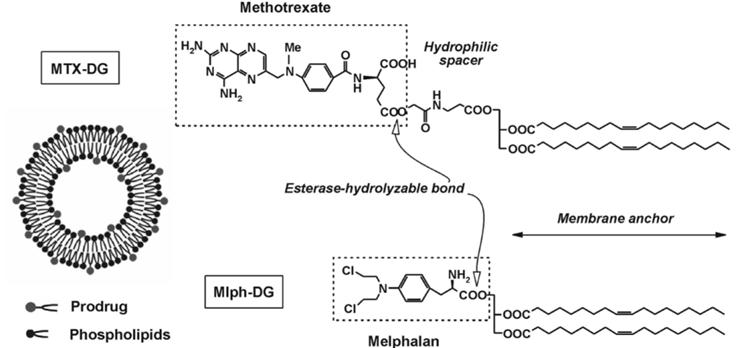
Figure 26. Synthesis of NP-MTX-CTX conjugate.
Radiolabeled conjugate of MTX-melphalan (L-PAM) was synthesized by covalently linked to PEGs and evaluated in vitro against the U87MG human glioma cell line revealed that the conjugates showed enhanced dose-dependent cytotoxicity [107].
A study was conducted to characterize the physicochemical stability of liposomal formulations containing Mlph-DG and MTX-DG, as well as to research into the accessibility of long-term storage liposomal preparations. MTX conjugated to 1,2-dioleoyl glycerol DG to give MTX-DG incorporated into the lipid bilayer of liposomes after it coupled with Phosphatidylcholine (PC) from egg yolk and phosphatidylinositol (PI) to provide PC-PI-MTX-DG [108] (figure 26).
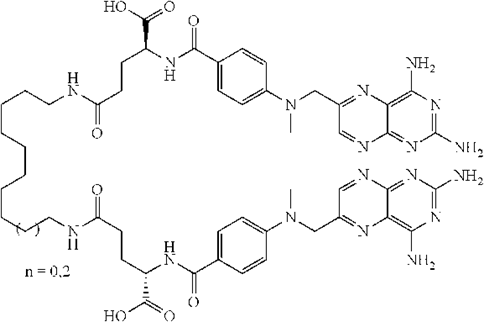
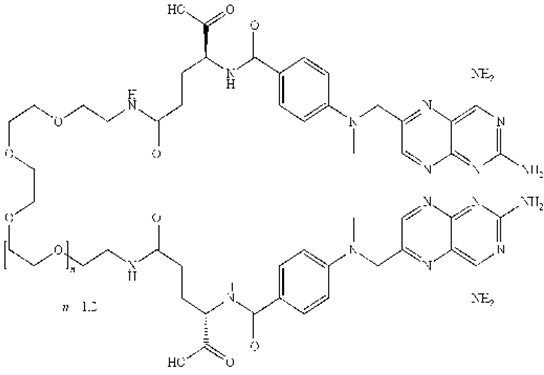
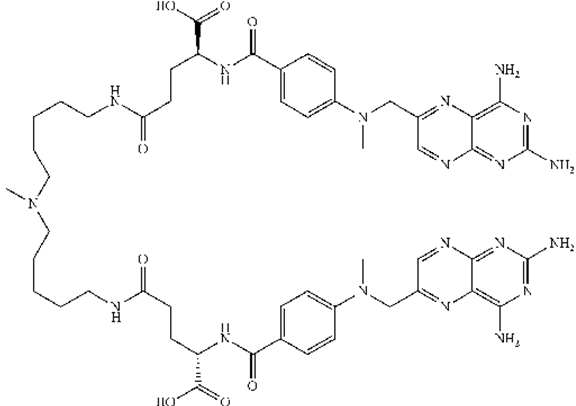
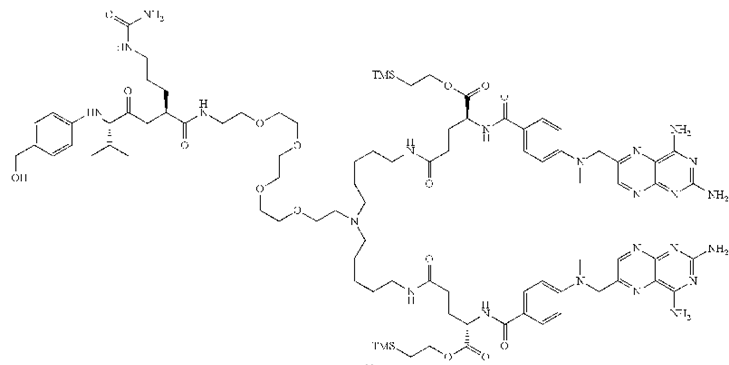
Figure 27. Structures of BisMTX.
MTX was applied as chemically induced dimerization when it conjugated with protein domains to demonstrate a method to regulate signal transduction. BisMTX (figure 27) was synthesized to form highly stable cyclic dimers, trimers, and larger rings from tetramers over octamers with diameters ranging from about 5 to at least 100 nm, in an attempt to create model systems for study of the specific interactions between protein and small-molecule DHFR ligands. The nanoring size is affected by the composition of the peptide linker, and the length, on induced protein-protein interactions, and on the affinity and configuration state of the dimerizer, and. The experiment revealed that BisMTX shows more stability than the binary MTX-DHFR and increase of binding affinity due to the generation of additional protein–protein interactions outside of the ligand-binding sites [109, 110].
