A Case of Cutaneous Myiasis Caused by a Larva of Cordylobia anthropophaga in a Nine Year Old Boy in Calabar, Southern Nigeria
Akpan Samuel S.*
Department of Medical Laboratory Science, College of Medical Sciences, University of Calabar, Calabar, Nigeria
Abstract
A nine year old boy presented with a furuncular swelling on one buttock with a complaint of pain and itching around the region of the lesion. With a gentle manual pressing of the swelling, a yellowish-white larva emerged. The larva was macerated in 10% potassium hydroxide solution over boiling water for 10 minutes to examine the posterior spiracles. Using the characteristic morphologic features (viz. an indistinct button, an incomplete peritreme and sinuous slits), the larva was identified as that of Cordylobia anthropophaga. This result confirmed a diagnosis of cutaneous myiasis. Conditions of squalor, poverty and ignorance facilitate the transmission of eggs and larvae from Calliphorid flies on to the human body. Awareness, personal hygiene and environmental sanitation are preventive measures which can curb the spread of this parasitosis.
Keywords
Awareness, Cordylobia, Myiasis, Parasitosis, Swelling
Received: June 14, 2016
Accepted: July 4, 2016
Published online: July 27, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Myiasis may be defined as the invasion of living tissues or organs by fly larva [1]. The term, derived from Greek (mya or fly), was first coined by The Reverend Frederick William Hope in 1840 in reference to diseases caused by dipterous larvae, to differentiate them from those caused by other insect larvae [2]. The disease has a worldwide distribution in human beings. In countries in which infections are not common, the condition ranks among the commonest imported skin diseases among travelers [3]. It is a common parasitic infection of man and also presents serious economic losses in livestock industries, including reduction in milk production, hide quality and reduced weight and fertility [4,5]. In human, this condition is usually caused by larvae of dipteran flies of the Family Calliphoridae. Examples of these flies belong to the Genera Callitroga, Chrysomyia, Cordylobia, Dermatobia, Gasterophilus, Hypoderma, Oestrus and Wohlfahrtia. Of these eight Genera, only Callitroga, Chrysomyia, Cordylobia and Dermatobia are usually found in the tropics [1]. In rural, tropical regions where these flies abound, myiasis is usually a common occurrence [6]. Travellers to endemic areas may be infected and they return to their countries of residence with exotic cases of myiasis [7,8]. The average incubation period from infection to manifestation of clinical symptoms may be up to one and a half months [9].
Human beings become infected through various means. The flies may deposit their eggs or live maggots on dirty, damp clothing or soil. Contact with larvae aids their penetration into the skin. This is usually the case in facultative myiasis. Once the larvae have been able to penetrate the skin, they bore their way into the subcutaneous tissue. The presence of larvae under the skin, with constant irritation, may lead to secondary bacterial infection. In obligatory myiasis, the larvae usually seek and penetrate a mammalian host; since the latter is required for their development and the larvae cannot complete their life cycle without their parasitic phase [10]. Mixed infections often occur, in which one person may harbour larvae of different genera; each located at different sites or organs with different clinical manifestations [11].
Many authorities have worked on the classification of myiasis. Two broad methods of classification are commonly adopted, viz., anatomical and ecological [4,12,13]. The classification of myiasis is done mostly according to the organ or part of the body which is infected. So, we can have cutaneous, nasal, aural, internal or wound myiasis [10,6,14]. External and internal ophthalmomyiasis are commonly caused by the botfly [15]. In case of ophthalmomyiasis, patients may complain of severe eye irritation, redness, foreign body sensation, pain, lacrimation, and swelling of the eyelids [16].
Important risk factors for contracting myiasis include poor hygiene, low socioeconomic status, ageing, mental disability and alcoholism [17]. Specific habits such as sitting or lying on bare floor also promote the occurrence of myiasis [18,19,20]. Certain dermatological conditions which attract dipteran flies are predisposing factors for myiasis. Such conditions include ulcers, herpes zoster virus infection, onychomycosis, leprosy, pediculosis, etc [18,21,22,23]. Urogenital infections, especially among females, have been reported among people with a recent visit to endemic areas [24]. Nosocomial myiasis is common if open wounds are infested with flies.
