Antibiotics Susceptibility of Escherichia coli Isolated from Female Students with Urinary Tract Infection
Dirisu C. G.1, *, Egbule O.1, Utuh I. A.2, Uzorka B. A.3
1Department of Biology Education, Federal College of Education (Technical), Omoku, Nigeria
2MD, Sick Bay, Federal College of Education (Technical), Omoku, Nigeria
3Department of Physical and Health Education, Federal College of Education (Technical), Omoku, Nigeria
Abstract
Uropathogenic strains of Escherichia coli were isolated from urine of female students in Madona University Elele, Rivers state, Nigeria and subjected to antibiotics sensitivity test using agar diffusion method. One hundred and twenty-five samples of early morning mid-stream urine were collected and inoculated by streaking directly into sterile eosine methylene blue (EMB) agar and incubated at 37°C for 24 hours. Black colonies with green metallic sheen on EMB, which is typical of E. coli were purified and inoculated on nutrient agar impregnated with multi disc antibiotics using spread plate method. The plates were incubated at 37°C for 24 hours. Observation of clear zone of inhibition indicated sensitivity while absence of any cleared zone indicated resistance. Result indicates that there was significantly more chances of isolating E. coli from urine (p > 0.05). Antibiotics susceptibility result shows that E. coli strains were more likely to be resistant to the antibiotics tested than those that were sensitive. Out of the 50 positive cases, the highest observed resistance was tetracycline (94%) and the least was ciprofloxacin (28%). 80% of isolates were resistant to sulphamethoxazole, 80% to penicillin, 76% to streptomycin and 60% to chloramphenicol. This study reveals that there is an increased rate of drug resistance among patients with urinary tract infection. Since antimicrobial resistance are constantly evolving and present global public health concerns, measures should be taken to prevent E. coli infection by organizing enlightenments programmes regularly to warn the students of the risk of drug abuse, poor personal hygiene and environmental conditions.
Keywords
Antibiotics, E. coli, Urine, Uropathogenic, Resistance, Sensitive
Received: July 16, 2016
Accepted: July 29, 2016
Published online: August 16, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Escherichia coli is a Gram- negative bacterium found in the human and animal lower intestines. E. coli belongs to member of enterobacterioacea family. There are many strains of E. coli and are classified based on the portal of infection, mode of pathogenesis, change in their physiological and life cycle, ability to use unique carbon source, ability to inhabit particular ecological niche and resistance to antimicrobial agent (Davis, 2008). At the molecular level, genes of the following strains have been identified, namely: uropathogenic E. coli (UPEC), enterotoxigenic E. coli, Enterotoxigenic E. coli (ETEC), Enteroinvasive E. coli (EIEC), Enterohemorrahagic E. coli (EHEC) also known as shiga toxin-producing E. coli (STEC), Enteroaggregative E. coli (EAEC) and Adherent-Invasive E. coli (AIEC) (Davis, 2008; Carl et al, 2015; CDC, 2015; MRL, 2016; Wikipedia 2016).
Uropathogenic E. coli (UPEC) causes urinary tract infections (UTI) (Ronald, 2003). The mode of pathogenesis has been described and virulence genes identified (MRL, 2015, Carl et al, 2015). UPEC is known to use a protein, adhesin and bind at specific receptor sites to endothelial cells of the urinary tract and colonizes the bladder. It produces alpha-and beta-hemolysin, which causes lysis of urinary tract cells (Nester et al, 2004; Wikipedia, 2016). UPEC also has the ability to form biofilms, which confer resistance to antibiotics and human immune defenses (Nester et al, 2004; Akinubi et al, 2009). This may account for transferable antibiotic resistance (Alex et al, 2011). An individual’s susceptibility to UTI caused by E. coli can be attributed to lack of UPEC’s receptor, which occurs in approximately 1% of individuals.
Control of bacterial infection by antibiotics treatment either kills or inhibits the growth of microbial pathogen. Non-susceptible microbes have developed resistance to such antimicrobial, which are part of organism’s genetic makeup (Cedric, 1998; Frye and Jackson, 2013). Antibiotic-resistant E. coli may also transfer the genes responsible for antibiotic resistance to other species such as Staphylococcus aureus when they are in close proximity particularly as biofilms. E. coli often carry resistant plasmids and under stress, readily transfer those plasmids to other species.
Most enterobacteriaceae are susceptible to antibiotics such as aminoglycosidess, penicillin and cephalosporin (Egri-Okwajietal, 2005). In this study, uropathogenic strains of E. coli isolated from urine were tested against an array of antibiotics to determine the extent of its sensitivity and resistance.
2. Materials and Methods
2.1. Specimen Collection
A total of 125 samples of early morning mid-stream urine were collected in a sterile container from female student of Madonna University, Elele, Nigeria and immediately transported to the Department of Microbiology Laboratory.
2.2. Culturing and Isolation of Bacteria
A loopful of urine was inoculated by streaking directly into sterile Eosine methylene blue agar (EMB) (Oxoid) and incubated at 37°C for 24 hours. E. coli forms typical black colonies with green metallic sheen on EMB. Isolates were sub-cultured on sterile nutrient agar and incubated at 37°C for 24 hours and the cultured plates were examined for growth (Cheesbourgh, 2006; Todar, 2007).