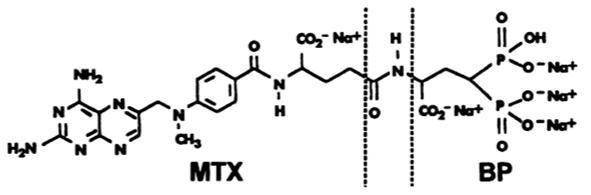
Figure 28. MTX- bisphosphonate conjugate.
A labeled conjugate of MTX- bisphosphonate (figure 28) with 99Tc containing a peptide bond has been found to behave like a bone-seeking agent and to possess more than five times greater antineoplastic activity against osteosarcoma in experimental animal models correlated with methotrexate alone [111].
Insulin was reported to be used as suitable candidate carrier for carcinoma targeted therapy by receptor mediation when covalently linked to MTX with and without linker (figure 29). The minimum inhibitory concentration of the conjugates to inhibit proliferation was similar to or slightly higher than unconjugated methotrexate [112, 113].
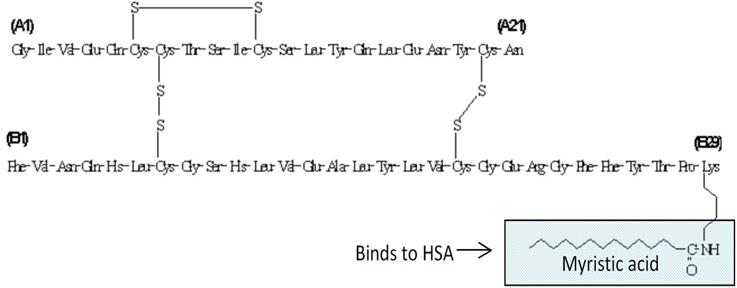
Figure 29. Insulin as a carrier for carcinoma targeted therapy.
Iron magnetic nanoparticles (MNP) were used to combine the two anticancer agents MTX and Doxorubicin DOX using glutaraldehyde activation method (figure 30), the resulted DOX-MNP-MTX confirmed by magnetic nanoparticle linked immunosorbent assay. Sixteen to 22% more killing effect observed in Hela cells [114].
Multidrug delivery system prepared from a random copolymer of polylactic-co-glycolic acid (PLGA) grafted branched polyethyleneimine (BPEI) were conjugated with MTX through the DCC/NHS chemistry to give (PBP-MTX), the later act as nano micelles with entrapped 5- fluorouracil FU through nanoprecipitation technique. Promising action illustrated on colon cancer [115] encouraged researchers to do further invvestigation.
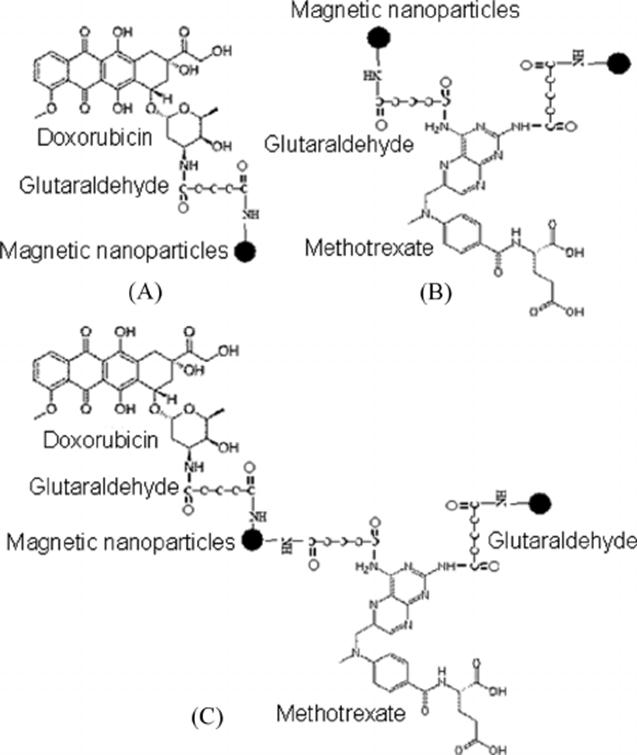
Figure 30. The Doxorubicin-methotrexate molecule.
A method identifying a molecule that bind a known target in a cell was reported by building chemical inducers of protein dimerization in a way that central molecule played as a cleavable linker, could covalently bind to two molecules having two different receptors. Methotrexate conjugate to dexamethasone, cepham, 3,5,3′-triiodothyronine, retinoic acids, and Biotin was synthesized and designed to use a variety of hydrophobic linkers, for example (figure 31 A) Dex-Cepham-MTX, shown that cepham was linked to MTX and work as a central moiety (cleavable linker), and (figure 31C) Dex conjugate to MTX via different linker, while in (figure 31B) cepham used as inducer of protein dimerization capable of selectively binding to penicillin binding protein (PBP) [116-118]. All compounds were screened and determined the capability of cell permeability and inducing protein dimerization in vivo. Also the study indicated that the length of the linker was necessary and has a great impact on permeability.
