The Prevalence of Meningitis and Associated Factors (Case study of state specialist hospital) Damaturu
Abubakar El-Ishaq*, Abigail Kadi
Science Laboratory Technology Department, School of Science and Technology, Federal Polytechnic Damaturu, Yobe State, Nigeria
Abstract
Meningitis infection had been reported, especially during the hottest period of the year sequel to the rainy season. The occurrence of meningitis and its related factors were assessed at state specialist hospital Damaturu. A total number of 255 patients were examined for meningitis, and they comprise of 120 Males and 135 Females from January-December, 2009. Cerebrospinal meningitis data was collected from the medical records. The data was analysed statistically and results presented. Age distribution of the examined patients are; Children 57, Adolescents 53 and Adults 145. However, the result obtained showed that only nine (9) patients died as a result of a complication. The immuno-protective capability of the children and adolescent seemed to be stronger than the elderly, where the percentage death is high when to compare to the youngster. Also, female (55.55%) are more prone than male (44.44%). Conclusion, the findings in this research work, has proved that there is still a prevalence of meningitis, and this is as a result of the presence of factors associated with the spread of meningitis. Therefore, some recommendations were made to the entire public and the government in such a way that will bring about a reduction if not completely eradicated.
Keywords
Bacteria, Cerebrospinal Fluid, Damaturu, Environmental Sanitation, Meningitis and Viral
Received: May 27, 2016
Accepted: June 8, 2016
Published online: November 12, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Meningitis is the inflammation of the protective covering of the brain and spinal cord, caused mostly by a viral or bacterial infection that crosses the blood brain barrier. Its is classified as aseptic meningitis when the causative organisms’ is viral, leukaemia and brain abscess, while septic meningitis refers to meningitis caused by bacteria most commonly messier meningitis. The causes of meningitis are - Bacterial resulting from streptococcus, pneumococcus, and Mycobacterium tuberculosis. Viral and Fungal. Many authorities have defined meningitis using various approach:
[1] described meninges as brain and spinal cord, which are completely surrounded by three membranes, meninges that are between the skull and brain and between the vertebra and spinal cord [1]. The report of [7], defined meningitis as an acute infection with the characteristic combination of pyrexia, headache, and meningism, meningitis consists of the stiffness of the neck and irritability of the meninges with positive kerning and bruzidkin’s signs [7]. defined meningitis as infection of pia, arachnoid mater that covers the brain and spinal cord [5]. Also, [13] defined meningitis as inflammation resulting from bacteria virus or chemical toxins such as lead and arsenic contrast media used in myelography and metastasis malignant cell [13]. According to [9] and [15], meningitis is the inflammation of the protective covering of the brain and spinal cord caused mostly by viral or bacterial that crosses the blood brain barrier. Although, harmonious influenza and Streptococcus pneumonia are also causative agents, bacterial meningitis is more severe and associated with high morbidity and mortality with a tendency to occur as epidemic especially in the meningitis belt which lies within 5-15° of the equator having an annual rainfall of 300-1100mm [9, 15]. The outlook is said to occur year round, and the peak incidence is in the winter and early spring [9, 15].
Meningitis can be diagnosed based on the clinical signs and symptoms confirm by isolating the organism from the cerebrospinal fluid. The cerebrospinal fluid is under increased pressure is cloudy or purulent and has grown leukocyte count, a high protein content and a reduced concentration of glucose, blood, nose, and throat swab cultures are done to assist in identifying the organism [8]. Radiography may be taken of the chest, skull and sinuses to detect areas of inflammation and analysis of the cerebrospinal fluid smear and culture are done for the causative organism [5]. Cytological examination of cerebrospinal fluid shows an increase in white blood cell count. The cerebrospinal fluid becomes cloudy, and the pressure increased above normal which is between 120-130mm Hg [8]. Lumbar puncture –this procedure is carried out on the patient by injecting a needle in between the 3rd and 4th lumbar vertebrate to obtained cerebrospinal fluid [5]. Clinical Manifestation are; Headache, nuchal rigidity, fever, photophobia, convulsion, vomiting, irritability, muscle pain, malaise. Classical signs include - Positive brudzinki’s sign, Positive kerning’s sign, Evidence of increased intracranial pressure example hypertension [5].
Management of Bacterial Meningitis can be treated with antibiotics that are introduced into the body intravenously. Viral meningitis is left to let the illness run its natural cause as antibiotics do not work on viruses. Nearly everyone who suffers from viral meningitis recovers completely [8]. Admit in a quiet room and approach the patient gently with a soft, calm voice. The possible spread of infection to others need to be considered. Using isolation procedures may be necessary. It requires prompt and specific antibiotics based on the laboratory result of culture and sensitivity test [8].
