Arsenicosis: Health Crisis and Social Consequences in Rural Bangladesh
Farhana Rahman1, 2, Saidul Alam3, S. M. Nazmul Hassan1, Muhammad Ali Akond4, *
1Integrated Community Based Arsenic Mitigation Project (ICBAMP), NGO Forum for Public Health, 4/6, Block-E, Lalmatia, Dhaka, Bangladesh
2Appartment No. 1405, Building No. 20, Japan Garden City, Mohammadpur, Dhaka
3Customs, Excise & VAT Commissionerate, Dhaka (South), National Board of Revenue, Dhaka, Bangladesh
4Lab of Microbiology, Department of Botany, Jahangirnagar University, Dhaka, Bangladesh
Abstract
This report unearths rural scenario in Bangladesh at existing perspectives of arsenic contamination in terms of health crisis and health seeking behavior, traditional remedial practices, social behavior and implications at multidimensional magnitude; and the underlying factors influencing all these parameters to aid policy making to address the crisis more efficiently. The study addressed 186 arsenicosis patients belonging to 83 arsenic affected villages of 3 districts in Bangladesh through a special and conventional interrogation. Females (56.99%) are more susceptible to arsenicosis compared to males (43.01%) and most of arsenicosis patients (28%) are illiterate. Symptoms as toxicity effects of arsenicosis patients found were white (27%) and black (31%) spots in body and palm and/or sole thickening and roughness (21%). Severe unavailability of proper treatments and enormous social fallout creating mental burden of arsenicosis patients have been exposed in this exploration. The arsenic hazard has posed a strong social dimension disrupting harmony within families and societies and created extreme instability in the social life of patients causing ostracism, marital problems, gender discrimination, increased poverty and death in the arsenic-prone areas of Bangladesh. The upsetting situation of arsenic crisis needs to be addressed immediately for effective national policy, especially for arsenic prone areas of Bangladesh. A motivational program to restore normal individual and social life as well in response to arsenicosis is immediate need.
Keywords
Arsenicosis, Health Problem, Social Crises, Rural Area, Bangladesh
Received:August 6, 2016
Accepted: August 29, 2016
Published online: September 8, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
A health catastrophe from arsenicosis and its health seeking behaviors have gradually been unfolding in Bangladesh where millions of people drink groundwater with arsenic above the permissible limit (10 µg/l) as recommended by World Health Organization (WHO) as well as the standard limit (50 µg/l) set by the Government of Bangladesh. Arsenic in groundwater, used mainly for drinking purpose, was first detected in Bangladesh in 1987, and the physical manifestations of arsenicosis was first identified in 1994 [1]. Adverse health effects from drinking arsenic contaminated water results skin depigmentation and different types of skin and internal cancers [2], increase in prevalence of diabetes, hypertension and respiratory illness [3, 4, 5]. An increased risk of spontaneous abortion and stillbirth from chronic exposure to arsenic in drinking water has also been reported [6]. Moreover, people with arsenicosis are strongly related with mental health [7]. It has been reported that 62 districts (out of the 64) in Bangladesh are affected with high level of arsenic contamination in ground water. Approximately 50 million people of the country are currently exposed to high level of arsenic (>10 µg/l) in drinking water. Very recently all the wells in 270 arsenic affected Upazilas (administrative area of local government) have been screened by the Bangladesh Arsenic Mitigation and Water Supply Project [8]. Results show that 29.12% of the total tube wells (1,440,409 tube wells out of 4,946,933) were contained with arsenic above >50 µg/l.
Disease resulted from chronic arsenic exposure is commonly known as arsenicosis. Early symptoms of arsenicosis include various skin lesions (cancers) that develop over an incubation period of 5-10 yrs of continuous exposure. After 10-20 yrs of prolonged exposure, afflicted persons often develop arsenic-related cancers [9]. Although no specific treatment of arsenicosis has yet proved to be effective, patients experiencing arsenic poisoning tend to seek treatment from health professionals. Use of antioxidant multivitamins (Vitamins A, C, and E), various skin lotions, and drinking arsenic-free water have been shown to be beneficial in some extent for the people who are in the initial stages of arsenicosis [10]. Eating selenium-rich foods, such as fresh fruits, vegetables, eggs and milk, also help to reduce the effects of arsenicosis symptoms [11]. Arsenic patients who are in the advance stages may require surgical interventions if they suffer from gangrene and arsenic-related cancers.