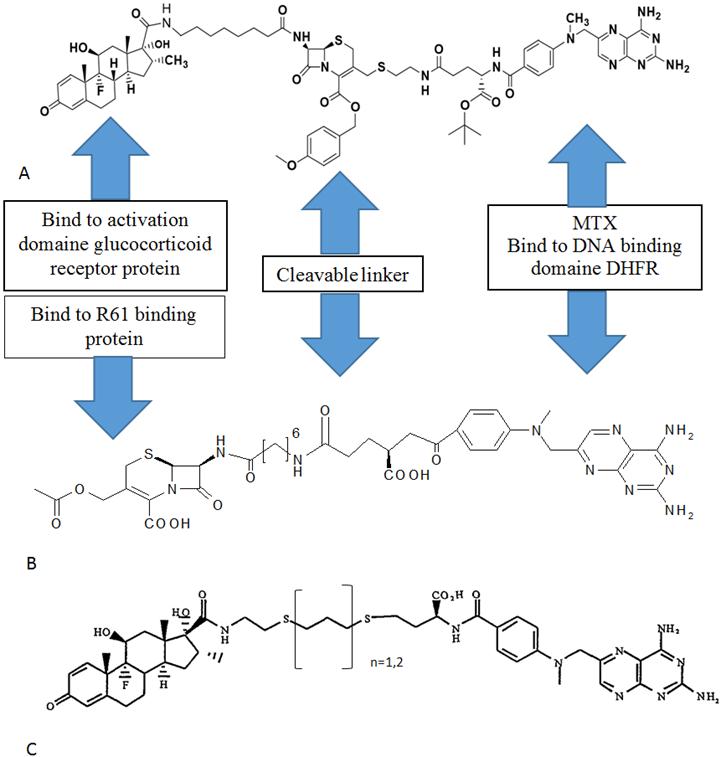
Figure 31. The design of complex compounds that dimerizing two fusion proteins inside a cell.
3. Conclusions
An ultimate goal in cancer therapy is to devise individually tailored a treatment that targets growth-promoting pathways and circumvents drug resistance. With a lack of marketable products, pharmaceutical companies have begun to lose interest. Only a few compounds are currently in clinical trials, as the development of most of the inhibitors has discontinued.
Next, the scientists created new drug conjugates by attaching the drugs to peptides known to bind to cancer cells. They designed the bridges between the peptides and the drugs to "switch off" the drugs. The bridges were to explain and "switch on" the drugs only in specific chemical environments within the leukemia cells, where they were predicted to be most effective.
With high precision and little side effects, the scientists say, the conjugates could make cancer drugs already on the market more effective and give new life to cancer drugs that shelved for being too toxic.
Combination chemotherapy is medicine’s best attempt to prevent mutation and resistance. By combining two or three chemotherapeutic agents a complete kill occurs. Cancer cells are attacked by multiple drugs with synergy by disrupting different stages of the cell reproduction cycle. This field required more investigation in the future, for example, the combination of the two anticancer MTX and photodynamic drug aminolevulinic acid as a surrogate of the glutamic moiety (figure 32), or acting as a polyglutamate terminal A, B, and C shown in (figure 33).
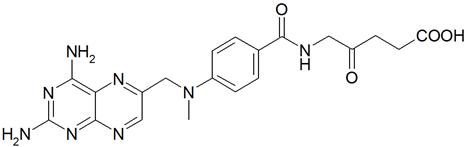
Figure 32. The proposed combination of MTX and Al.
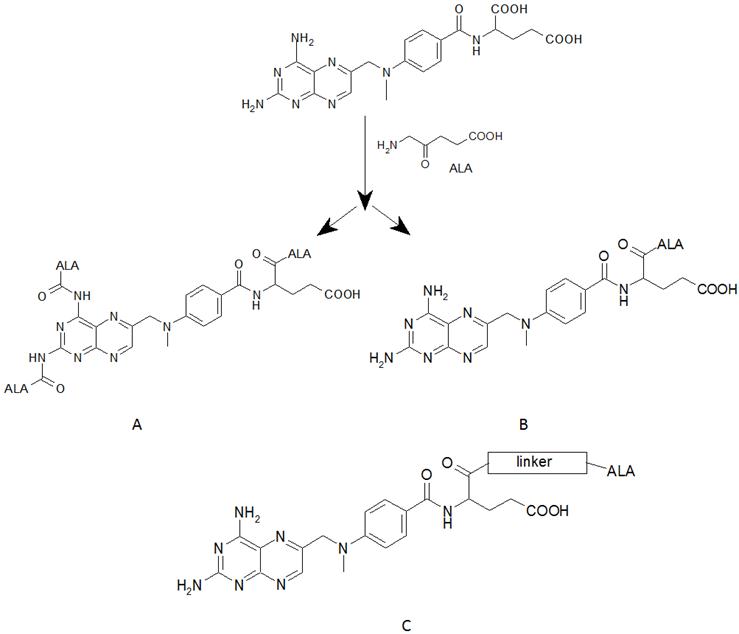
Figure 33. Proposal studies for new photodynamical MTX.
Despite dramatic advancements of drug delivery in scientific research, too little has been precisely established concerning their drug release properties, targeting abilities and therapeutic efficacy.
Collaborative and standardized efforts to develop and evaluate novel drugs are necessary to ultimately provide effective long-term treatment for this high-risk, complicated population.
References
- Gottesman MM. Mechanisms of cancer drug resistance. Ann Rev Med 2002; 53: 615–27.
- Abali EE, Skacel NE, Celikkaya H, Hsieh YC. Regulation of human dihydrofolate reductase activity and expression. Vitamin and Hormone 79: 267-287.
- Schnell JR, Dyson HJ, Wright PE. Structure dynamics, and catalytic function of dihydrofolate reductase. Ann Rev Biophys Biomol struct 2004; 33: 119-140.