Myiasis is often misdiagnosed because its signs and symptoms are often vague and unspecific [6]. In deep-seated cases in which parasites are lodged deep within the tissues, surgery may be required to remove the larvae [6]. Ultrasound may be employed for a definitive diagnosis of furuncular myiasis and also remove the larvae [25,26]. Among health personnel without experience in tropical medicine, molecular diagnosis would be useful in the identification of the infecting larva [27]. Accurate diagnosis of myiasis is important in order to understand its mode of transmission and also plan appropriate treatment and preventive measures [13].
2. Case Presentation
This case was recorded in April, 2016 in Calabar Municipality Local Government Area of Cross River State in Southern Nigeria. A 9 year old boy presented with an erythematous, furuncular (boil-like) swelling on one buttock. The patient complained of pain and itching around the region of the lesion. Upon a close examination, a whitish, scab-like substance was noticed slightly beneath the punctum of the lesion [28]. The lesion was squeezed manually using two wooden spatulas to reduce the chance of rupturing the larva [29]. Only one larva emerged from the lesion. Mechanical removal and surgery are well known procedures for the extraction of maggots [19]. The lesion was non-suppurative with a serosanguinous discharge.

Figure 1. A furuncular lesion on the buttock of the patient under study.
3. Morphology of the Larva
The larva was oval in shape, yellowish-white in colour and measured about 8mm in length and 1.5mm across the last abdominal segment. The larva was immediately placed in hot (but not boiling) water for 1 minute. This initial step is critical in order to preserve the integrity and natural colour of the larva as observed by other workers [30]. It was laterpreserved in 70%alcohol for further examination at the Parasitology Laboratory of the University of Calabar Teaching Hospital.

Figurse 2. A larva of Cordylobia anthropophaga (removed from the lesion above).
4. Processing of the Larva
The larva was removed from the preservative and placed on a clean glass slide. With the aid of a scalpel blade, the posterior spiracle was cut off as a nib. It was placed in a test tube containing 2ml of 10% potassium hydroxide (KOH) solution. The test tube was placed in a beaker containing boiling water and left to stand for 10 minutes. With the aid of a Pasteur pipette, the KOH solution was carefully removed. Water was added to wash the spiracle. After removing the water, 2ml of 50% alcohol was added to dehydrate the spiracle for 10 minutes. The alcohol was removed and 2ml of 90% alcohol was added to further dehydrate the specimen for 20 minutes. Two changes of 2 ml absolute methanol were added. Each change was allowed to stand for 20 minutes for further dehydration of the specimen. After removing the alcohol, two changes of xylene were added to clear the specimen for 5 minutes each. Finally, the specimen was mounted permanently on a clean glass slide using DPX as mountant.
5. Result
The mounted specimen was examined under a microscope using10x objective lens. The specimen was identified as larva of Cordylobia anthropophaga based on the following characteristic features: the peritreme was less sclerotized and incomplete; the button was indistinct and the spiracular slits were moderately sinuous [1]. Cordylobia anthropophaga and Dermatobia hominis are the most common aetiologic agents of furuncular myiasis [13].
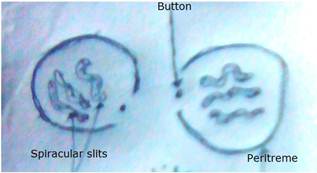
Figure 3. A diagram of posterior spiracle of Cordylobia anthropophaga.
6. Management of the Case
A topical application of FUNBACT-A was administered on the lesion. This ointment is a local application with antibacterial, antifungal and anti-inflammatory effects. The patient was given 2 tablets of Panadol (a local analgesic) to douse any pains. The lesion healed completely within 3 days without any scar or secondary bacterial infection. Oral medication, especially with antibiotics, is usually unnecessary in the treatment of cutaneous or furuncular myiasis. Topical application of 1% Ivermectin on the lesion may kill the larva in situ; but may cause an inflammatory reaction [31]. The major aim of treatment is to remove the larva intact and completely from the skin to forestall any secondary bacterial infection [19]. Generally, an early and accurate diagnosis of myiasis is important in order to alleviate the patient’s pains. Administration of antibiotics may not be necessary in all cases to avoid bacterial resistance [32].