World Health Organization [12] listed the symptoms of arsenicosis roughly in successive order as changes of skin color (either hyper-pigmentation or depigmentation), thickening of skin particularly on the palms and soles (keratosis), skin lesions, skin and internal cancers, peripheral vascular disorders, and neurological disorders. The liver and lung may also become affected [13,14]. Arsenic poisoning also affects the productivity of the sufferers, and its debilitating nature may disrupt their family harmony. Although it has been long enough of the first report on ground water arsenic contamination, yet till now many of the people drinking this contaminated water are not aware of its consequences. Countless future generation is still gravely at risk from arsenic contamination in addition to thousands of present arsenicosis patients. According to the Bangladesh Government statistics, number of identified arsenicosis patients are 38,430 [8]. But the actual magnitude of the problem and upcoming future burden is very difficult to scale up and therefore this study is just an endeavor towards touching the tip of the iceberg in capturing the entire scenario in a single frame. Yu et al. [15] predicted that there are some two million cases of skin lesions in the country caused from drinking arsenic contaminated water, and 3,000 people die every year in Bangladesh from arsenic-related illnesses.
The overall objective of the study was to find out the perception of individuals exposed to elevated level of arsenic in rural Bangladesh and the practice they followed and to identify the underlying factors for such behavior with present target of addressing i) identification of socio-demographic status of the arsenicosis patients, ii) the perception about arsenicosis disease among the rural peoples in Bangladesh, iii) identification of traditional practices followed to manage the disease, and iv) finding out the loopholes of existing medical facilities for arsenicosis patients in rural area which might be helpful in effective decision making to handle the crisis more efficiently.
2. Methodology
2.1. Data Collection
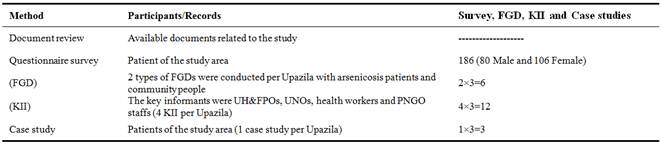
This is a descriptive cross sectional study. Data used in this study were from primary sources. Data collection was based on respondent (confirmed arsenicosis patients) answers to questionnaire surveys completed by enumerators in four unions of Bangladesh. Qualitative methods, such as informal discussions with people who suffered from arsenic poisoning and community people, were used for this study (Table 1).
Table 1. Methods used in Data Collection.
2.2. Field Survey
The methodology for this study included practical field observation and field level data collection through interviews in formal and non-formal ways. The primary data for this study were mainly collected from Integrated Community Based Arsenic Mitigation Program (ICBAMP) Project, NGO Forum for Drinking Water Supply and Sanitation (DWSS). In order to fulfill the aims and objectives, the research was divided into two phages; i) data collection and ii) data analysis. The quantitative data were collected from questionnaires survey with different arsenicosis patients and in-depth interviews with different stake holders, whereas qualitative data were collected through focus-group discussions and key informant interviews with different group allow a greater depth of understanding about the health seeking behaviors that followed by the arsenicosis patients in the severely arsenic affected areas in rural Bangladesh.
2.3. Study Area
Some highly arsenic contaminated areas (Upazilas) were selected for this study where ICBAMP project has been implementing and have at least 60 arsenicosis patients per district. These Upazilas were listed in accordance to their geographical location, arsenicosis patients’ burden and arsenic contamination rate. We selected Comilla district as high arsenic concentrated area, and Jhenaidah and Pabna as low arsenic concentrated areas [16]. The selected areas for this study are Barobazar Union of Kaliganj Upazila under Jhinaidah district, Ruppur & Masumdia Unions of Bera Upazila under Pabna district and Kandirpar Unin of Laksham Upazila under Comilla district. These four Unions cover 83 villages. The total number of arsenicosis patients in 4 Unions was 437 and among those patients, 186 patients were studied for this research.
2.4. Case Definition and Classification
Arsenicosis may be defined as a chronic condition due to prolonged (for more than 6 months) exposure of arsenic above the safe level (0.05 mg/l) usually manifested by characteristic skin lesions with or without involvement of internal organ and malignancies.According to WHO guideline the case classification of arsenicosis are-
I) Suspected: A Suspected case is a subject who shows characteristic skin lesions or pigmentary changes or keratosis on first presentation, and who has not undergone in-depth medical examination or laboratory testing.
II) Probable: A Probable case is a suspected case that has undergone further clinical examination and belongs to one of the two following category-
1) A suspected case showing melanosis and bilateral keratosis involving palms and soles.
2) A suspected case showing unilateral melanosis or keratosis after excluding other skin lesions mimicking arsenicosis.
III) Confirmed: A clinically compatible/confirmed case is a probable case in which the presence of other arsenicosis stimulating skin lesions was ruled out by differential in-depth skin examination by either a trained dermatologist or an arsenic expert.
2.5. Diagnosis of Arsenicosis
Diagnosis of arsenicosis is a prolonged process. Different steps are available to maintain the process. A diagnostic algorithm for arsenicosis case detection provides a simplified scheme for implementing the case definition and classifying patients under field conditions and in various levels of health care facilities. The suggested algorithm is shown in Figure 1.