- Abdulrahman L, Chhabra SR. The Chemistry of Methotrexate. Med Res Rev 1988; 8: 95-155.
- Rosowsky A, Beardsley GP, Ensminger WD, Lazarus H, Yu CS. Methotrexate analogs 11. Unambiguous chemical synthesis and in vitro biological evaluation of alpha- and gamma-monoesters as potential prodrugs. J Med Chem 1978; 21: 380–386.
- Jerry BH, George P. Protein Design and the Development of New Therapeutics and Vaccines. Plenium press, NY 1990: 307
- Bavetsias V, Jackman AL, Marriott JH, Kimbell R, Gibson W, Boyle FT, Bisset GM. Folate-based inhibitors of thymidylate synthase. J Med Chem 1997; 40: 1495-1510.
- Gangjee A, Yang J, McGuire JJ, Kisliuk RLSynthesis and evaluation of a classical 2,4-diamino-5-substituted-furo[2,3-d]pyrimidine and a 2-amino-4-oxo-6-substituted-pyrrolo[2,3-d]pyrimidine as antifolates. Bioorg & Med Chem 2006; 14: 8590-8598.
- Gangjee A, Devraj R, McGuire JJ, Kisliuk RL. Effect of bridge region variation on antifolate and antitumor activity of classical 5-substituted 2,4-diaminofuro[2,3-d]pyrimidines. J Med Chem 1995; 38: 3798.
- Gangjee A, Devraj R, McGuire JJ, Kisliuk RL, Queener SF, Barrows LR. Classical and Nonclassical Furo[2,3-d]pyrimidines as Novel Antifolates: Synthesis and Biological Activities J Med Chem 1994; 37: 1169.
- Gangjee A, Zeng Y, McGuire JJ, Kisliuk RL. Synthesis and antifolate properties of 10-alkyl-8,10-dideazaminopterins. J Med Chem 2000; 43: 3125.
- Lu YH, Gao XQ, Wu M, Zhang-Negrerie D, Gao Q. Strategies on the development of small molecule anticancer drugs for targeted therapy. Mini Rev Med Chem. 2011; 11: 611-24.
- David A. Gewirtz, A. Critical Evaluation of the Mechanisms of Action Proposed for the Antitumor Effects of the Anthracycline Antibiotics Adriamycin and Daunorubicin, Biochemical Pharmacology 1999; 57: 727–741.
- Baskar R, Lee KA, Yeo R, Yeoh KW. Cancer and Radiation Therapy: Current Advances and Future Directions. Int J Med Sci 2012; 9: 193-199.
- Li Y, Haiqing D, Li X, Shi D, Li Y. Single Polymer-drug Conjugate Carrying Two Drugs for Fixed-dose Codelivery. Med chem 2014; 4: 676-683.
- William BL, David RK, Brandon VS, Nicholas AP. Polymers for Drug Delivery Systems. Ann Rev Chem Biomol Eng 2010; 1: 149–173.
- Webster R, Didier E, Harris P, Siegel N, Stadler J, Tilbury L, Smith D. PEGylated proteins: Evaluation of their safety in the absence of definitive metabolism studies. Drug Metab Dispos 2007; 35: 9–16.
- Pasut G, Sergi M, Veronese FM. Anti-cancer PEG-enzymes: 30 years old, but still a current approach. Adv Drug Deliv Rev 2008; 60: 69–78.
- Ryan SM, Mantovani G, Wang X, Haddleton DM, Brayden DJ. Advances in PEGylation of important biotech molecules: delivery aspects. Expert Opin Drug Deliv 2008; 5: 371–383.
- Haiqing D, Chunyan D, Wenjuan X, Yongyong L, Tianbin R. Self-assembled, redox-sensitive, H-shaped pegylated methotrexate conjugates with high drug-carrying capability for intracelular drug delivery. Med Chem Commun 2014; 5: 147-152.
- Riebeseel K, Biedermann E, Lӧser R, Breiter N, Hanselmann R, Muelhaupt R, Unger C, Kratz F. Polyethylene glycol conjugate of MTX varying in molecular weight from MW 750 to MW 40.000: synthesis, characterization and structure activity relationships in vitro and in vivo. Bioconj Chem 2002; 13: 773-785.
- Gholamhossein Y, Seyed M F, Afshin Z, Alireza S. Synthesis and Characterization of Methotrexate Polyethylene Glycol Esters as a Drug Delivery System. Chem Pharm Bull 2010; 58: 147-153.
- Divya BB. Pegylated methotrexate based micellar conjugates for anticancer chemotherapy. Asian J Parmaceutics 2015; 9: 69-82.
- Fanghong L, Yang L, Mengmeng J, Fei C, Hongjie W, Fei Y, Jinyan L, Xiangrui Y, Zhenqing H, Qiqing Z. Validation of a Janus role of methotrexate-based PEGylated chitosan nanoparticles in vitro. Nanoscale Res Letters 2014; 9: 363.
- Chetana DM, Suketu JP, Alpesh BD, Murthy RSR. Functionalization and evaluation of PEGylated Carbon Nanotubes as novel Drug delivery for methotrexate. J Appl Pharm Sci 2011; 1: 103-108.
- W Li, P Zhan, ED Clercq, H Lou, X Liu. Current drug research on PEGylation with small molecular agents. Prog Poly Sci 2013; 38: 421-444.
