Association Between Leptin Hormone and Oxidative Stress Markers in Hypothyroid, Hyperthyroid, and Euthyroid Patients
Maher K. Ibrahim1, *, Abdul-Monaim H. Al-Samarrai2, Khudhair A. Khudhair1
1Department of Biochemistry, College of Medicine, University of Tikrit, Tikrit, Iraq
2Department of Chemistry, College of Education, University of Samarra, Samarra, Iraq
Abstract
The present study aimed to assess if leptin concentration is associated with the serum oxidative stress index (represented by MDA level), antioxidant status (represented by GSH), lipid profile, and/or other parameters of blood biochemistry in eu-, hypo- and hyperthyroid patients. MDA, an index of oxidative stress (OS) was elevated in hyperthyroidism and hypothyroidism patients as compared to euthyroid control, while GSH was a highly significant decrease in all patients with thyroid dysfunction as compared to euthyroid control. The results showed a highly significant increase in the sera levels of TC, TG, VLDL in patients with hypothyroidism and a highly significant decrease in TC and LDL levels in patients with hyperthyroidism patients as compared to euthyroid control. In hypothyroidism patients, there was a significant positive correlation between leptin hormone and BMI, TG and VLDL levels. In hyperthyroidism patients, there was only a significant positive correlation between leptin hormone and BMI, whereas a nearly significant positive correlation was observed between leptin hormone and TG & VLDL levels. Also a nearly significant positive correlation was observed between leptin hormone and MDA levels in hypo-, hyper-, and euthyroid control groups, while a nearly significant negative correlation between leptin and GSH in hypo- and hyperthyroid patients. In conclusion the study demonstrated that oxidative stress was increased in hypothyroidism and hyperthyroidism as indicated by the elevated lipid peroxidation product, MDA, while GSH was reduction.
Keywords
Leptin, Hypothyroidism, Hyperthyroidism, Euthyroid, Oxidative Stress, Lipid Peroxidation, Lipid profile
Received: August 8, 2016
Accepted: August 23, 2016
Published online: October 19, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Leptin is a cytokine hormone made by white adipose tissue that acts by activating specific leptin receptors in hypothalamus to control the energy balance and neuroendocrine processes of the body [1]. It has emerged over the past decade as a key hormone in not only important in the regulation of food intake and energy expenditure, but that it also has a function in the regulation of neuroendocrine and immune function as well as the modulation of glucose and fat metabolism as shown by numerous observational and interventional studies in humans [2]. Leptin circulates in the plasma in amounts directly proportional to body fat stores and responds to changes in energy balance between ingested calories and energy expenditure [3]. Leptin on one hand is known as an anti-obesity hormone and on the other hand obese people develop leptin resistance. Leptin resistance and dyslipidemia together may make the situation worst as both are related to metabolic disorders [4].
People who have thyroid dysfunction have been found to also suffer from weight problems. Thyroid hormone (TH) and leptin are both involved in the regulation of energy metabolism [5]. Weight loss is a typical sign of thyroid hyperfunction, whereas hypothyroidism is generally associated with weight excess [6]. Furthermore, patients with morbid obesity showed significantly lower serum levels of FT4 and FT3, and higher serum concentrations of TSH, when compared with healthy controls [7].
TH play particularly important roles, since both hyperthyroidism and hypothyroidism have been shown to be associated with OS in animals and humans. OS is defined as an unbalance between the production of pro-oxidant substances and antioxidant defenses [8].
Free radicals and disorders of the antioxidant defense system have a pathogenic impact on human tissues and hence are seen as important factors in the development of various diseases [9, 10].
Excessive concentration of free radicals in the cell environment may lead to cell damage and death. This damage may be prevented or alleviated by the presence of antioxidant molecules [11].
Malondialdehyde (MDA) is a natural product of peroxidation of unsaturated fatty acids with three or more double bonds. MDA is the end-product formed during OS. Known OS as an imbalance between pro-oxidants and anti-oxidants, occurs when this balance is disrupted through intense production of ROS and/or by insufficient anti-oxidative defenses, which causes severe defects and damage to biological macromolecules [12]. There is much evidence that show both hyperthyroidism and hypothyroidism are related to OS and cellular damage. The effects of TH on MDA under investigation in several studeis but the results are contradictory to some extent. It was reported that hypermetabolic condition in hyperthyroidism was associated with an increase in free radical formation and lipid peroxidation levels in rat [13] and the patient [14].
