Association Between Leptin Hormone and Thyroid Hormone Levels in Hypothyroid, Hyprethyroid and Euthyroid Subjects
Maher K. Ibrahim1, *, Abdul-Monaim H. Al-Samarrai2, Khudhair A. Khudhair1
1Department of Biochemistry, College of Medicine, University of Tikrit, Tikrit, Iraq
2Department of Chemistry, College of Education, University of Samarra, Samarra, Iraq
Abstract
Leptin is a hormone secreted by adipose tissues and is considered as a satiety hormone, it is known to be an important regulator of food intake and energy storage. Disturbance of thyroid function is associated with marked changes in both body weight and energy expenditure, and it has therefore been the subject of much research to study the mutual roles of leptin and thyroid hormones in this respect. Very few researches are done to investigate the possible association of serum leptin and thyroid hormones in Iraq. Despite intensive research in this field, results are still not very clear. Objective of this study was to find any possible association of serum leptin levels and thyroid hormones. This prospective, randomized study was conducted in Baghdad; Iraq. The subjects were selected from Medical City Hospital. Serum samples were collected from 180 individuals; 56 (31%) of them were males and 124 (69%) females. The patients classified into three groups, two groups for thyroid dysfunctions patients (hypothyroid and hyperthyroid patients) and the third group as control group (euthyroid). The body weight of each individual was measured using a carefully calibrated weighing balance. The height of each individual was measured to calculate BMI ratio. Blood samples were taken early in the morning, 12 hours postprandial. The serum samples were stored at (-20°C) until required for thyroid hormones (Total and Free T3, T4 & TSH) and plasma leptin measurements (by using ELISA). To determine if serum leptin levels are affected by thyroid dysfunction, we measured its concentration in serum samples from 55 euthyroid controls, mean age 36.9±9.9 yr and 125 subjects: 74 patients with hypothyroidism, mean age 44.3±7.0 yr, and 51 patients with hyperthyroidism, mean age 43.5±6.9 yr. Mean leptin levels in the euthyroid (3.69±1.94 ng/ml), hypothyroid (4.97±2.61 ng/ml) and hyperthyroid (2.36±1.26 ng/ml) groups were significantly different. The results showed no significant correlation in serum leptin and T3, T4, FT3, FT4, TSH either in the hypothyroid or in the hyperthyroid and euthyroid control group of patients. These data suggest that leptin levels are not affected by thyroid dysfunction. There was a significant positive correlation between BMI and leptin level (r = 0.29, p =.03) in euthyroid controls, (r = 0.35, p =.01) in hypothyroid and (r = 0.33, p =.01) in hyperthyroid. Serum leptin levels in males were lower than those recorded in females [hypothyroid patients; 4.4±2.1 and 5.1±2.7 ng/ml; P˃0.05: hyperthyroid patients; 2.0±0.63 and 2.5±1.45 ng/ml; P˃0.05: euthyroid; 3.2±1.8 and 3.9±2.0 ng/ml; P˃0.05]. In conclusion, leptin hormone was no significantly correlated with thyroid hormone function in eu-, hypo-, and hyperthyroid patients. Leptin level is highly correlation with the BMI might be confirmed that BMI and gender are the major determinant of leptin levels.
Keywords
Leptin, Hyperthyroidism, Hypothyroidism, Euthyroidism
Received: July 25, 2016
Accepted: August 9, 2016
Published online: October 9, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Leptin is a 146-amino acid protein hormone encoded by the ob gene, it is an important circulating signal for the regulation of body weight [1] and secreted by adipocytes in response to an increase in fat mass [2]. Since its discovery, leptin has been the subject of an enormous amount of work especially within the fields of nutrition, metabolism and endocrinology. It is believed to be involved in interacts with putative receptors in the hypothalamus decreasing appetite, increasing energy expenditure and regulating body weight [3, 4]. In thyroid disorders there are changes in basal metabolic rate, oxygen consumption, appetite and body weight. Thyroid hormones (TH) are important regulators of both basal and total energy consumption, and modulate the activity of several enzymes involved in lipid metabolism [5].