- Newkome GR, Yao ZQ, Baker GR, Gupta VK. Micelles. Part 1. Cascade molecules: a new approach to micelles A [27] -arborol. J Org Chem 1985; 50: 2003-2004.
- Duncan R, Dimitrijevic S, Evagorou EG. The Role of Polymer Conjugates in the Diagnosis and Treatment of Cancer. STP Pharma Sci 1996; 6: 237-263.
- Maeda H, Seymour LW, Miyamoto Y. Conjugates of Anticancer Agents and Polymers: Advantages of Macromolecular Therapeutics in Vivo. Bioconj Chem 1992; 3: 351-362.
- Mehvar R. Dextrans for Targeted and Sustained Delivery of Therapeutic and Imaging Agents. J Control Release 2000; 69: 1-25.
- Matsumura RB, Maeda H. A New Concept for Macromolecular Therapeutics in Cancer Chemotherapy: Mechanism of Tumoritropic Accumulation of Proteins and the Antitumor Agent SMANCS. Cancer Res 1986; 46: 6387-6392.
- Ellens H, Bentz J, Szoka FC. H+-Induced and Ca-2+-Induced Fusion and Destabilization of Liposomes. Biochem 1985; 24: 3099-3106.
- Watkins DM, Sayed-Sweet Y, Klimash JW, Turro NJ, Tomalia DA. Dendrimers with hydrophobic cores and the formation of supramolecular dendrimersurfactant assemblies. Langmuir 1997; 12: 3136-3141.
- Hawker CJ, Wooley KL, Fre´chet JMJ. Unimolecular Micelles and Globular Amphiphiles - Dendritic Macromolecules as Novel Recyclable Solubilization Agents. J Chem Soc Perkin Trans 1 1993; 12: 1287-1297
- Tomalia DA, Baker H, Dewald J, Hall M, Kallos G, Martin S, Roeck J, Ryder J, Smith P. A New Class of Polymers-Starburst-Dendritic Macromolecules. Polym J 1985; 17: 117-132.
- Haensler J, Szoka FCJr. Poliamidoamine Cascade Polymers Mediate Efficient Transfection of Cells in Culture. Bioconj Chem 1993; 4: 372-379.
- Malik N, Wiwattanapatapee R, Klopsch R, Lorenz K, Frey H, Weener JW, Meijer EW, Paulus W, Duncan R. Dendrimers: Relationship Between Structure and Biocompatibility in Vitro, and Preliminary Studies on the Biodistribution of 125I-Labeled Polyamidoamine Dendrimers in Vivo. J Control Release 2000; 65: 133-148.
- Supattapone S, Wille H, Uyechi L, Safar J, Tremblay P, Szoka FCJr, Cohen FE, Prusiner SB, Scott MR. Branched Polyamines Cure Prion-Infected Neuroblastoma Cells. J Virol 2001; 75: 3453-3461.
- Duncan R, Malik N. Dendrimers: Biocompatibility and Potential for Delivery of Anticancer Agents. Proc Int Symp Controlled Release Bioact Mater 1996; 23: 105-106.
- Jolanta FKL, Kimberly AC, Zhengyi C, Shraddha SN, Istvan JM, Thommey PT, Lajos PB, Mohamed KK. Nanoparticle Targeting of Anticancer Drug Improves Therapeutic Response in Animal Model of Human Epithelial Cancer. Cancer Res 2005; 65: 5317-5324.
- Yuehua Z, Thommey PT, Ankur D, Hong Z, Pascale R L, Istvan J. Majoros, James RBJr. Targeted Dendrimeric Anticancer Prodrug: A Methotrexate-Folic Acid-Poly (amidoamine) Conjugate and a Novel, Rapid, "One Pot" Synthetic Approach. Bioconj Chem 2010; 21: 489–495.
- David DND, Eberhard N, Margo N, Constance EJ, van R. Carrier-bound Methotrexate. III, Antiproliferative activity of macromolecular MTX conjugates against the human HeLa and colon carcinoma cell lines. S Afr J Chem 2003; 59: 33-42.
- Khatri S, Das NG, Das SK. Effect of methotrexate conjugated PAMAM dendrimers on the viability of MES-SA uterine cancer cells. J Pharm Bioall Sci 2014; 6: 297-302.
- Linda S L, John J, Weixian M, Verica R, Kishor M W, Helen M B. Methotrexate loaded poly (l-lactic acid) microspheres for intra-articular delivery of methotrexate to the joint. J Pharm Sci, 2004; 93: 943-956.
- Hawker CJ, Fre´chet JMJ. Preparation of Polymers with Controlled Molecular Architecture - A New Convergent Approach to Dendritic Macromolecules. J Am Chem Soc 1990; 112: 7638-7647.
- Kono K, Liu M, Fre´chet JMJ. Design of Dendritic Macromolecules Containing Folate or Methotrexate Residues. Bioconj Chem 1999; 10: 1115-1121.
- Dang JM, Leong KW. Natural polymers for gene delivery and tissue engineering. Adv Drug Deliv Rev 2006; 58: 487–499.
- Ratner BD, Bryant SJ. Biomaterials: Where we have been and where we are going. Ann Rev Biomed Eng 2004; 6: 41–75.
- Chen J, Jo S, Park K. Polysaccharide hydrogels for protein drug delivery. Carbohydr Polym 1995; 28: 69–76.
- Mizrahy S, Peer D. Polysaccharides as building blocks for nanotherapeutics. Chem Soc Rev 2012; 41: 2623–2640.