Hyperleptinemia has been shown to play a key role in the formation of lipid peroxides and thus to mediate OS, confirmed by the previous observation that leptin increased the OS in tissues where there is a high rate of fatty acid oxidation, including muscle tissues.
Glutathione (GSH) is a tripeptide composed of (glutamate, cysteine and glycine). Often referred to as the main antioxidants in the body, which plays central role in the defense against oxidative damage in humans. GSH is available in the reduced and oxidized forms. Reduced GSH has the ability to give the unstable molecules, such as the ROS, upon oxidation; GSH can be regenerated from the glutathione disulfide by the enzyme glutathione reductase [15]. It exerts its antioxidant function by donating electrons to radicals and changing to its oxidized form, which is subsequently reduced by the enzyme glutathione reductase [16]. In previous studies, there are conflicting results, some of them increase, while several decrease or remain unchanged of antioxidant in hyperthyroidism. It has been reported that GSH plays an important role in the detoxification of H2O2 and prevents the effect of lipid peroxidation [17]. In hypothyroidism, TH levels are very low, suggesting a possible direct involvement of free radical scavengers and lipid peroxidation. Depression of metabolism due to hypothyroidism has been reported to reduce oxidant production and thus protects tissues from damage oxidation [18].
The aim of this study was to investigate the dynamics of OS and antioxidant status marker in both patients with hypothyroidism and hyperthyroidism by measuring the level of MDA and GSH in Iraqi patients and then finding the correlation between all these parameters with leptin hormone.
2. Patients & Methods
2.1. Patients
All samples were collected from laboratory unit in Medical City Hospital-Baghdad. The patients classified into three groups.
1. Groups I: consist of 74 patients with hypothyroidism (19 males and 55 females), mean age 44.3±7.0 yr.
2. Groups II: consisted of 51 patients with hyperthyroidism (16 males and 35 females), mean age 43.5±6.9 yr.
3. Control group: - This group consisted of 55 patients with euthyroid (21 males and 34 females), mean age 36.9±9.9 yr.
To eliminate the factors which might affect free radical antioxidant activity, we excluded all smoking and alcohol drinking subjects, as well as individuals suffering from chronic or acute diseases, such as hypertension, diabetes mellitus, diseases of the liver, kidney, and immunological disorders.
2.2. Specimen Collection
Fasting blood samples were collected and placed into containing tubes. Five milliliters of venous blood were drawn from patients. Slow aspiration of the venous blood sample via the needle of syringe to prevent the hyemolysis with tourniquet applied above the anterior. The samples were dropped into clean disposables tubes, left at room temperature for 30 min. for clotting formation and then centrifuged for 10 min at 5000 run per min to get the serum. Serum samples were stored at -20°C until analysis.
2.3. Methods
Serum leptin, MDA, GSH, TT3, TT4, FT3, FT4 & TSH were determined by Enzyme-linked immunosorbent assay (ELISA) technique. Serum lipid profile was measured immediately.
2.4. Statistical Analysis
All data were expressed as mean ± standard deviations of number of experiments. The statistical significance was evaluated by Student's t-test using SPSS software for Windows, 13 (SPSS, Inc. Chicago, USA). Association between leptin, and biomarkers of study was analyzed by multiple linear regressions. P values <0.05 were considered statistically significant.
3. Result
TT3 and TT4 displayed highly significant depletion in hypothyroidism (0.45±0.32 ng/l and 3.67±1.59 µg/dl) compared with euthyroid control (1.28±0.28 ng/l and 8.18±1.87 µg/dl). The results also show a highly significant increase in the levels of TT3 and TT4 in hyperthyroidism (2.89±1.17 ng/l and 14.83±3.71 µg/dl) compared to euthyroid control. A similar trend of significance was noticed in the serum level of FT3 and FT4 in hypothyroidism and hyperthyroidism patients respectively, as shown in Table 1. On the other hand there was a highly significant increase in TSH value of hypothyroidism (15.12±8.9 mlU/L) and a significant decrease in hyperthyroidism (0.15±0.08 mlU/L) when compared to euthyroid control group (1.96±1.00 mlU/L) (Table 1).
Table 1. Serum TT3, TT4, FT3, FT4 level and TSH level for eu-, hyper-, and hypothyroid patients.
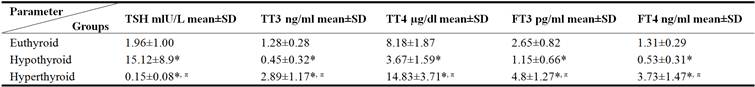
*P < 0.05 when compared to euthyroid. π P < 0.05 when compared hyperthyroid versus hypothyroid group. SD; standard deviation.