Although TH and leptin are both involved in the regulation of energy metabolism, the precise interrelationship between the two endocrine systems (leptin and TH) is presently incompletely understood and still controversial [6-19]. This might have to do with interference of major factor controlling the serum concentration of leptin; fat mass and gender. BMI and the fat mass of the body shows as a strong relationship exist with serum leptin concentration and is presumably the most important physiological determinant [20]. A clear sexual dimorphism of serum leptin concentration is noted, with leptin levels in females being twice as high as in males [21] as well as other studies differed in terms of patient characteristics, length of treatment (if performed), and method for measuring serum leptin. It is therefore not surprising that extreme variation in the results was seen. A large number of studies investigated the relationship between thyroid dysfunctions and circulating levels of leptin, but the reported results were highly conflicting both in basal conditions and after correction of the thyroid dysfunction. In hypothyroid subjects serum leptin was found to be increased [3, 6, 15, 17, 18, 22], decreased [7, 9, 12, 23] and unchanged [8, 10, 11, 13, 24, 25] compared with a control group and/or euthyroid subjects. In hyperthyroid subjects serum leptin was increased [7, 8, 14], decreased [3, 6, 22, 23] and unchanged [9, 10, 13, 16, 18, 24, 25].
The aim of this study has been to provide new data on the relationship between plasma leptin levels in relation to thyroid dysfunction.
2. Materials and Methods
2.1. Subjects
We studied 180 adult patients (124 females and 56 males) aged 20-63 years with thyroid disorders: 74 were affected with autoimmune primary hypothyroidism (55 females, 19 males), 51 with hyperthyroidism (35 females, 16 males) and 55 with euthyroid control (34 females, 21 males). Body weight, height and body mass index (BMI; kg/m2) were determined for each patient. Thyroid function was assessed by measuring serum fasting total and free triiodothyronine (TT3, FT3), total and free thyroxine (TT4, FT4), and thyrotropin (TSH). Serum leptin levels were measured at (900 h) after an overnight fast.
2.2. Assays
Serum leptin levels were determined by Enzyme-linked immunosorbant assay (ELISA). Also circulating levels of TT3, FT3, TT4, FT4 and TSH were measured by ELISA technique.
2.3. Statistical Methods
All data were analyzed using SPSS software for Windows, 13 (SPSS, Inc. Chicago, USA). Age, BMI, serum TSH, TT4, FT4, TT3, FT3 and leptin levels were compared among the various groups of patients using Student’s t-test and within each group by linear regression analysis. Data are expressed as means±S.D.
3. Results
Serum TSH was 15.12±8.9 mU/l in hypothyroid a highly significant increase compared to 1.96±1.00 mU/l (mean±SD) in euthyroid patients and 0.15±0.08 mU/l in hyperthyroid patients. TT3 and TT4 levels were 0.45±0.32 ng/l and 3.67±1.59 µg/dl a significant decrease in the hypothyroid compared to 1.28±0.28 ng/l and 8.18±1.87 µg/dl in the euthyroid, 2.89±1.17 ng/l and 14.83±3.71 µg/dl in the hyperthyroid group respectively.
FT3 and FT4 were 1.15±0.66 and 0.53±0.31 ng/l in the hypothyroid also show a highly significant decrease compared to 2.65±0.82 and 1.31±0.29 ng/l in euthyroid controls, 4.8±1.27 and 3.73±1.47 ng/l in the hyperthyroid group respectively (Table 1).
Table 1. Serum TT3, TT4, FT3, FT4 level and TSH level for eu-, hypo-, and hyperthyroid patients.
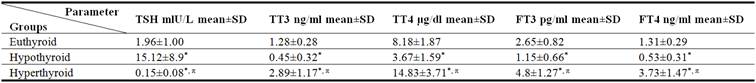
*P < 0.05 when compared to euthyroid. πP < 0.05 when compared hyperthyroid versus hypothyroid group.
SD; standard deviation.
Serum leptin in hypothyroid patients was significantly higher than in euthyroid controls (4.97±2.61 ng/ml vs 3.69±1.94 ng/ml, P < 0.05). While serum leptin in hyperthyroid patients was significantly lower than in euthyroid controls (2.36±1.26 ng/ml vs 3.69±1.94 ng/ml, P < 0.05) (Table 2 and Fig. 1)
Table 2. Serum leptin level for eu-, hypo-, and hyperthyroid patients.
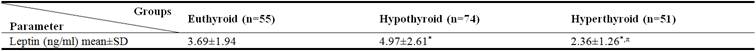
*P < 0.05 when compared to euthyroid. πP < 0.05 when compared hyperthyroid versus hypothyroid group.
SD; standard deviation. n= Number of subjects.
The difference found between hypothyroidism and hyperthyroidism patients was mainly due to the significantly different BMI in the two groups (30.73 vs 25.11 kg/m2; P <0.05), (Table 3) and possibly to the concomitant sex hormone.