2.3. Characterization of Bacteria Isolates
Based on colonial morphology, cultural characteristics and biochemical tests, each isolates were identified. The cultural characteristics observed included colony size, shape, colour edge and growth pattern. Microscopy of Gram stained smears of E. coli pure isolates was carried out to determine morphological characteristics while biochemical tests were used for confirmation. Biochemical tests included Indole test and citrate utilization test as described by Todar (2007) as well as catalase and urease test as described by Cheesbrough (2006).
2.4. Antibiotics Susceptibility Test
Antibiotic susceptibility test was done on nutrient agar (NA) using multi-disc antibiotics. Prepared NA was poured in Petri dish and allowed to solidify. Isolated organisms were inoculated into peptone water and allowed for 6 hours. A sterile swap stick was used to transfer organisms in the broth and spread plated. The multi-disc antibiotics impregnated paper was centrally placed and gently pressed into the agar with a pair of sterile forceps. The plate was inverted and incubated at 37°C for 24 hours. Observation of clear diameter zone of inhibition indicated sensitivity while absence of any cleared zone indicated resistance. The interpretation of results was done using the zone sizes. Zone of inhibition greater than 10mm was considered sensitive, 5-10mm moderate, and no zone of inhibition or less than 5 mm resistant (Akinyemi et al, 1997).
3. Results and Conclusion
The frequency (%) of Escherichia coli isolated from the urine samples according to age brackets of the students is shown in figure 1.
Figure 1. Frequency (%) of E. coli positive cases isolated from urine of female students with urinary tract infection.
Fifty (50) positive E. coli cases were recorded. Percentages of the age brackets with positive cases were 33.3, 57.5 and 31.3 for 16-20, 21-25 and 26 age brackets respectively. There was significantly more chances of isolating Escherichia coli from urine.
Table 1 shows the percentage susceptibility of E. coli isolated from students’ urine to various antibiotics. It shows that E. coli strains were more likely to be resistant to the antibiotics tested than those that were sensitive. High resistance to tetracycline was observed, 28% was resistant to ciprofloxacin, 60% to chloramphenicol, 80% to sulphamethoxazole, 76% to streptomycin and 80% to penicillin, while resistance to tetracycline was 94%.
Table 1. Antibiotics Susceptibility Patterns of E. coli Isolated from Clinical Specimen.
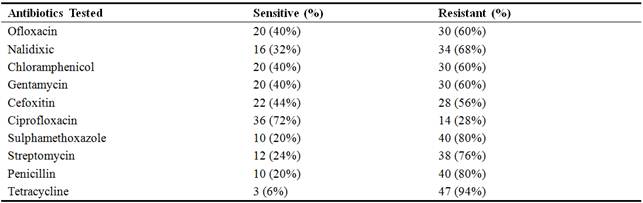
Out of 125 female students that volunteered their urine for examination, 50 had positive isolates of Escherichia coli representing 40%. This is lower than the 59% of E. coli positive cases from urine reported by Umolu et al (2006). Isolates of UPEC have relatively high potentials for developing resistance to antimicrobial agents tested. This was observed by Omigie et al (2006) who also reported resistance of E. coli isolates to tetracycline and sulphomethaxazole.
Antibiotic resistance is a growing problem. Some of this is due to overuse of antibiotics in humans, but some of it is probably due to use of antibiotics as growth promoters in animal feeds (Oteo et al, 2005; Adenipekun et al, 2015). In recent years, the use of quinolones has increased in many countries and emergence of bacterial resistance to quinolones has been observed. Consistent step-wise increase in Escherichia coli resistant to ciprofloxacin was observed from 1995 (0.7%) to 2001 (2.5%) by Bolon et al, (2004). Ciprofloxacin resistance in Portugal was 25% and Italy 24.3% and 6.8%. Albinu et al (2004) observed that E. coli is highly resistant to ampicillin, amoxicillin, tetracycline and trimethoprim - sulfamethoxazole. Also, Umolu et al (2006) reported very high resistance levels (>75%) of E. coli against tetracycline, augmentin and amoxicillin while nitrofurantoin and ofloxacin recorded the least resistance levels of 6% and 19% respectively among the isolates. Stelling et al (2005) equally reported high resistance of E. coli to antimicrobials in South Africa, Israel, Philippines and Hong Kong. Oteo et al (2005) also reported resistance to Ciprofloxacin ranging from. 6.2 to 25.8% in Portugal, Italy, Germany and Netherlands. Isolates in this study were highly resistant to tetracycline.
The study revealed that urinary tract infection is mainly attributed to E. coli, and that girls within the age brackets of 24-25 years are the most affected. This study as well as reviewed literature reveals that there is an increased rate of drug resistance among patients, globally. Since these antibiotics resistant bacteria are constantly evolving and present global public health problem, measures should be taken to minimize E. coli infection by organizing enlightenments programmes regularly to educate students, and particularly females of the risk of drug abuse, poor personal hygiene and environmental conditions. Good toilet, bathroom and portable water should be made available. Proper ventilation should be also allowed within the hostels to avoid spread of infection.