The hypothyroid group had higher (P<0.05) BMI, total cholesterol (TC), triglycerides (TG) and VLDL compared with euthyroid control, whereas age, high density lipoprotein cholesterol (HDL) and low density lipoprotein cholesterol (LDL), were not different, while in hyperthyroid group there was lower (P<0.05) BMI, TC and LDL compared with euthyroid control, whereas age, TG, HDL and VLDL, were not different (Table 2 and 3).
In the euthyroid group, leptin correlated positively with BMI only (r=0.29, P=0.03) (Fig. 1-a), while leptin positively correlated with BMI (r=0.35, P=0.01), TG (r=0.28, P=0.01) and VLDL (r=0.28, P=0.01) in hypothyroid (Fig. 2-a, b, c), In hyperthyroid group, leptin correlated positively with BMI (r=0.33, P=0.01) (Fig. 3-a) and a nearly significant positive correlation with TG (r=0.25, P=0.06) and VLDL (r=0.25, P=0.06) (Fig. 3-b, and c) were noticed.
Table 2. Serum TC, TG, HDL, LDL and VLDL level for eu-, hypo-, and hyperthyroid patients.
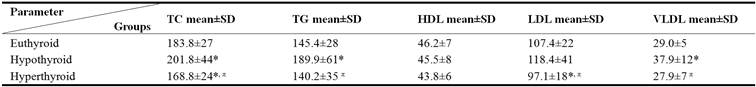
*P < 0.05 when compared to euthyroid controls. πP < 0.05 when compared hyperthyroid versus hypothyroid group. SD; standard deviation.
MDA is higher in both hypothyroid (493.35±169.4 ng/ml; p<0.05) and hyperthyroid (399.52±98.2 ng/ml; P˃0.05) cases in comparison with euthyroid group (336.21±180 ng/ml). The mean serum MDA level in hyperthyroidism patients was significantly (p<0.05) lower than the mean of hypothyroid group (Table 3).
GSH shows a highly significant decrease in both hypothyroidism (3.58±2.68) and hyperthyroidism (4.44±3.35) when compared to euthyroid control group (8.29±4.03), as shown in Table 3.
Table 3. Age, BMI and serum MDA, GSH& Leptin levels for eu-, hypo-, and hyperthyroid patients.
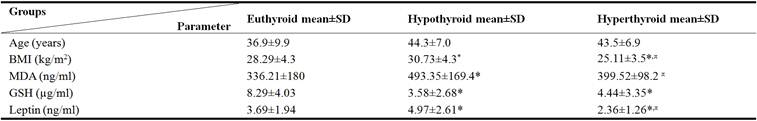
*P < 0.05 when compared to control. π P < 0.05 when compared hyperthyroid versus hypothyroid group.
SD; standard deviation.
A nearly significant positive correlation was noticed between leptin and MDA in euthyroid (r=0.24, P=0.06) (Fig. 1-b), hypothyroid (r=0.23, P=0.06) (Fig. 2-d) and hyperthyroid patients (r=0.26, P= 0.056) (Fig. 3-d). Also a nearly significant negative correlation was noticed between leptin and GSH in hypothyroid (r= -0.24, P=0.05) and hyperthyroid patients (r= -0.27, P=0.054) (Fig. 4), but not in euthyroid control (r= -0.18, P=0.17) with no evident relationship with the thyroid status (Table 4).
Table 4. Correlation of serum leptin and thyroid hormone for eu-, hypo-, and hyperthyroid patients.
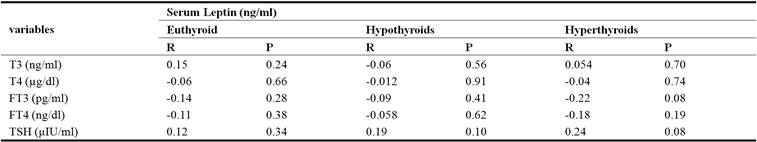
R= correlation coefficients. P= P-values
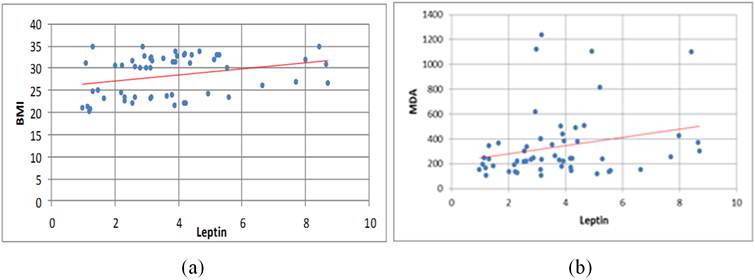
Figure 1. Positive correlation between leptin levels and a) BMI, b) MDA in euthyroid group.