- Liu Z, Jiao Y, Wang Y, Zhou C, Zhang Z. Polysaccharides-based nanoparticles as drug delivery systems. Adv Drug Deliv Rev 2008; 60: 1650–1662.
- Saravanakumar G, Jo DG, Park JH. Polysaccharide based nanoparticles: A versatile Platform for Drug Delivery and Biomedical Imaging. Curr Med Chem 2012; 19: 3212–3219.
- Mehvar R. Recent trends in the use of polysaccharides for improved delivery of therapeutic agents: pharmacokinetic and pharmacodynamic perspectives. Curr Pharm Biotechnol 2003; 4: 283302.
- Dmitry N, Renata B, Urszula K, Monika J, Mohamed SO, Janusz B, Adam O. Antitumor Properties and Toxicity of Dextran-methotrexate Conjugates are Dependent on the Molecular Weight of the Carrier. Anticancer Res 2006; 26: 1135-1144.
- Ying C, Frederick E, Tan RL. Synthesis and Characterization of Dextran−Peptide−Methotrexate Conjugates for Tumor Targeting via Mediation by Matrix Metalloproteinase II and Matrix Metalloproteinase IX. Bioconjug Chem 2004; 15: 931-941.
- Goszczyński TM, Filip-Psurska B, Kempińska K, Wietrzyk J, Boratyński J. Hydroxyethyl starch as an effective methotrexate carrier in anticancer therapy. Pharmacol Res Perspect 2014; 2: e00047.
- Shoshy M, Dalit LM, Dan P; Sweet Fairytale. Carbohydrates as Backbones for Glyconanomedicine. Isr J Chem 2013; 53: 616-629.
- Singh UV, Aithal KS, Udupa N. Physicochemical and Biological Studies of Inclusion Complex of Methotrexate with β-Cyclodextrin. Pharma Sci 1997; 3: 573-577.
- Juan-Juan Y, Sonali S, Stepan P S, Zhi-Xin W, Zhi-Wei Z. Synthesis and Biological Evaluation of Novel Folic Acid Receptor-Targeted, β-Cyclodextrin-Based Drug Complexes for Cancer Treatment. PLOS One 2013; 8: e62289.
- Taheri A, Dinarvand R, Salman NF, Khorramizadeh MR, Taheri BA, Mansoori P, Atyabi F. Use of biotin targeted methotrexate-human serum albumin conjugated nanoparticles to enhance methotrexate antitumor efficacy. Int J Nanomed 2011; 6: 1863-74.
- Shin JM, Kim SH, Thambi T, You DG, Jeon J, Lee JO, Chung BY, Jo DG, Park JH. A hyaluronic acid-methotrexate conjugate for targeted therapy of rheumatoid arthritis. Chem Commu 2014; 50: 7632-7635.
- Homma A, Sato H, Okamachi A, Emura T, Ishizawa T, Kato T, Matsuura T, Sato S, Tamura T, Higuchi Y. Novel hyaluronic acid–methotrexate conjugates for osteoarthritis treatment. Bioorg Med Chem 2009; 17: 4647–4656.
- Anna M, Monica C. Hyaluronic Acid Bioconjugates for the Delivery of Bioactive Molecules. Polym 2014; 6: 346-369.
- Budzynska R, Nevozhay D, Kanska U, Jagiello M, Opolski A, Wietrzyk J, BoratynskiJ. Antitumor activity of mannan-methotrexate conjugate in vitro and in vivo. Oncol Res 2007; 16: 415-421.
- Blauchfield J, Toth I. Lipid, sugar and polysaccharide based delivery system. Current Med Chem 2004; 11: 2375-2382.
- Lockett T, Reilly W, Manthey M, Wells X, Cameron F, Moghddam M, Johnston J, Smith K, Francis C, Yang Q, Whittaker R. Tris Lipidation: A Chemically Flexible Technology For Modifying The Delivery Of Drugs and Genes. Clin Exp Pharmac Physio 2000; 27: 563-567.
- Pignatello R, Spampinato G, Sorrenti V, Di GC, Vicari L, McGuire JJ, Russell CA, Puglisi G, Toth I. Lipophilic methotrexate conjugates with antitumor activity. Eur J Pharma Sci 2000; 10: 237-245.
- Jaroslav T, Andrew DM, Zuzana K, Róbert L, Josef M, Štěpán K, Milan R. Lipid-Based Nanoparticles and Microbubbles – Multifunctional Lipid-Based Biocompatible Particles for in vivo Imaging and Theranostics. Advances in Bioengineering 2015; edited by Pier Andrea Serra, ISBN 978-953-51-2141-1.
- Wang X, Liu P, Yang W, Li L, Li P, Liu Z, Zhuo Z, Gao Y. Microbubbles coupled to methotrexate-loaded liposomes for ultrasound-mediated delivery of methotrexate across the blood–brain barrier. Int J Nanomed 2014; 9: 4899-4909.
- Furuhata A, Honda K, Shibata T, Chikazawa M, Kawai Y, Shibata N, Uchida K. Monoclonal antibody against protein- bound glutathione: use of glutathione conjugate of acrolein-modified proteins as an immunogen. Chem Res Toxicol 2012; 25: 1393-1401.
- Heidi LP, Pina MC, Shrikant D, Sanjeev G, Gretchen MS, Gregory DV, Robert MB. Antibody-drug conjugates: Current status and future directions. Drug Discov Today 2013; 1-13.