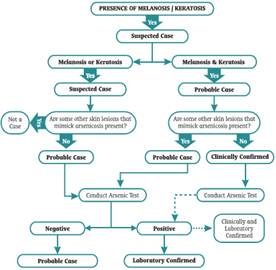
Figure 1. Flowchart of case definition algorithm for arsenicosis
2.6. Estimation of Sample Size and Data Analysis
Alternatively we calculated sample size by EPI info software version 3.2.2. With 95% confidence level, 80% power, and percentage of disease among exposed group 10%, calculated sample size was 186. All collected data and information were analyzed using statistical software SPSS (version 11.9 for Windows). In data analysis, available and necessary tools and techniques were used to have both qualitative and quantitative outputs.
3. Results and Discussion
3.1. Distribution of Different
Socio-economic Characteristics of the Arsenicosis Patients in the Study Areas
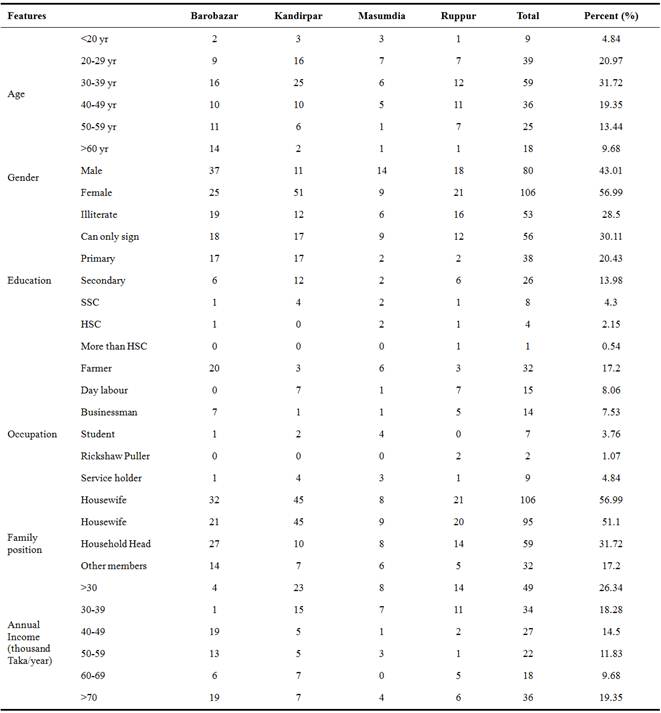
Arsenicosis is a widespread problem in Bangladesh. The country is now facing not only a major environmental concern, but also social behavior and critical health hazard from arsenic problem in the ground water. The extent of arsenicosis differs greatly between age group and gender. Most of the arsenicosis patients in the study areas were between 30-39 yrs age (31.72%). The extent of arsenicosis among the people of below 20 yrs or more then 60 yrs old is significantly lower (between 4.84% and 9.68%) than the other age groups (Table 2).
Table 2. Socio-economic characteristics of the patients in the study area.
It might be related to the diet of age groups, especially the water intake. People may intake water directly (intake of water as drinking behavior) or indirectly (intake of water used for cooking foods) [17]. The standard of direct water consumption by adults, according to the WHO recommendation, is 2 l/d [15]. Water intake differs greatly from country to country and locality to locality as well as sex and age. It has been reported that Taiwanese male and female (weighing 55 and 50 kg, respectively) intake 3.5 and 2.01 liter of water/d, respectively as direct drinking [18,19]. In tropical countries like Bangladesh (and also in other South Asian countries), water intake is normally higher then other countries. It was reported that the average direct intake of water by the population of West Bengal, India is 4, 3, and 2 l/d for male, female, and children, respectively [20]. The researchers also speculated that those who work in the field might drink as much as 6 l/d. Most of the arsenic affected areas of Bangladesh are villages, and the people of those areas are involved in agrarian manual labor. Therefore the daily direct water intake by an adult (between 20 and 49 yrs) ranged between 4 and 6 l/d [21].
From the survey it was observed that the female (56.99%) were more susceptible to arsenicosis than the male (43.01%) (Table 2). The reasons behind this are not clear at all. However, in Bangladesh and other South Asian countries the females are more subjected to malnutrition compared to the male. Therefore, it is predicted that the higher number of arsenicosis patients among the female is due to malnutrition.
Not only gender but also the educational status was found to be correlated to the extent of arsenicosis in the rural areas of Bangladesh. Among the arsenicosis patients, most of them (28%) had no formal education, and 31% could sign only. More importantly, only between 0.5%-4.3% of the total arsenicosis patients were educated (completed secondary education) (Table 2). The results suggest that the scope of arsenicosis is significantly higher among the illiterate people compared to those of educated. This might be because the educated people know well about the arsenic problem and are more aware of the disease (arsenicosis). They are more conscious about their health and to take control measures or medical treatments of the disease in time. On the other hand, illiterate people don’t know about arsenic and its health effects in most cases. They don’t know how to take control measures of arsenic disease and delay to take or don’t take appropriate medical treatments very often.