References
- Adenipekun EO., Jackson CR., Oluwadun A, Iwalokun BA., Frye JG., Barrett JB., Hiott LM., and Woodley TA. 2015. Microbial Drug Resistance. 21(3): 358-365. doi:10.1089/mdr.2014.0222.
- Agwung-Fobellah D. 2007. Step by Step Biostatistics for Biological and Health Science.Art of Wisdom Publishers.Abia State of Nigeria: 205–217.
- Aibinu I, Adenipekun E. and Odugbemi T. 2004. Emergence of Quinolone Resistance amongst Escherichia coli strains isolated from clinical infections in some Lagos State Hospital in Nigeria. Nig. J. Health Biomed. Sc. 3 (2): 73-78.
- Akinobu I, Asami T, Thithiwat M, Koji K, Satoshi O. 2009. Increased Antibiotic Resistance of Escherichia coli in Mature Biofilms. Appl. Environ. Microbiol. 75 (12) 4093-4100
- Alex B, Goesseri W, Schee CV, Margreet CV, Cornelissen J, and Hubert E. 2001. Rapid Emergence of ofloxacin- resistant Enterobacteriaeceae containing multiple gentamycin resistant associated integron in a Dutch hospital. Emerg. Infect. Dis. 7(5): 862–871.
- Bolon MK, Wright SB, Gold HS, and Cermeli Y. 2004. The Magnitude of Association between fluoroquinolone-resistant E. coli and K. pneumonia may be lower than previously reported. Antimicrob. Agents Chemother 48: 1934–1940.
- Carl FM, Lixin Z, and Foxman B. 2005.Escherichia coli- mediated urinary tract infections: Are there distinct uropathogenic E. coli (UPEC) pathotypes? FEMS Microbiology Letters 252 (2), 183-190.
- Cheesbrough M. 2000. District Laboratory Practice in Tropical Countries, Part 2. Cambridge University Press, Cambridge, UK: 141.
- Egri-Okwaji MTC, Iroha EO, Kesah CN, Odugemi T. 2005. Bacterial Pathogens causing neonatal sepsis in an out- born neonate unit in Lagos, Nigeria. Nig. Qt. J. Hosp. Med. 6:149-152.
- Frye JG, and Jackson CR. 2013. Genetic mechanisms of antimicrobial resistance identified in Salmonella enterica, Escherichia coli, and Enterococcus spp. isolated from U.S. food animals. Front. Microbiol. 4:135.
- Karlowsky JA, Jones ME, Draghi DC, Thornsbery C, Sahm DF, and Volturo GA. 2004. Prevalence of antimicrobial susceptibilities of bacteria isolated from blood cultures of hospitalized patients in the United States in 2002. Ann., Clin.Microbial.Antimicrob.3:7.
- Kesah CN, Egri-Okwaji MTC, Iroha EO, and Odugbemi T. 2003.Common antimicrobial resistance of nosocomial pathogens. Nig. Postgrad. Med. 6:149-152.
- National Committee for Clinical Laboratory Standards. 2000. Methods for Dilution Antimicrobial susceptibility tests for bacteria that grow aerobically. NCCLS Approved Standard M7-A5 and Informational Supplement M100-S19. Wayne. PA USA.
- Oteo J, Lazaro E, De Abjo FJ, Baquero F, Campos J. 2005. Antimicrobial resistant invasive Escherichia coli. Spain. Emerg. Infect. Dis. 11 (4):546–553.
- Rolhion N, Darfeuille-Michaud A. 2007. Adherent-invasive Escherichia coli in inflammatory bowel disease Inflamm. Bowel Dis. 13 (10): 1277–1283. doi:10.1002/ibd.20176
- Ronald A. 2003. The etiology of urinary tract infection: traditional and emerging pathogens. Dis Mon, 49(2),71-82.
- Sahm DF, Thornsberry C, Mayfield DC, Jones M.E, Karlowsky JA. 2004. Multidrug resistant urinary tract isolates of Escherichia coli: Prevalence and patient demographics in the United States. Antimicrob. Agents Chemother. 41:15-22.
- Stelling JM, Travers K, Turner PJ, O’Brien TF, Levy SB. 2005. Integrating Escherichia coli antimicrobial susceptibility data from multiple surveillance programmes Emerg. Infect. Dis. 11 (6): 873-882.
- Todar K. 2007. Pathogenic E. coli. Online textbook for Bacteriology. Available at http://www.textofbacteriology.net/e.coli.html. Accessed 18/6/2009
- Todorova K, Bratoera M, Danera M. 2006.Characterization of enteroinvasive Escherichia coli serotype 0164 by means of plasmid analysis and virulence assay. J. Basic Microbiol. 30 (6): 451–454.
- Umolu PI, Omigie O, Tatfeng Y, Omorogbe FI., Aisabokhale F, Ugbodagah OP. 2006. Antimicrobial Susceptibility and Plasmid Profiles of Escherichia coli Isolates obtained from different human clinical specimens in Lagos – Nigeria. The J. of Amer Sci 2(4):70-75.