The mean serum leptin levels in males with thyroid disorders and euthyroid group were in general lower than those recorded in females, [hypothyroid patients; 4.4±2.1 and 5.1±2.7 ng/ml; P˃0.05: hyperthyroid patients; 2.0±0.63 and 2.5±1.45 ng/ml; P˃0.05: euthyroid; 3.2±1.8 and 3.9±2.0 ng/ml; P˃0.05 respectively] (Table 4).
The statistical analysis of the results showed the serum leptin levels in non-obese was lower than those recorded in obese [hypothyroid patients; 3.83±1.5 and 5.8±2.1 ng/ml; p<0.05: hyperthyroid patients; 2.31±1.2 and 2.54±1.2 ng/ml; P˃0.05: euthyroid; 3.34±1.6 and 3.96±1.3 ng/ml; P˃0.05] (Table 5).
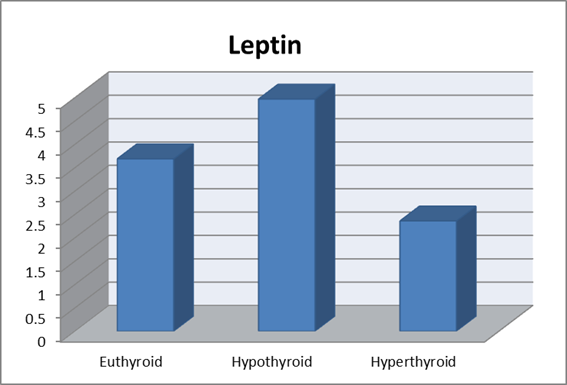
Figure 1. Serum leptin hormone levels in eu-, hypo-, and hyperthyroid patients.
Table 3. The mean±SD of BMI for eu-, hypo-, and hyperthyroid patients.
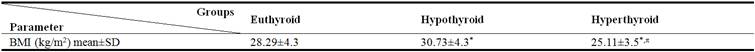
*P < 0.05 when compared to control. πP < 0.05 when compared hyperthyroid versus hypothyroid group.
SD; standard deviation.
Table 4. Serum levels of leptin in male and female for eu-, hypo-, and hyperthyroid patients.
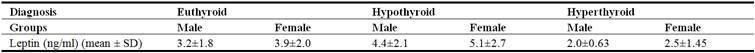
SD; standard deviation.
Table 5. Serum levels of leptin in obese and non-obese for eu-, hypo-, and hyperthyroid patients.
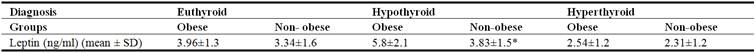
*P < 0.05 when compared to obese group. SD; standard deviation.
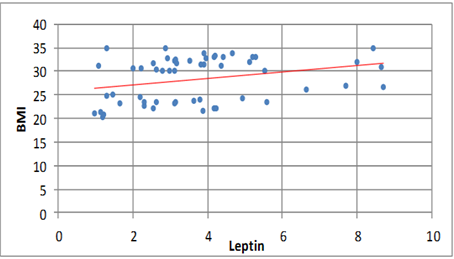
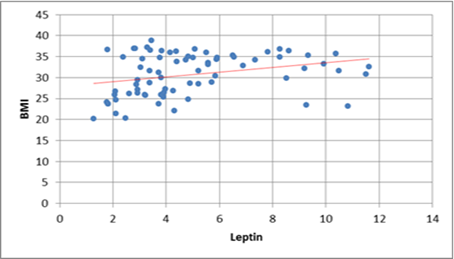
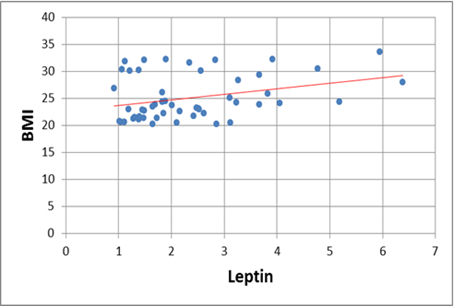
The correlation coefficient for leptin and the BMI in eu-, hypo-, and hyperthyroid patients was (r=0·29, P=0·03), (r=0·34, P=0·01), (r=0.33, P=0.01) respectively, (Fig. 2), with no evident relationship with the thyroid hormone status (Table 6).
Table 6. Correlation of serum leptin to biochemical parameters for eu-, hypo-, and hyperthyroid patients.