The scope of arsenicosis among the population of the study areas was evaluated in this study. The result showed that socio-economic conditions are one of the important determinants for arsenicosis disease. The highest number of arsenicosis patients was farmer (17.2%) followed by day labor (8.06%), Businessman (7.53%), Serviceman (4.48%), and Student (3.76%) (Table 2).
From the above data it is noted that the risk of arsenicosis is correlated between the educational status and socio-economic condition of the people. Farmers of rural Bangladesh are mostly illiterate and the highest number of arsenicosis patients is highest in them.
The position of arsenicosis patients in the family was also investigated in this study. About 31% arsenicosis patients were the key earning person (mainly male) in the family of the study area. On the other hand 51% of the patients were house wife (data not shown). From these findings it is quite clear that females are more venerable to arsenicosis compared to males.
3.2. Source of Drinking Water for the Rural People of the Study Areas
Still now, people in the study area used pond water (1%) as a source of drinking water without any treatment, which is a threat for creating hazardous effect on human health. In our study area, about 36% and 31% respondents used water from shallow tube wells and deep tube wells, respectively, and among those tube wells, about 20% tube wells were red marked (arsenic contaminated). This is a great threat for the people of rural Bangladesh not to get safe water for drinking. The women and children of the rural Bangladesh are generally collect safe water for other family members. Therefore, this places extra burden on their time and energy in order to fetch water from fewer safe sources. If the safe water sources are too far from the house, or troublesome, they are likely to procure water from nearby tube wells, even though the tube wells were contaminated [22,23]. Still now, safety level of arsenic in drinking water sources was not screened in about 12% tube wells, which is a great threat to the people of rural Bangladesh who use these water sources, and 62% of the patients in the study area did not know the arsenic safety level of their drinking water.
3.3. Symptoms of Arsenicosis Observed in the Body of the Patients
The poisoning that is taking place in Bangladesh through arsenic-contaminated groundwater is chronic in nature. Of the various sources of arsenic in the environment, drinking water probably poses the greatest threat to human life. The most common effects of arsenic include gradual loss of strength, pigmentation and scaling of the skin, degeneration of faulty tissue, white and black spot in the body, thickening and roughness of the palm/sole, and the development of characteristic streaks across fingernails. It may take 2 to 20 yrs for a person exposed to arsenic to develop the symptoms of arsenicosis. The period differs from patient to patient depending on the amount of arsenic ingested, nutritional status of the person, immunity level of the individual, and the total time period of arsenic ingestion. Our study shows that most of the patients had first stage arsenicosis symptoms such as black spot in the body (31%), white spot in the body (27%), thickening and roughness of the palm/sole (21%), body ache (7%), and weakness (7%) (Table 3).
Table 3. Distribution of different symptoms of the respondents.
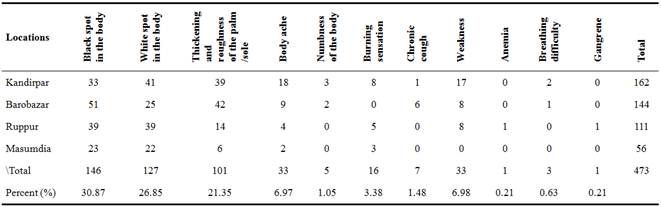
Early effects of exposure to arsenic in drinking water include pigmentation changes and hyperkeratosis [24,25], which reportedly appear after 5–10 yrs of exposure [26]. These skin lesions may develop into more serious and disabling forms, including cancer [24,26,31].
Smith et al. [25] stated that pigmentation changes may be hyper or hypo colored. For example, among those consuming 263-864 μg/l of arsenic in their drinking water, the prevalence of skin lesions for men is well over 20/1000, but the prevalence for women is only slightly over 5/1000. This hyper pigmentation or melanosis may occur anywhere in the body, especially marked on the non-exposed parts of the body. Leucomelanosis (hypo pigmentation) follows the same distribution and may be present even in the absence of melanosis [32]. Arsenic-related skin lesions and the other non-cancerous conditions caused by arsenic contamination have a latency period of about 5–10 yrs, whereas the latency period for arsenic-related cancers is about 20–30 yrs toxicity may be used as an indicator of high exposure and are quite distinctive [33]. Over 70 million people are estimated to be in risk of arsenic exposure [25].