- Franco D, Paola B, Luigi Cattel. Immunotoxins and Anticancer Drug Conjugate Assemblies: The Role of the Linkage between Components. Toxins 2011; 3: 848-883.
- Martin CG, Robert WB. An improved synthesis of a Methotrexate-Albumin-791T/36 Monoclonal Antibody Conjugate cytotoxic to Human Osteogenic Sarcoma Cell Lines. Cancer Res 1986; 46: 2407-12.
- Raymond E, Nicole HPC, Jan W, Liesbeth VD, Peter JB, Piet B. Transport of glutathione prostaglandin A conjugates by the multidrug resistance protein 1. Febs Letters 1997; 419: 112-116.
- Noriaki E, Yoshinori K, Yumiko T, Masahiko S, Naoji U, Kazuo K, Takeshi H. In Vitro Cytotoxicity of a Human Serum Albumin-mediated Conjugate of Methotrexate with Anti-MM46 Monoclonal Antibody. Cancer Res 1987; 47: 1076-1080.
- Noriaki K, Yumiko T, Naoji U, Kazuo K, Kenzo W, Masahiko S, Yoshinori K, Takeshi H. Nature of Linkage and Mode of Action of Methotrexate Conjugated with Antitumor Antibodies: Implications for Future Preparation of Conjugates. Cancer Res 1988; 48: 3330-3335.
- Rowland AJ, Harper ME, Wilson DW, Griffiths K. The effect of an anti-membrane antibody methotrexate conjugate on the human prostatic tumor line PC3. B J Cancer 1990; 61: 702-708.
- Geoffrey P, Kenia K. Antibody-Targeted Drugs for the Therapy of Cancer. J Drug Target 1994; 2: 183-215.
- Cloe K. Macrocyclic chemistry, current trends and future perspectives. Springer 2005; 407-425.
- Wen-Hao W, Mark F, Darren M, Zhong W, Phil L, Mimi M, Dale M, Jonathan LS. Gadolinium texaphyrin–methotrexate conjugates. Towards improved cancer chemotherapeutic agents. Org Biomol Chem 2005; 3: 3290-3296.
- Feng L, Liu Z. Graphene in biomedicine: opportunities and challenges. Nanomedicine (Lond) 2011; 6: 317-324.
- Georgakilas V, Otyepka M, Bourlinos AB, Chandra V, Kim N. Functionalization of graphenes: Covalent and noncovalent approaches, derivatives and applications. Chem Rev 2012; 112: 6156-6214.
- Singh I, Rehni AK, Kumar P, Kumar M, Aboul-Enein HY. Carbon Nanotubes- Synthesis, Properties and Pharmaceutical Applications. Fullerenes, Nanotubes and Carbon Nanostruct 2009; 17: 361–377.
- Huiyun W, Yongyong L. Redox Sensitive Nanoparticles with Disulfide Bond Linked Sheddable Shell for Intracellular Drug Delivery. Med Chem 2014; 4: 748-755.
- Romberg B, Hennink WE, Storm G. Sheddable coatings for long circulating nanoparticles. Pharm Res 2008; 25: 55-71.
- Mohammad JA, Jaleh B, Ali MA, Soodabeh D, Yadollah O, Mohammad-Reza R. Methotrexate-conjugated quantum dots: synthesis, characterisation and cytotoxicity in drug resistant cancer cells. J Drug Targeting 2016; 24: 120-133.
- Pei JW, Keng LO, Jem KC, Hsiao PF, Shin HT, Wei XL, Jia YC. Methotrexate-conjugated AgInS2/ZnS quantum dots for optical imaging and drug delivery. Material Letter 2014; 128: 412-416.
- Prato M, Kostarelos K, Bianco A. Functionalized carbon nanotubes in drug design and discovery. Acc Chem Res 2008; 41: 60-8.
- Pastorin G, Wu W, Wieckowski S, Briand JP, Kostarelos K, Prato M, Bianco A. Double functionalization of carbon nanotubes for multimodal drug delivery. Chem Commun 2006; 11: 1182-4.
- Samorı C, Ali-Boucetta H, Sainz R, Guo C, Toma FM, Fabbro C, da Ros T, Prato M, Kostarelos K, Bianco A. Enhanced anticancer activity of multi-walled carbon nanotube-methotrexate conjugates using cleavable linkers. Chem Commun 2010; 46: 1494-6.
- Marega R, Bergamin M, Aroulmoji V, Dinon F, Prato M, Murano E. Hyaluronan-carbon nanotube derivatives: Synthesis, conjugation with model drugs, and DOSY NMR characterization. Eur J Org Chem 2011; 2011: 5617–5625.
- Xinlin Y, Ali E, Jie L, Quanjun C. Fullerene–biomolecule conjugates and their biomedicinal applications. Int J Nanomed 2014; 9: 77–92.
- Xiunan W, Yi L, Jingcheng X, Shengjuan L, Fada Z, Qian Y, Xiao Z. Molecular Dynamics Study of Stability and Diffusion of Graphene-Based Drug Delivery Systems. J Nanomaterials 2015; 1-14.
- Jun Yue, Shi Liu, Rui Wang, Xiuli Hu, Zhigang Xie, Yubin Huang, Xiabin Jing. Transferrin-Conjugated Micelles: Enhanced Accumulation and Antitumor Effect for Transferrin-Receptor-Overexpressing Cancer Models. Mol Pharmaceutics 2012; 9: 1919–1931.