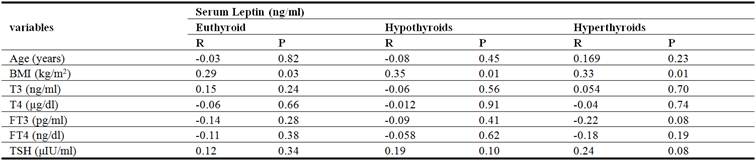
R= correlation coefficients. P= P-values
(a)
(b)
(c)
Figure 2. Positive correlation between leptin levels and BMI, a) in euthyroid b) hypothyroid and c) hyperthyroid group.
4. Discussion
There are conflicting results as to the effects of TH on the production of leptin, with suggestions that TH has inhibitory, stimulatory or no effect on levels of leptin.
In this study, there was no significant correlation between serum leptin and TH levels in eu-, hypo-, and hyperthyroid patients (Table 6). Other workers in the field [8, 11, 13, 17, 24, 25] suggested that leptin levels are not affected by thyroid dysfunction and observed circulating TH do not appear to play any relevant role in leptin synthesis and secretion. These findings supported our observations. Similar results by Sesmilo et al [10] who studied 16 patients with hypo- and 17 patients with hyperthyroidism, all of autoimmune origin, before therapy and every 6–8 weeks until euthyroidism was reached, BMI which correlated with serum leptin concentrations. No correlation was found between serum leptin and TH levels at any time during the study. Similarly, Corbetta et al [13], also found that circulating TH do not appear to play any relevant role in leptin synthesis and secretion and also founded females with either overt hypo- or hyperthyroidism after L-thyroxine therapy show differences in their standard deviation score, a subtle interaction between sex steroids and thyroid status in modulating leptin secretion, at least in women, may occur.
The present results clearly suggest that circulating TH do not play a major role in the regulation of leptin synthesis and secretion. Thus the ability of TH to regulate energy expenditure does not operate through variations in serum leptin levels. In contrast, they do not support previous studies in humans showing decreased leptin concentrations in hypothyroid patients [12] and in Zucker rats, demonstrating a decrease in leptin mRNA in response to T4 administration (26). In the latter case, the significant loss of animal weight and the consequent decrease in adipose stores probably account for the reduced leptin gene expression.
In agreement with other reports [21, 27, 28, 29], we found that serum leptin concentrations recorded in both normal controls and patients with thyroid disorders were characterized by high variability, the major determinants of which are BMI and gender. This figure is documented by the significant correlation between leptin levels and BMI in any group of patients with thyroid disorders, and by the finding that leptin levels in males are consistently lower than those found in females. Serum leptin levels are known to increase with the percentage of body fat and, to a lesser degree with the BMI. This was confirmed in our study (Table 5). Leptin showed significant positive correlation with BMI at (r=0.29; p=0.03) in euthyroid and (r=0.35; p=0.01) in hypothyroid and (r=0.33; p=0.01) in hyperthyroid groups (Table 6 and Figure 2). This result was expected; since the major source of leptin in the human body is the adipose tissue and the greater adipose tissue mass the greater is the leptin level.
This result supported by other studies that demonstrated serum leptin levels showed significant positive correlation with BMI. Yoshida et al [9] who revealed that, serum leptin levels were correlated significantly with BMI in the hypothyroid, hyperthyroid, and normal groups. Kennedy et al. [30] who reported in both men and women, fasting leptin levels were highly correlated with BMI. Similarly, Perry et al [31] also found the major factor controlling serum leptin is BMI as a strong relationship exists with serum leptin concentration. Van Gaal et al [32] who reported that circulating leptin levels appears to be one of the best biological markers of obesity and hyperleptinemia is directly reflect the amount of body fat. Other study by Kautzky-Willer et al [17] which agrees with our study it was reported higher leptin levels in obese hypothyroid subjects than in obese euthyroid subjects. Also our result supported by other study such as Baig et al [33] and Considine et al [20] that demonstrated serum leptin concentrations in lean and obese subject reflects the amount of adipose tissues and is directly proportional with fat contents.
Higher leptin levels in females are in agreement with a recently published study demonstrating the involvement of sex hormones in the regulation of leptin synthesis [21]. In addition, ob gene messenger RNA expression is increased in obese females compared with obese males [2].