3.4. Steps Toward the Control Arsenic Crisis in Rural Bangladesh
The supply of safe water is one of the most important determinants of health and socioeconomic development. For human consumption, water should be both safe and wholesome. Without ample safe drinking water, communities cannot be healthy. For a developing country like Bangladesh, where the majority of the people live below the poverty line in the rural area, the provision of safe drinking water is one of the prior conditions for overall social development. To avoid the problem of arsenic crisis, we must stop intake of arsenic contaminated water. From this study, we found that only about 19% people stopped intake of arsenic contaminated water but rest of the people (about 81%) still using the arsenic contaminated water. This is because of the unavailability of safe water, lack of awareness, and ignorance of the fact of arsenicosis. However, medical facilities for the patients of rural Bangladesh will not be reasonable because of high poverty.
At present, the government of Bangladesh, development partners, and non-governmental organizations (NGOs) have come forward to control the arsenic crisis in rural Bangladesh. They initiated a number of projects including screening and labeling of tube wells, building mass awareness among the people of affected areas about arsenic contamination and related diseases, developing appropriate and cost-effective arsenic mitigation measures, and identifying alternative sources of safe drinking water. In our study areas we found that about 86% of the arsenicosis patients were identified by health workers of NGOs, whereas only 5% were identified by Government health workers. Among the arsenicosis patients, about 90% patients were consulted with physicians after the identification of arsenic related symptoms in their body. Some of them (about 4%) only discuss about their illness with relatives/friends, and about 7% of the patients keep it secret (data not shown). However, in most cases the arsenicosis patients delay to consult with doctors/physicians about their illness. Most of the patients (about 66%) did not know what to do with arsenicosis symptoms though few of them (about 18%) understand lately (data not shown). These were the reasons to delayed consultation with the physician. More importantly, about 13% of the patients ignored the symptoms of arsenicosis though they know its circumstances.
In this study, we observed that 42% of the patients visited NGO clinics for medical treatments whereas only 27% visited government facilities (district and sub-district hospitals). The alarming news is that 45% of the patients did not visit any medical facilities to take treatments (Table 4).
Table 4. Medical facilities taken by the arsenicosis patients in the study areas.
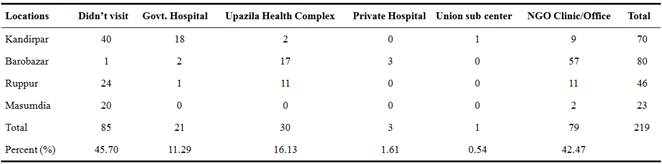
Most of the patients (74%) answered that vitamins were provided for their arsenicosis disease, and ointment & rex were provided to 23% and 2% patients, respectively. After given medical treatments to the arsenicosis patients, the health condition of 38% patients gradually improved, but 15% patients were unchanged and 1% patients were deteriorated. All of the respondents think that arsenic poisoning is a serious threat to their life.
Most of the patients (about 35%) in this study answered that they got awareness about arsenic related diseases from NGO workers, television (24%), and radio (10%). Few people (about 10%) also got information about arsenic and arsenic related health hazards from their neighbors (Table 5).
Table 5. Awareness rising sources among the people of arsenic affected areas of Bangladesh.
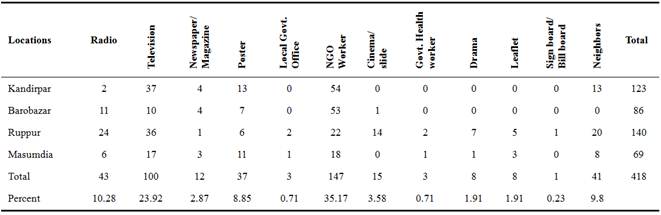
Many development projects of the government and NGOs are trying to increase public awareness in order to address this massive water supply and public health problem [21,34,35]. The alternative safe water options in the rural area are insufficient. Therefore, it is likely that the people of arsenic affected areas of Bangladesh will continue to use arsenic contaminated water rather than the safe sources [36].
There were some problems of current medical facilities for getting arsenicosis treatment in the study areas. Most of the people were happy to get medicine in home but they recommended that regular medicine supply should be ensured. About 22% to 26% of the patients think that loan should be provided to them for getting better treatment and to buy nutritious food (Table 6).
Table 6. Recommendations proposed by the patients for medical facilities to get better treatment of arsenicosis.
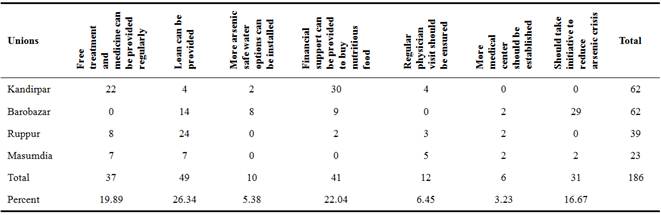
So, it is urgent to solve the limitation of existing medical treatments and must to ensure the availability of medical facilities for the patients of arsenicosis.