A-intravenous injection of crystalline penicillin 1-2mµ four times daily for five days
B- muscle relaxant like diazepam injection 5-10mg noted for 3days
C- analgesic such as paracetamol injection 300mg start, then tabs 1gm ads for 3days.
Observation – the vital sign example blood pressure, pulse, respiration, and temperature are regularly monitored to ascertain patient’s condition either responding to treatment or not [5].
Input and output should be controlled to know if there is any deviation from normal. Psychograph should be given by reassuring the patient and relatives, advice the patient to comply with hospital follow up appointment [5].
Prevention and Control according to [6] stated that there are four basic approaches to the control and prevention of meningitis.
1. The management of sick patients and their contact.
2. Environmental sanitation control design to reduce airborne disease
3. Immunization
4. Surveillance [7].
Risk Factors
There are many risk factors for meningitis as listed below;
i. Complication of illness: - Diseases like otitis media, osteomyelitis, and sinusitis result in meningitis following bacteraemia from infections agents traveling via the blood and choroids plexus or by direct invasion from contagious tissues [12].
ii. Age –babies below 5 years of age and youths in the age group of 15-24 years and older are at risk of being infected with meningitis.
iii. Overcrowding-students living in hostels, dometries, military personnel living on campus are prone to congestion in their environments which leads to improper cross ventilation and thus result in transmission of cross-infection [7].
iv. Pregnant mothers are likely to develop listeriotic (a disease caused by listeria which resembles meningitis and can cause miscarriage). The bacterium also may cause meningitis when there is a complication of listeriosis hence when a child is born of women suffering from listeriosis he becomes at the higher risk of developing meningitis [3].
v. Immune compromised system- people suffering from aids, diabetics and those using immune suppressant drugs are susceptible to develop meningitis. Autoimmune diseases tend to weaken the immune system thereby increasing the risk of meningitis.
vi. At birth –meningitis is contagious diseases that can pass from person to person sometimes infants get it at birth although the mother may not show symptoms of meningitis nonetheless the meningitis germs passes from the mother to the child making the child suffer from the ill health [5].
vii. Poor hygiene Poor hygiene is often responsible for the infection. The enteroviruses that cause meningitis could spread through the feces. Maintaining cleanliness and washing hands regular could prevent meningitis, the unclean environment can cause virus and bacteria to invade the body. Food contaminated with feces of rodents infected with meningitis can cause the disease when passed between people by coughing and sneezing from poor hygiene environment [8].
[1] states that there are three pathways in existing tense by which an infection agent gain access to the central nervous system, and cause meningeal disease [1]. Initially the infectious agent colonies or establishes a localized infection in the host. It's may be in the form of colonization or infection of the skin, nasopharynx respiratory tract, gastrointestinal tract or genitourinary tract. The most meningeal pathogen is transmitted through the respiratory route as exemplified by the nasopharyngeal colonization with Streptococcus pneumonia. From this site, the organism invades the submucosa by circumventing host defences and gains access to the central nervous system by- Invasion of the bloodstream that is bacteraemia, viremia, fungemia, parasitism and subsequent hematogenous seeding of the central nervous system, which is the most common mode of spread for agents [8].
Direct contagious spread i.e. sinusitis congenital malformations trauma, direct inoculation of the intracranial manipulation certain respiratory virus are thoughts to enhance the entry of bacterial agents into the intravascular compartment presumably by damaging most defences, once inside the bloodstream the infective agent developed gradually [5]. Whenever this infection spreads to the brain, the choroids plexus within the villi of the ependyma lining the ventricles start to secrete more cerebrospinal fluid in and flush out the offending organism which is toxicant to cerebrospinal fluid production and its circulation within and around the brain and spinal cord [10, 12].
Infections of the heat-regulating center in the hypothalamus lead to continuous pyrexia resulting into fits in adults or conclusion in children, irritation of the visual center and visual pathway in the brain leads to photophobia. Whenever the neck region of meningitis covering the spinal cord is irritated or inflamed, and the neck is flexed forcibly. The victim always leads to the characteristic’s neck rigidity, the sacral segment of the spinal cord beings about the inability to straighten the knee when the hip is flexed. This is the characteristics positive kerning’s sign of meningitis in which the victim experience severe pain when the knee is forcibly straightened while the hip is flexed, hence he prefers to flex the knee [10, 12].
In another development, the victim may prefer to flex the hip and knee to reduce the pain been felt in response to forward flexion of the neck. Its refers to another characteristic sign of meningitis in the thorax region and lumbar segments of the spinal cord cause the severe back pain. In response to the presence of micro-organisms and their toxin, the reticule-endothelial organs (e.g., bone marrow) produce more while blood cells to combat this infection, this leads to increase leukocyte of the cerebrospinal fluid. In untreated cases, the meningitis patients become confused, drowsy and goes into a coma due to the involvement of all vital canter’s in the brain [12].