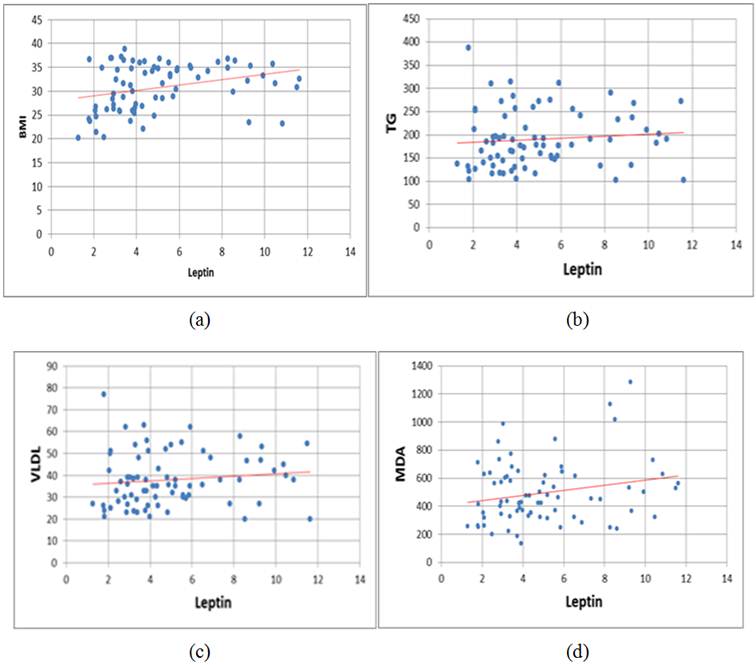
Figure 2. Positive Correlation between leptin levels and a) BMI, b) TG, c) VLDL and, d) MDA, in hypothyroid group.
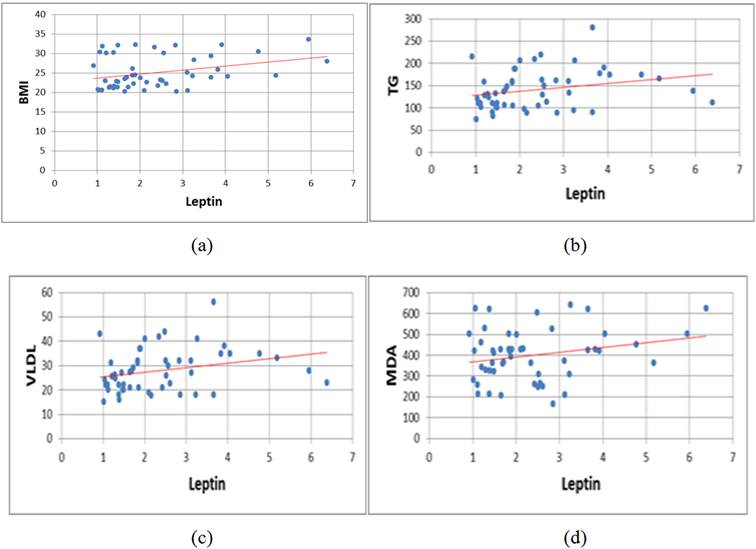
Figure 3. Positive Correlation between leptin levels and a) BMI, b) TG, c) VLDL, and d) MDA in hyperthyroid group.
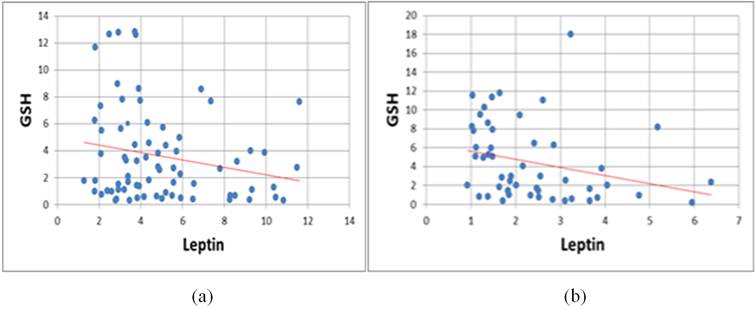
Figure 4. Negative correlation between leptin levels and GSH in (a) hypothyroid group (b) hyperthyroid group.