- Woitoniszak M, Urbas K, Peruzynska M, Kurzawski M, Drozdzik M, Mijowska E. Covalent conjugation of graphene oxide with methotrexate and its antitumor activity. Chem Phys Letter 2013; 151-156.
- Abbing A, Blaschke UK, Grein S, Kretschmar M, Stark CMB, Thies MJW, Walter J, Weigand M, Woith DC, Hess J, Reiser COA. Efficient Intracellular Delivery of a Protein and a Low Molecular Weight Substance via Recombinant Polyomavirus-like Particles. J Biol Chem 2004; 279: 27410.
- Bert JL, Wen-Lin PT, Foad M, Edward AP, Anne B M, Daniel T K. Inhibition of Transferrin Iron Release Increases in Vitro Drug Carrier Efficacy. J Control Release. 2007; 117: 403–412.
- Justin PS, Margaret AP, Nicholas AP. Cellular Revaluation of Synthesized Insulin/ Transferrin Bioconjugates for Oral Insulin Delivery Using Intelligent Complexation. Macromol Biosci 2010; 10: 299–306.
- Ren I K, Dusad I A, Dong R, Quan L. Albumin as a Delivery Carrier for Rheumatoid Arthritis. J Nanomed Nanotechol 2013; 4: 4.
- Wunder A, Müller-Ladner U, Stelzer EHK, Funk J, Neumann E, Stehle G, Pap T, Sinn H, Gay S, Fiehn Ch. Albumin-Based Drug Delivery as Novel Therapeutic Approach for Rheumatoid Arthritis. J Immunology 2003; 170: 4793-4801.
- Jin-Ho Choy et al. Layered double hydroxide as an efficient drug reservoir for folate derivatives. Biomaterials 2004; 25: 3059–3064.
- Jae-Min Oh et al. Efficient delivery of anticancer drug MTX through MTX-LDH Nanohybridsystem. J Phys & Chem Solids 2006; 67: 1024–1027.
- Chakraborty M, Dasgupta S, Saundrapandian C, Basu D. Methotrexate intercalated ZnAl-layered double hydroxide. J Solid State Chem 2011; 184: 2439-2445.
- Shams A. Nadhum, Mohammed HM. Design, Synthesis, Characterization and Preliminary Anticancer Study for Methotrexate Silibinin Conjugates. Iraqi J Pharm Sci 2015; 24: 74-84.
- DeBin JA, Strichartz GR. Chloride channel inhibition by the venom of the scorpion Leiurus quinquestriatus. Toxicon 1991; 29: 1403–8.
- Conroy S, Chen F, Zachary S, Omid V, Stacey H, Donghoon L, Richard GE, Jim O, Miqin Z. Tumor-targeted drug delivery and MRI contrast enhancement by chlorotoxin-conjugated iron oxide nanoparticles. Nanomedicine 2008; 3: 495–505.
- Gauri S, Anjani KT, Nitin K, Deepa S, Pushpa M, Harish C, Anil K M. Cancer Biotherapy and Radiopharmaceuticals. 2008; 23: 571-580.
- Kuznetsova N, Kandyba A, Vostrov I, Kadykov V, Gaenko G, Molotkovsky J, Vodovozova E. Liposomes loaded with lipophilic prodrugs of methotrexate and melphalan as convenient drug delivery vehicles. J Drug Del Sci Tech 2009; 19: 51-59.
- Stephan JK, Robert FS, John CDD, James CH. Chemically induced dimerization of dihydrofolate reductase by a homobifunctional dimer of methotrexate. Chem & Bio 2000; 7: 313-321.
- Carston RW. Protein nanorings. US8236925 B1 Aug 7, 2012.
- Fazle H, Richard PS, Helen MC, Georges LS. Targeted Delivery of Antineoplastic Agent to Bone: Biodistribution Studies of Technetium-99m-Labeled Gem-Bisphosphonate Conjugate of Methotrexate. J Nuclear Med 1996; 37: 105-107.
- Xiao-Hong O, An-Ren K, Zheng-Lu L, Xian P. Receptor binding characteristics and cytotoxicity of insulin-methotrexate. World J Gastroenterol 2004; 10: 2430–2433.
- Hugh MT. Compounds and methods for treating cancer. US8501906 B2, Aug 6, 2013.
- Samra ZQ, Ahmad S, Javeid M, Dar N, Aslam MS, Gull I, Ahmad MM. Anticancer medicines (Doxorubicin and methotrexate) conjugated with magnetic nanoparticles for targeting drug delivery through iron. Prep Biochem Biotechnol 2013; 43: 781-97.
- Ashwanikumar N, Kumar NA, Nair AS, Kumar GSV. Dual drug delivery of 5-fluorouracil (5-FU) and methotrexate (MTX) through random copolymeric nanomicelles of PLGA and polyethylenimine demonstrating enhanced cell uptake and cytotoxicity. Colloids Surf B Biointerfaces 2014; 23: 520-8.
- Virginia WC. Covalent chemical inducers of protein dimerization and their uses in high throughput binding screens. WO 2002059272 A2, Aug 1, 2002.
- Virginia WC. Binding and catalysis screen for high throughput determination of protein function using chemical inducers of dimerization. US 20020168737 A1, Nov 14, 2002.
- Virginia WC. Methods and assays for screening protein targets. US 7419780 B2, Sep 2, 2008.