Factors that increase the risk of developing bacterial infection are tobaccos smoking, a viral infection of upper respiratory tract because these increase the amount of droplet production. Persons with immune system deficiencies are also at risk for developing bacterial meningitis some areas that are commonly affected within the study area in Damaturu, which was created from the defunct of Borno state in 1976 when general Muritala's regime introduced the local government reform. It was made the capital of Yobe State on 27th August 1991. During the General Ibrahim Babangida’s regime.
Those areas are -Nayinawa ward, Pampomari, Gwange, Pawari and Sabon Pegi ward of the Damaturu metropolis. Therefore, considering the consequences of meningitis infection, socio-economic, political and societal development. The aim of this study is to conduct a survey study on the prevalence of meningitis and associated factors and find out a possible solution to control the occurrence in the human population.
2. Methodology
The principle and method employed are data collection, it also comprises of the sampling techniques and analysis of data. Area of the Study is Damaturu metropolis. Damaturu was situated along trunk "A" Maiduguri / Kano road about 130km west of Maiduguri. It shares a boundary with Gujba to the south, Tarmuwa local government area to the North, Fune local Government to the west and Boron state to the east. Population sample for this research work is the inhabitant of Damaturu metropolis which is populated with over 134,660 inhabitants according to the result of 1999 census. Sampling Techniques for the conduct of the study 2009, cerebrospinal meningitis data was collected from the medical record of state specialist hospital Damaturu.
3. Statistical Analysis
Numerical data were collected and was analysed, presented in the form of Bar chart.
4. Results
The information of meningitis obtained from medical record of state specialist hospital Damaturu was presented in (Figure 1). Its shows that out of some patients admitted with meningitis in 2009 there has been a higher rate in March and May recording 45 cases each this signifies the prevalence of meningitis as the record of each month.
Figure 2 shows the sex distribution of the sample population; male 120 and female 135.
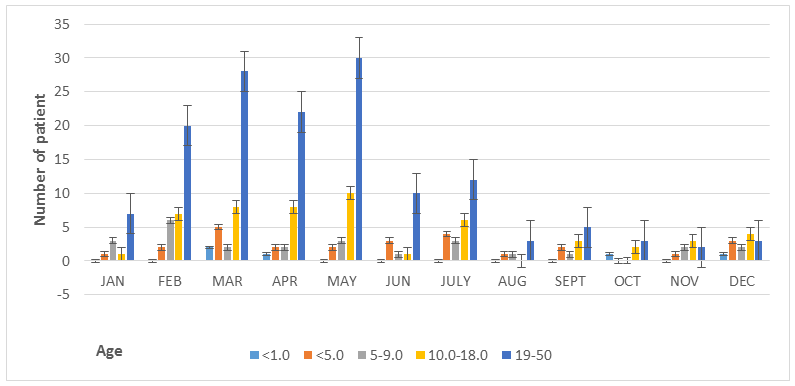
Figure 1. Age range and some admission per month in 2009.
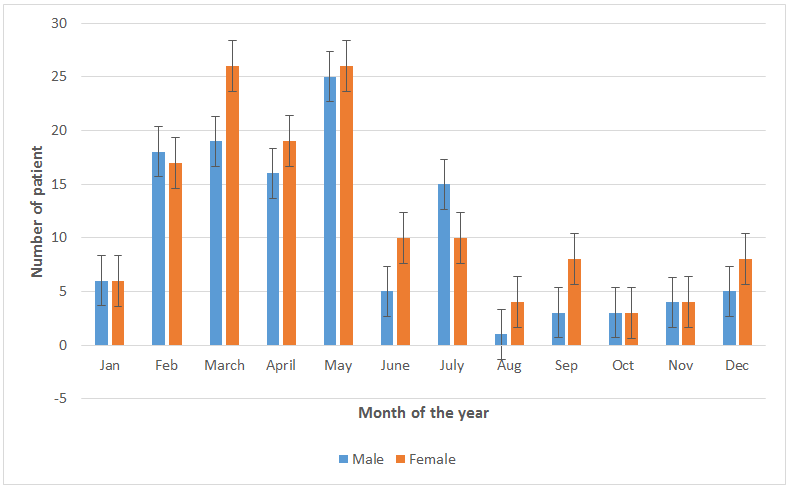
Figure 2. Sex distribution and number of patient’s death per month.
5. Discussion
The figure 1 shows that out of patients admitted with meningitis in 2009 there has been a higher rate in March and May recording 45 cases each this signifies the prevalence of meningitis as the record of months. The above bar chart shows that there was a case of death in three months (3) only, that is March, April, and May, which was nine (9) patient out of the 255 patients, that are admitted throughout the year. Among them are four (4) male adults, three (3) are female adults and two (2) female children as in figure 1 above.