4. Discussion
People who have thyroid dysfunction have been found to also suffer from weight problems. Results show that there was a significant increase of BMI in hypothyroid group and a significant decrease of BMI in hyperthyroid group in comparison with euthyroid group (Table 3). The results also showed that there was a significant decrease in hyperthyroid group when compared with that of hypothyroid group. The finding results agree with Hoogwerf et al [19], who reported that hyperthyroidism patients lose weight despite an increase of appetite, whereas hypothyroid patients gain weight despite a decreased appetite.
Furthermore, patients with morbid obesity showed significantly lower serum levels of FT4 and FT3, and higher serum concentrations of TSH, when compared with controls [7]. Further, the Knudsen et al [20] study showed that BMI was positively correlated to serum TSH, negatively to serum FT4 and had no correlation to serum FT3. Other investigators [21-23] have also found positive associations between TSH levels and obesity in their studies.
Also the results of the present study show that leptin hormone was significantly high correlated well with BMI. This result was expected; since the major source of leptin in the human body is the adipose tissue and the greater adipose tissue mass the greater is the leptin level. This result supported by other studies [24-26] that demonstrated serum leptin levels showed significant positive correlation with BMI.
The findings of hyperleptinemia in obese humans may be indicating the existence of a defect in the leptin action. Most obese individuals are leptin-resistant [27, 28], an inability of leptin to enter the cerebral spinal fluid to reach the hypothalamus regions that regulate appetite. Leptin resistance may occur for one of several reasons: Leptin may fail to transport through the blood-brain barrier or to reduce signaling distal to the leptin receptor.
In the present study lipid profile of the hypothyroid and hyperthyroid patients showed that maximum number of 40.54% and 11.76% cases had only raised TC, while 58.10% and 29.41% cases had only raised TG, and both hypercholesterolemia and hypertriglyceridemia was seen in 39.18% cases of hypothyroid and 7.84% cases of hyperthyroid patients. Alterations of the lipid profile are well known phenomena in thyroid dysfunction.
The finding results agree with Hueston et al. [29] who reported that hypothyroidism had higher mean TC levels than the euthyroid control group and there were no significant differences in LDL levels. Similar results are also documented by Yu et al. [30], Kung et al. [31] and Pearce et al [32].
Duntas [33] showed that hyperthyroidism exhibits an enhanced excretion of cholesterol and an increased turnover of LDL resulting in a decrease of total and LDL cholesterol.
These changes in the lipid profile are explained by the regulatory effect of TH on the activity of some key enzymes of lipoprotein metabolism. Specifically, the TH stimulates the hepatic de novo cholesterol synthesis by inducing the 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase that catalyzes the conversion of HMG-CoA to mevalonate, the first step in the biosynthesis of cholesterol. This results in an enhanced intracellular cholesterol concentration in hyperthyroidism and a decreased one in hypothyroidism. A study carried out by Duntas [33] showed that overt hypothyroidism is characterized by hypercholesterolaemia and a marked increase in LDL because of a decreased fractional clearance of LDL by a reduced number of LDL receptors in the liver. While in hyperthyroidism exhibits an enhanced excretion of TC and increased turnover of LDL resulting in a decreased total and LDL-cholesterol.
In this study, the serum TG exhibited significant elevations (p<0.05) in the hypothyroid groups and reductions (p>0.05) in the hyperthyroid groups compared with euthyroid control group, as shown in (Table 2). This is also in agreement with the findings of other authors [30, 34] noted that observed plasma TG concentration is greater in hypothyroid than euthyroid and hyperthyroid subjects, due to greater secretion of large, TG-rich VLDL particles from the liver.
Moreover, One mechanism whereby TH might decrease plasma TG could be to increase the activity of lipoprotein lipase (LPL) [35]. Hypothyroid patients showed another pattern of alteration of TG kinetics. The synthesis of plasma TG was normal but the fractional removal of both endogenous and exogenous TG was markedly reduced and this change seems to account for the hypertriglyceridemia associated with thyroid hypofunction. Moreover, a decrease in LPL activity is found in overt hypothyroidism, the clearance of TG-rich lipoproteins [36]. Also the present study showed that serum TG was non-significantly lower in hyperthyroidism compared to euthyroid control patients. These results may be due to that these studies performed in 39 non-obese and 12 obese patients with hyperthyroidism were compared to 31 non-obese and 24 obese in euthyroid control group. Non-obese euthyroid control patients generally had normal levels of TG while the obese patients had hypertriglyceridemia. In most hyperthyroid patients had low TG and the treatment tends to normalize the TG.