The higher leptin levels in females than in males have previously been reported in population studies (Lonnqvist et al [2]; Saad et al [21]; Wabitsch et al [34], Baumgartner et al [35]) has been proposed that leptin levels in females being twice as high as in males and the higher leptin levels in females due to the different pattern of fat deposition and/or the role of sex hormones. Many studies support that sex hormones, in particular estradiol in women and testosterone in men, may be important contributors to the variations in serum leptin concentrations [36-38]. Second possibility for these sex differences in leptin concentrations may be explained by differences in the body composition. It is known that, females are likely to have a greater percentage of body fat than males [38, 39].
5. Conclusion
Lack of effects of circulating thyroid hormone levels on serum leptin concentrations. Leptin level for females was higher than leptin level for males. BMI in eu-, hypo- and hyper-thyroidism has been proved to be the major influencing variable of circulating leptin levels.
References
- Zhang Y, Proenca R, Maffei M, Leopold L & Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature 1994 372 425–431.
- Lu¨nnqvist F, Arner P, Nordfors L & Schalling M. Overexpression of the obese (ob) gene in adipose tissue of human obese subjects.Nature Medicine 1995 1 950–953.
- Pinkney JH, Goodrick SJ, Katz J, Johnson AB, Lightman SL & Coppack SW. Leptin and the pituitary-thyroid axis: a comparative study in lean, obese, hypothyroid and hyperthyroid subjects. Clin Endocrinol Oxf 1998 49 (5) 583-8.
- Caro JF. Sinha MK. Kolazynski JW, Zhang PL & Considine RV. Leptin: the tale of an obesity gene. Diabetes. 1996 45 1455-62.
- Wolf M, Weigert A & Kreymann G. Body composition and energy expenditure in thyroidectomized patients during shortterm hypothyroidism and thyrotropin-suppressive thyroxine therapy. European Journal of Endocrinology 1996 134 168– 173.
- Escobar-Morreale HF, Escobar del Rey F & Morreale de Escobar G. Thyroid hormones influence serum leptin concentrations in the rat. Endocrinology 1997 138 (10) 4485-8.
- Diekman MJ, Romijn JA, Endert E, Sauerwein H & Wiersinga WM. Thyroid hormones modulate serum leptin levels: observations in thyrotoxic and hypothyroid women. Thyroid 1998 8 1081-6.
- Ozata M, Ozisik G, Bingol N & Corakci A. The effects of thyroid status on plasma leptin levels in women. J Endocrinol Invest. 1998 21 (6) 337-41.
- Yoshida T, Momotani N, Hayashi M, Monkawa T, Ito K &, Saruta T. Serum leptin concentrations in patients with thyroid disorders. Clin Endocrinol Oxf 1998 48 (3) 299-302.
- Sesmilo G, Casamitjana R, Haperin I, Gomis R & Vildardell E. Role of thyroid hormones on serum leptin levels. Eur J Endocrinol 1998 139 (4) 428-30.
- Sreenan S, Caro JF & Refetoff S. Thyroid dysfunction is not associated with alterations in serum leptin levels. Thyroid 1997 7 (3) 407-9.
- Valcavi R, Zini M, Peino R, Casanueva FF & Dieguez C. Influence of thyroid status on serum immunoreactive leptin levels. J Clin Endocrinol Metab 1997 82 (5) 1632-4.
- Corbetta S, Englaro P, Giambona S, Persani L, Blum WF & Beck-Peccoz P. Lack of effects of circulating thyroid hormone levels on serum leptin concentrations. Eur J Endocrinol 1997 137 (6) 659-63.
- Zimmermann-Belsing T, Dreyer M, Holst JJ & Feldt-Rasmussen U. The relationship between the serum leptin concentrations of thyrotoxic patients during treatment and their total fat mass is different from that of normal subjects. Clin Endocrinol Oxf. 1998 49 589-95.
- Leonhard U, Gerdes E, Ritzel U, Schafer G, Becker W & Ramadori G. Immunoreactive leptin and leptin mRNA expression are increased in rat hypo- but not hyperthyroidism. J Endocrinol. 1999 163 115-21.
- Mantzoros CS, Rosen HN, Greenspan SL & Flier JS, Moses AC. Short-term hyperthyroidism has no effect on leptin levels in man. J Clin Endocrinol Metab 1997 82 497-9.
- Kautzky-Willer A, Ludwig C, Nowotny P, Roden A, Huemer C, Widhalm K, et al. Elevation of plasma leptin concentrations in obese hyperinsulinaemic hypothyroidism before and after treatment. Eur J Clin Invest 1999 29 395-403.
- Leonhardt U, Ritzel U, Schäfer G, Becker W & Ramadori G. Serum leptin levels in hypo- and hyperthyroidism. J Endocrinol. 1998 157 75-9.