3.5. Social Facts of Arsenicosis Patients in Rural Bangladesh
Arsenic is not only a physical but also a social phenomenon. Lack of proper knowledge about arsenic related diseases, unavailability of safe drinking water as well as proper treatment are creating extreme instability in the social life of the people in the arsenic affected areas of Bangladesh. Moreover, social conflict over contaminated water contributes to destruction of social harmony and network relationships. Superstitions and prejudices are constructed surrounding arsenic patients. People think that it is a contagious disease and thus they stay away from arsenic victims, neglect them, or become scared of them [37]. The patients as well as their close relatives are not allowed to use public tube wells and village ponds. As a result, arsenic affected people are closely related to mental disorders [38,39]. Very often family members, like husbands or wives, abandon the arsenicosis victims. Arsenic has an adverse impact on marital relationships. People are reluctant to develop marital relationships with families whose members suffer from arsenicosis. This has caused serious anxiety for parents of unmarried adult children. Many women are divorced or abandoned by their husbands due to arsenicosis. Women are frequent victims of ostracism due to arsenicosis. Women are doubly vulnerable: from the disease itself and by being divorced, abandoned, or even forced out of the society. As gender discrimination exists in many forms in the patriarchal society of Bangladesh, women suffer more from these things than men [40]. This study reported many women victims of arsenicosis disease getting divorced and faced many other social obstacles. The common scenario in many families is that if the male member had arsenicosis, his wife nurses him. But if the wife had arsenicosis, her husband does not even come to her, and rather divorce her ruthlessly.
Those people live in poverty are the main victims of arsenic contamination as they are compelled to drink contaminated tube well water. Researchers believe that the severity of arsenicosis is very much related to nutritional deficiency [6]. Malnutrition makes them easy victims. Due to poverty, victims are deprived of proper treatment. Not only the poor people affected mostly by arsenicosis, but also arsenic-related weakness and illness causes further economic damage as the people suffering from arsenicosis are increasingly unable to work [41]. Among poor families, adults are reluctant to take medical treatment because their families cannot manage without their daily pay. When seeking treatment, the costs become a burden to them. A group of low-income patients sent one person to the sub-district health centre (a government hospital) to collect monthly medicines for all, because the travel costs were too difficult to bear [2,42]. Some families are rendered destitute when their earning members die of arsenic-related disease. Most field workers in highly affected areas have seen and reported that people living and dying under such unfortunate circumstances [43]. As arsenicosis decreases the victim’s working ability, his or her income decreases. Due to ostracism, arsenic patients lose their jobs too. Thus, arsenic negatively contributes to the poverty situation in Bangladesh.
The time constrain is one of the most important limitation of this study. This study is not the representative of all arsenicosis patients in all arsenic affected villages of Bangladesh. So, studies regarding the health crisis and social consequences of arsenicosis patients in all arsenic affected areas would be required to know the real scenario of the country.
4. Conclusions
The academic as well as research institutes should take appropriate measures to assess the cause and impact of arsenic poisoning and to take remedial measures whenever and wherever necessary. It is now apparent that groundwater must undergo analysis for arsenic before it is used for drinking and cooking purposes. The arsenic problem in Bangladesh and elsewhere has decidedly pointed out that water quality should be surveyed and included in all water development and distribution program. The presence of arsenic in drinking water has also indicated that more research work is necessary to deter the potential health effects emerging from other inorganic elements present in water resources and to make available suitable and affordable safe water technologies. It is urgent to aware the rural people against arsenicosis to ensure arsenic-free community in Bangladesh. The knowledge of the study helps people to understand the routine testing of drinking water which is important for maintaining healthy life from arsenicosis. In addition, regular checkup of arsenicosis patients is also essential to sustain clinical practice. The study helped to understand one of the emerging public health issues in Bangladesh. It also creates the scope of thinking about the future work in the arena of arsenic crisis. Moreover, it will help the policy makers to take decision to improve healthcare facilities in rural Bangladesh.
Acknowledgement
The authors are grateful to Integrated Community Based Arsenic Mitigation Project (ICBAMP) of the NGO Forum for Public Health, Lalmatia, Dhaka-1207, Bangladesh and European Union & MISEREOR who provided the financial support for the project.
References
- Ahmad SA, Akhtar SK, Sayed MHSU, Hadi SKA, Faruquee MH, Khan MH, Jalil MA, Ahmed R, Khan AW. Arsenicosis in a village of Bangladesh. Int. J. Environ. Health Res., 1999; 9: 187-195.
- World Health Organization (WHO): Towards an Assessment of the Socioeconomic Impact of arsenic Poisoning in Bangladesh. Geneva (Switzerland): WHO; 2000.