7. Prevention and Control
Generally, all forms of myiasis may be prevented and controlled by maintaining a personal hygiene and an environmental sanitation. In deep-seated cases in which parasites are lodged deep within the tissues, surgery may be required to remove the larvae [7]. Clothing materials should be washed, dried completely under the sun and ironed before use. Ironing of clothes helps to kill any eggs or larvae which might have been deposited on the fabrics while they were hung outside to dry. Floors and walls of houses should be devoid of crevices which constitute a potential ssite for the deposition of eggs and larvae. Health education is also vital to inform people of the mode of transmission of this infection.
8. Conclusion
This work has confirmed that myiasis is a common skin disease in this part of the world. However, epidemiological data may be scanty because cases are hardly reported to health professionals who usually regard myiasis as a disease of minor importance [13]. This case was recorded in a 9 year old boy in April, which marks the beginning of the rainy season in the Southern part of Nigeria. This finding confirms the work of previous workers who observed that infestation by C. anthropophaga was particularly common among children during the rainy season [13,33,35].
References
- Gordon, R. M. &Lavoipierre, M.M.J. (1962). The Family Calliphoridae. In: Entomology for Students of Medicine: 5th Printing. Blackwell Scientific Publications. London, 189-198.
- Hope FW, 1840. On insects and their larvae occasionally found in the human body. Trans. R. Entomology. Society of London1840:256–271.
- Caumes E, et al., 1995. Dermatoses associated with travel to tropical countries—a prospective study of the diagnosis and management of 269 patients presenting to a tropical disease unit.Clin. Infect. Dis. 20:542–548.
- Zumpt F,1965. Myiasis in man and animals in the Old World. Butterworths, London, United Kingdom. 172.
- Otranto, Domenico. "The immunology of myiasis: parasite survival and host defense strategies." Trends in Parasitology 17 (2001): 4.
- John, D. & Petri, W. (2006). Markell and Voge’s Medical Parasitology 9th Edition. Missouri: Saunders Elsevier, 328-334.
- Palmieri J, North D, Santo A, 2013.Furuncularmyiasis of the foot caused by the tumbu fly, Cordylobia anthropophaga: a report in a medical student returning from a medical mission trip to Tanzania.International Medical Case Reports Journal 6:25-8.
- Fujisaki R, Makimura K, Hayashi T, Yamamura M, Yamaoka T, Shiraishi K, Ishibashi S, Kawakami S, Kurihara T, Nishiya H, 2008. Exotic myiasis caused by 19 larvae of Cordylobia anthropophaga in Namibia and identified using molecular methods in Japan.Trans R Soc Trop Med Hyg.102(6):599-601.
- Schwartz E, Gur H, 2002.Dermatobia hominis myiasis: an emerging disease among travelers to the Amazon basin of Bolivia. J Travel Med. 9(2):97-9.
- Janovy, J., Schmidt, G. D. & Roberts, L. S. (1996). Foundations of Parasitology. Dubuque, Iowa: Wm.C. Brown. ISBN 0-697-26071-2.
- Nwosu PU, Dakul DA, 2013. Report of a case of cutaneous (furuncular) and gastrointestinal myiasis (Dermatobia hominis) in a Nigerian child. West Afr J Med.32(2):149-52.
- James MT,1947. The flies that cause myiasis in man, p 1–175. U.S. Department of Agriculture miscellaneous publication no. 631. USDA, Washington, DC.
- Fabio Francesconi & Omar Lupi, 2012. Myiasis. Clinical Microbiology Review, 25:1, 79-105.
- Ockenhouse, C., Samlaska, C., Benson, P., Roberts, L., Eliasson, A., Malane, S. & Menich, M. (1990). Cutaneous myiasis caused by the African tumbu fly. Archives of Dermatology 126:199-202.