- Yoshida T, Monkawa T, Hayashi M & Saruta T. Regulation of expression of leptin mRNA and secretion of leptin by thyroid hormone in 3T3-L1 adipocytes. Biochem Biophys Res Commun 1997 232 822-6.
- Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, Nyce MR, et al. Serum immunoreactive leptin concentrations in normal-weight and obese humans. N Eng J Med 1996 334 292-295.
- Saad MF, Damani S, Gingerich RL, Riad-Gabriel MG. Khan A, Boyadjian R, et al. Sexual dimorphism in plasma leptin concentration. J Clin Endocrinol Metab 1997 82 579-584.
- Rada FH, Al - Sa kkal N& Yahia A. Leptin in Goitrous patients. MMJ 2009 8 33 - 6.
- Iglesias P, Alvarez Fidalgo P, Codoceo R & Díez JJ. Serum concentrations of adipocytokines in patients with hyperthyroidism and hypothyroidism before and after control of thyroid function. Clin Endocrinol (Oxf) 2003 59 (5) 621-9.
- Yaturu S, Prado S& Grimes SR. Changes in adipocyte hormones leptin, resistin, and adiponectin in thyroid dysfunction. J Cell Biochem 2004 93 (3) 491-6.
- Santini F, Marsili A, Mammoli C, Valeriano R, Scartabelli G, Pelosini C, et al. Serum concentrations of adiponectin and leptin in patients with thyroid dysfunctions. J Endocrinol Invest 2004 27 (2) RC5-7.
- Swick AG, Carroll RS, Stevenson RW, Martin KA & Hargrove DM. Effects of thyroid hormone on metabolic rate and gene expression in fatty Zucker rats. Obesity Research 1995 3 (Suppl. 3) 339s.
- Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Yet al. Leptin levels in human and rodents: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nature Medicine 1995 1 1155–1161.
- Kolacynski JW, Nyce MR, Considine RV, Boden G, Nolan JJ, Henry R et al. Acute and chronic effect of insulin on leptin production in humans: studies in vivo and in vitro. Diabetes 1996 45 699–701.
- Ostlund REJ, Yang JW, Klein S & Gingerich R. Relation between plasma leptin concentration and body fat, gender, diet, age, and metabolic covariates.Journal of Clinical Endocrinology and Metabolism 1996 81 3909–3913.
- Kennedy A, Pan Q & Garvey T. The metabolic significance of leptin in humans: gender-based differences in relationship to adiposity, insulin sensitivity, and energy expenditure. J Clin Endocrinol Metab 1997 82 1293-300.
- Perry HM, Morley JE, Horowitz M, Kaiser FE, Miller DK& Wittert G. Body composition and age in African-American and Caucasian women: relationship to plasma leptin levels. Metabolism 1997 46 (12) 1399-405.
- Van Gaal LF, Wauters MA, Mertens IL, Considine RV& De Leeuw IH. Clinical endocrinology of human leptin. Int. J. Obese Relat. Metab. Disord 1999 23 29-36.
- Baig M, Karira KA, Ahmed A, Niaz K & Kamal S. Serum Leptin level in Hyperthyroid Female Patients. JPMA 2003 53 176.
- Wabitsch M, Jensen PB, Blum WF, Christoffersen CT, Englaro P, Heinze E, et. al. Insulin and cortisol promote leptin productionin cultured human fat cells. Diabetes 1996 45 1435-8.
- Baumgartner RN, Walters DL, Morley JE, Patrick P, Montoya GP & Gary P. Age-related changes in sex hormones affect the sex difference in serum leptin independently of changes in body fat. Metabolism 1999 48 378–84.
- Rosembaum M & Leibel R. Role of gonadal steroids in the sexual dimorphism in body composition and circulating concentrations of leptin. J Clin Endocrinol Metab 1999 84 1784–9.
- Vettor R, De Pergola G, Pagano C, Englaro P, Laudadio E, Giorgino F, et al. Gender differences in serum leptin in obese people. Relationships with testosterone, body fat distribution and insulin sensitivity. Eur J Clin Invest 1997 27 (12) 1016–24.
- Blaak E. Gender differences in fat metabolism. Curr Opin Clin Nutr Metab Care 2001; 4: 499-502.
- Hube F, Lietz U & Igel M. Difference in leptin mRNA levels between omental and subcutaneous abdominal adipose tissue from obese humans. Horm Metab Res 1996 28 690-93.