- Parvez F, Chen Y, Yunus M, Olopade C, Segers S, Slavkovich V, Argos M, Hasan R, Ahmed A, Islam T, Akter MM, Graziano JH, Ahsan H. Arsenic Exposure and Impaired Lung Function. Findings from a Large Population-based Prospective Cohort Study. American Journal of Respiratory and Critical Care Medicine, Vol. 188, No. 7 (2013), pp. 813-819. doi: 10.1164/rccm.201212-2282OC.
- Milton AH, Rahman M. Respiratory Effects and Arsenic Contaminated Well Water in Bangladesh. Int. J. Environ. Health Res., 2002; 12: 175-179.
- Naujokas MF, Anderson B, Ahsan H, Aposhian HV, Graziano JH, Thompson C, Suk WA. The broad scope of health effects from chronic arsenic exposure: update on a worldwide public health problem. Environ Health Perspect. 2013 Mar;121(3):295-302. Epub 2012 Dec 21.
- Milton AH, Hasan Z, Shahidullah SM. Association between nutritional status and aresnicosis due to chronic arsenic exposure in Bangladesh. Int. J. Environ. Health Res., 2004; 14(2): 99-108.
- Chowdhury S, Krause A, Zimmermann KF. Arsenic Contamination of Drinking Water and Mental Health. IZA Discussion Paper No. 9400 October 2015.
- Bangladesh Arsenic Mitigation Water Supply Project (BAMWSP): Dhaka. May 2005. BAMWSP Newsletter; Available from: [http://www.bamwsp.org/Other%2520Files/newsletter%2520may_05.pdf 2005]
- Paul BK, Brock VLT. Treatment Delay Period: The case of Arsenicosis in Rural Bangladesh. Health and Place, 2006; 12(4): 580-593.
- Majumdar D, Guha N. Treatment of chronic arsenic toxicity as observed in West Bengal. J. Indian Med. Assoc., 1996; 94(2): 41-42.
- Paul BK, De S. Arsenic Poisoning in Bangladesh: A geographic Analysis. J. American Water Resources Association, 2000; 36(4): 799-809.
- World Health Organization (WHO): Arsenic in drinking water. Facts sheet No 210. Geneva (Switzerland): WHO; February 1999.
- Abernathy CO, Calderon RL, Chappell WR. Arsenic: Exposure and Health Effects. London: Chapman and Hall, Co.; 1997.
- Mazumder GDN, Gupta JD, Santra A, Pal A, Ghose A, Sarkar S, Chattopadhaya N, Chakraborti D. Non-cancer effects of chronic arsenicosis with special reference to liver damage. In Arsenic: Exposure and Health Effects. Abernathy CO., Calderon RL, Chappell WR, Editors. London: Chapman and Hall, 1997; pp. 112-123.
- Yu WH, Harvey CM, Harvey CF. Arsenic in groundwater in Bangladesh: a geostatistical and epidemiological framework for evaluating health effects and potential remedies. Water Res., 2003; 39(6): 1146-1162.
- NGO Forum for Drinking Water Supply and Sanitation Bangladesh: ICBAMP in 100 Unions of Bangladesh. 2007. Baseline Survey Report; 4/6 Block-E, Lalmatia, Dhaka-1207, Bangladesh.
- Rahman MA, Hasegawa H, Rahman MA, Rahman MM, Miah MAH. Influence of cooking methods on arsenic retention in cooked rice related to dietary exposure. Sci. Total Environ., 2006; 370: 51-60.
- Levallois P, Guevin N, Gingras S, Levesque B, Weber JP, Letarte R. New patterns of drinking-water consumption: results of a pilot study. Sci. Total Environ., 1998; 209: 233–241.
- Abernathy CO, Marcus W, Chen C, Gibb H, White P.Internal Memorandum to P. Cook/P. Preuss:Report on Arsenic (As) Work Group Meetings. USEPA, Office of Drinking Water, Washington, DC. February 23, 1989.
- Brown K, Abernathy C. The Taiwan skin cancer risk analysis of inorganic arsenic ingestion: effects of water consumption rates and food arsenic levels. In Arsenic: exposure and health effects. Abernathy Co, Calderon R, Chappel RW, Editors. London: Chapman and Hall, 1997. p. 260–271.
- Chowdhury UK, Biswas BK, Chowdhury TR, Samanta G, Mandal BK, Basu GC. Groundwater arsenic contamination in Bangladesh and West Bengal. Environ. Health Perspec., 2000; 108: 393–397.
- Alam MGM, Allinson G, Stagnitti F, Tanaka A, Westbrooke M. Arsenic Contamination in Bangladesh Groundwate: A Major Environmental and Social Disaster. In.t J. Environ. Health Res., 2002; 12 (3): 235–253.