Epidemiology, diagnosis, and antimicrobial treatment of Acute Bacterial Meningitis need a careful assessment to enable clinicians to provide a quick and positive response to compact the menace [7]. It could be deduced that a total number of 255 patients were admitted to the state specialist hospital in 2009, 135 patients are female while only 120 patients are male. Which mean the female are more affected than their male counterpart?
With the limited predictive validity of symptoms and signs and routine laboratory tests, specific tests for JE virus, mumps virus and enteroviruses are required to evaluate the immunization impact and plan for further intervention. CSF bacterial culture cannot be omitted in guiding clinical decisions regarding patient treatment [14]. It can be observed here that the findings, the prevalence is only during the hottest period of the year, this needs to be further research, while the infection rate is not occurring during the rainy season or the harmattan.
6. Conclusion
From the findings in this research work, it has proved that there is still a prevalence of meningitis, and this is as a result of the presence of factors associated with the spread of meningitis. Therefore, some recommendations were made to the entire public and the government in the ways that may bring about a reduction in the number of admitted cases if not totally eradicated.
The paper there recommends as follows;
The government should put more effort to improve environmental hygiene in the villages and rural settlements because unhygienic environment creates a conducive environment for the growth and development of organism caused meningitis. Government and health workers should enlighten people through the mass campaign and other media on the dangers of meningitis. Health educates the entire inhabitants of Damaturu metropolis during harsh weather to protect themselves from becoming infected. They should avoid overcrowding. The government should improve the supply of the vaccine to the community where an outbreak of meningitis is suspected or reported, and the entire community members should be immunized. The government should set up a camp for the infected individuals and restrict visitors strictly.
Well-trained medical practitioners should be provided to care for the infected people in the camp.
References
- Anne Waugh and Allison Grant. (2001). Rose and Wilson. Anatomy and Physiology in Health and Illness 9th edition. Church Hill. Livingstone. Elsevier.
- Ayo, Akinfe. (2009). Do we have a strategy to address meningitis, polio, and Lassa fever? Aakinfe@ao1.com.
- Barbara, F. Weller. (2001). Pocket Medical Dictionary published by Tamsyn declaim are www.amazon.co.uk.
- Epidemic. (2009). In Merriam-Webster. Retrieved from http://www.merriam-wedster.com/dictionary/epidemic
- Famakinwa, T. T. (2002). A Synopsis of Medical, Surgical Nursing Nigeria published by Bayosoye printing services.
- Gilles, H. M. (1990). Epidemic Cycles for Meningococcal diseases for five African Countries over a 30-year period. 1966-1999.
- Matthijs C. Brouwer, 1 Allan R. Tunkel, 2 and Diederik van de Beek. (2010). Epidemiology, Diagnosis, and Antimicrobial Treatment of Acute Bacterial Meningitis. Clinical Microbiology Reviews, Vol. 23, No. 3 p. 467–492 doi: 10.1128/CMR.00070-09.
- Mike, Walsh. (2002). Watson's Clinical Nursing and Related Sciences 6th edition published by Elsevier Science Limited London.
- Oladunjoye, O. (2010). Diagnosing Cerebrospinal Meningitis (CSM) at the Grassroots Levels presented at the sensitisation campaign on the menace of cerebrospinal meningitis held at the Yobe state secretariat Damaturu.
- Olaf Hoffman and Joerg R. Weber (2009). Pathophysiology and treatment of bacterial meningitis. Ther Adv Neurol Disord 2 (6) 401412 DOI: 10.1177/ 1756285609337975
- Oyeyemi, Oyedeji. (2009). Diseases and Death as Meningitis Ravages from North to South Published Sunday magazine.
- Mustapha, R. O. (1999). Path to Success for the student nurses up to final qualifying, printed in Nigeria by Adewumi printing press, publish at 20, major in street Sabo Oke Ilorin.
- Weller, Roy O. Mark I. Fowler, John E. Heckels, and Myron Christodoulides. (2004).Different meningitis-causing bacteria induce distinct inflammatory responses on interaction with cells of the human meninges. In Cellular microbiology. Vol 6. Issue 6.DOI: 10.1111/j.1462-5822.2004. 00382.x
- Xie Y, Tan Y, Chongsuvivatwong V, Wu X, Bi F, Hadler SC, et al. (2015). A Population-Based Acute Meningitis and Encephalitis Syndromes Surveillance in Guangxi, China, May 2007- June 2012. PLoS ONE 10 (12): e0144366. doi: 10.1371/journal. pone.0144366.
- World Health Organization. (2009, May). Meningococcal disease: situation in the African Meningitis Belt. Retrieved from http://www.who.int/csr/don/2009_05_24/en/index.html