- Lagacé-Wiens, Philippe; Dookeran, Ravi; Skinner, Stuart; Leicht, Richard; Colwell, Douglas D.; Galloway, Terry D. (2008). "Human Ophthalmomyiasis Interna Caused by Hypoderma tarandi, Northern Canada". Emerging Infectious Diseases 14 (1):64–6.
- Masoodi M, Hosseini K, 2004. External ophthalmomyiasis caused by sheep botfly (Oestrus ovis) larva: a report of 8 cases. Arch Iran Med. 7:136-139. 250.
- Hutington, T., David, W. & Higley, L. (2008). Not the usual suspects: Human wound myiasis by Phorids. Journal of Medical Entomology 45,1:157-159.
- Fernandes LF, Pimenta FC, Fernandes FF, 2009. First report of human myiasis in Goias State, Brazil: frequency of different types of myiasis, their various etiological agents, and associated factors. J. Parasitol. 95:32–38.
- Francesconi F, Lupi O, 2006. Myiasis, p 232–239. In Tyring SK, Lupi O, Hengge UR (ed.), Tropical dermatology. Elsevier, Philadelphia, PA210.
- Fujisaki R, et al., 2008. Exotic myiasis caused by 19 larvae of Cordylobia anthropophaga in Namibia and identified using molecular methods in Japan. Trans. R. Soc. Trop. Med. Hyg. 102:599–601.
- Balcioglu IC, Ecemis T, Ayer A, Ozbel Y,2008. Sub-unguial myiasis in a woman with psychiatric disturbance. Parasitol. Int. 57:509–511.
- Murthy SC, Udagari MM, 2003. Myiasis complicating herpes zoster in an immuno-compromised patient. Indian J. Dermatol. Venereol. Leprol. 69:
- Marquez AT, Mattos MD, Nascimento SB, 2007.Myiasis associated with some socioeconomic factors in five urban areas of the State of Rio de Janeiro. Rev. Soc. Bras. Med. Trop. 40: 175–180.
- Kovaleva A, Climent PC, Bécare CV, Martín Azaña MJ, Irishina N, Goy EI, (2013). Urogenital myiasis by Cordylobia anthropophaga. J Pediatr Adolesc Gynecol. 26(6):e123-5.
- Schechter E, Lazar J, Nix ME, Mallon WK, Moore CL, 2008. Identification of subcutaneous myiasis using bedside emergency physician performed ultrasound. J. Emerg. Med. 40:e1–e3 334.
- Szczurko C, et al., 1994. Ultrasonography of furuncular cutaneous myiasis: detection of Dermatobia hominis larvae and treatment. Int. J. Dermatol. 33:282–283.
- Buettner H, 2002. Ophthalmomyiasis interna. Arch. Ophthalmol. 120:1598–1599.
- Adisa, C. & Mbanaso, A. (2004). Furuncular myiasis of the breast caused by the larvae of the tumbu fly (Cordylobia anthropophaga) BMC Surgery 4:5.
- O'Rourke FJ,1954. Furuncular myiasis due to Wohlfahrtia vigil (Walker). CMAJ 71:146–149.
- Mariwalla K, Langhan M, Welch KA, Kaplan DH, 2007. Cutaneous myiasis associated with scalp psoriasis. J. Am. Acad. Dermatol. 57:S51–S52.
- Quintanilla-Cedillo MR, Leon-Urena H, Contreras-Ruiz J, Arenas R, 2005. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int. J. Dermatol. 44:34–37.
- Noutsis C, Millikan LE. 1994. Myiasis. Dermatol. Clin. 12:729–736.
- Blacklock B, Thompson MG, 1923. A study of the tumbu-fly Cordylobia anthropophaga Grunberg in Sierra Leone. Trop. Med. Parasitol. 17:443–502.
- Gunther S,1971. Clinical and epidemiological aspects of dermal tumbu-fly myiasis in Equatorial Africa. Br. J. Dermatol. 85:226–231.
- Kozminska-Kubarska A,1981. Cordylobia anthropophaga infestation. Int. J. Dermatol. 20: 495–496.