- BRAC: Combating a deadly menace: early experience with a community based arsenic mitigation project in Bangladesh. June 1999 - June 2000. BRAC Research Monograph Series No. 16. BRAC Research and Evaluation Division: Dhaka, Bangladesh; 2000.
- Jakariya, M. The use of alternative safe water option to mitigate the arsenic problem in Bangladesh:community perspective. BRAC Research Monograph Series No. 24. BRAC Research and Evaluation Division, Dhaka, Bangladesh; 2003.
- InternationalAgency for Research on Cancer (IARC): Some Drinking-Water Disinfectants and Contaminants, including Arsenic Related Nitrosamines. IARC Monogr Eval Carcinog Risks Hum., 2004; 84: 1-512.
- Smith AH, Lingas EO, Rahman M. Contamination of drinking water by arsenic in Bangladesh: A public health emergency. Bulletin of the World Health Organization, 2000; 78(9): 1093-1103. [http://www.who.int/bulletin/pdf/2000/issue9/bu0751.pdf ]
- Mazumder GDN, Haque R, Ghosh N, De BK, Santra A, Chakraborty D. Arsenic levels in drinking water and the prevalence of skin lesions in West Bengal, India. Int. J. Epidemiol., 1998; 27(5): 871–877.
- Haque R, Mazumder DN, Samanta S, Ghosh N, Kalman D, Smith MM. Arsenic in drinking water and skin lesions: dose-response data from West Bengal, India. Epidemiol., 2003; 14(2): 174–182.
- NRC (National Research Council): Arsenic in Drinking Water, 2001 Update. Washington DC, National Academy Press, 2001.
- Tondel M, Rahman M, Magnuson A, Chowdhury IA, Faruquee MH, Ahmad SA. The relationship of arsenic levels in drinking water and the prevalence rate of skin lesions in Bangladesh. Environ. Health Perspect., 1999; 107: 727–729.
- Tseng WP. Effects and dose–response relationships of skin cancer and black foot disease with arsenic. Environ. Health Perspect., 1997; 19: 109–119.
- World Health Organization (WHO)/International Programme on Chemical Safety (IPCS): Arsenic and Arsenic Compounds. Environmental Health Criteria 224. 2nd ed. Geneva (Switzerland): WHO; 2001.
- Milton AH, Rahman M. Environmental pollution and skin involvement pattern of chronic arsenicosis inBangladesh. J. Occup. Health, 1999; 41(4): 207-208.
- CaldwellBK, Smith W, Caldwell JC, Mitra SN. Searching for an Optimum Solution to the Bangladesh Arsenic Crisis. J. Social Science and Medicine, 2003; 56(10): 2089-2096.
- Hadi A. Fighting Arsenic at the Grassroots: experience of BRAC’s community awareness initiative in Bangladesh. Health Policy and Planning, 2003; 18(1): 93-100.
- Jakariya M, Chowdhury AMR, Hossain Z, Rahman M, Sarker Q, Khan RI, Rahman M. Sustainable community-based safe water options to mitigate the Bangladesh arsenic catastrophe-an experience from two upazilas.Current Science., 2003 ; 85(2) : 141-146.
- George, C. M., Factor-Litvak P, Khan K, Islam T, Singha A, Howard JM, Geen A, Graziano JH. Approaches to Increase Arsenic Awareness in Bangladesh: An Evaluation of an Arsenic Education Program. 2013. Health Education & Behavior; 40(3), 331–338.
- Tyler, C. R., Allan AM. The Effects of Arsenic Exposure on Neurological and Cognitive Dysfunction in Human and Rodent Studies: A Review. Current Environmental Health Reports.,2014; 1(2), 132–147
- Hossain, M. D., Ahmed HU, Chowdhury WA, Niessen LW, Alam DS. Mental disorders in Bangladesh: a systematic review.2014. BMC Psychiatry, 14:216.
- Jack CN, Jianping W, Amjad S. A global health problem caused by arsenic from natural sources. Chemosphere, 2003; 52 (9): 1353-1359.
- Ahmad SA, Sayed MHSU, Barua S, Khan MH, Faruquee MH, Jalil A, Hadi SKA, Talukder HK. Arsenic in drinking water and pregnancy outcomes. Environ. Health Perspect., 2001; 109: 629–631.
- UnitedNations International Children's Emergency Fund (UNICEF): Arsenic Mitigation in Bangladesh. Dhaka; 1999.
- ChakrabortiD, Biswas BK, Roy Chowdhury T, Basu GK, Mandal BK, Chowdhury UK, Mukherjee SC, Gupta JP, Chowdhury SR, Rathore KC. Arsenic groundwater contamination and sufferings of people in Rajnandgaon district, Madhya Pradesh. India. Current Science, 1999; 77: 502–504.