The result in (Table 2) showed that there were slightly low, in serum HDL levels in hypo- and hyperthyroid when compared with euthyroid control group but the difference was not statistically significant. These results agree with Hueston et al [29] and Verdugo et al [37]. Another study by Duntas (33) showed that overt hypothyroidism is characterized the HDL levels are normal or even elevated in severe hypothyroidism because of decreased activity of cholesteryl-ester transfer protein (CETP) and hepatic lipase (HL), which are enzymes regulated by TH. The low activity of CETP, and more specifically of HL, results in reduced transport of cholesteryl esters from HDL(2) to VLDL and intermediate low-density lipoprotein (IDL), and reduced transport of HDL(2) to HDL(3). Hyperthyroidism exhibits an enhanced excretion of cholesterol and an increased turnover of LDL resulting in a decrease of total and LDL cholesterol, while HDL is decreased or not affected. Furthermore, in hyperthyroidism some studies suggested that decrease HDL level was due to increased HL activity [34, 35, 38] and also due to increased CETP from HDL to VLDL [33, 39]. So treatment of hypothyroidism is associated with lowering of HDL- cholesterol levels and normalization of CETP and HL activities [29, 40].
There are a significant (p<0.05) increase in serum VLDL level in hypothyroid group in comparison with euthyroid control group, and the mean of VLDL in hyperthyroidism patients was lower than mean of euthyroid control patients (P> 0.05) (Table 2). VLDL cholesterol is produced in the liver and released into the bloodstream to supply body tissues with a type of fat (TG). About half of a VLDL particle is made up of TG.
TH is known to increase the LPL activity, an enzyme responsible for clearance of VLDL and chylomicron from circulation. Thus, in hyperthyroidism clearance of the VLDL and its metabolic product LDL is increased, resulting in decreased VLDL, plasma total and LDL cholesterol [41].
In hypothyroidism the clearance of chylomicron remnant and IDL from circulation was delayed. These LPL activity is decreased in hypothyroidism [35, 36] resulted elevated TG levels associated with increased levels of VLDL [42].
It can be concluded that a relationship between leptin concentrations with TC, LDL and HDL levels among thyroid dysfunction patients was not statistically significant. This was in agreement with the results reported by some investigators [43, 44]. Although, the actual mechanism to the role of leptin in the metabolism of lipids is still not clear in human, yet the studies have shown that 85% of variance in serum leptin levels was explained by a model including BMI, and a weak correlation with gender. An interesting observation of this study, there was only a significant positive correlation of serum leptin with serum TG levels as shown in hypothyroid (r =0.28; p=0.01) (Figure 2-b), a near significant positive correlation in hyperthyroid (r =0.25; p= 0.06) (Figure 3-b) and euthyroid control group (r =0.24; p= 0.07). Theirs may be due to the fact that TG is stored in adipose tissue as the main form of energy among the biochemical markers, which explains its correlation with leptin [45, 46]. There's no simple, direct way to measure VLDL cholesterol, VLDL cholesterol is usually estimated as a percentage of TG value. So the same results may be found. In this study, a serum MDA level was increased significantly in hypothyroid group and non-significantly in hyperthyroid group compared to euthyroid control group (Table 3), this indicates increased OS (OS is defined as an unbalance between the production of pro-oxidant substances and antioxidant defenses). Our results are in agreement with the finding of Cheserek et al [47]. This increase in MDA was related to elevated plasma lipids (mainly LDL). Thus, lipid oxidation in hypothyroidism may not have been directly caused by low thyroid function, but was enhanced by the presence of elevated plasma TC and LDL secondary to hypothyroidism, this was observed by Santi et al [48] The increase in MDA concentration in hypothyroid group may be due to the decrease in cellular receptor numbers of LDL, then reduced its removal from blood stream which in turn lead to increase LDL concentration in blood stream may be hence to formation and accumulation of lipid, that stimulated lipid oxidation and therefore form free radicals, the increased concentration of MDA depend on free radical production [49]. Also our data results is in agreement with the finding of Torun et al [50] and Costantini et al [51] showed that TG, TC and LDL cholesterol levels were significantly high in hypothyroid patients when compared with the controls, and MDA showed a correlation with LDL cholesterol, TC and TG.
It was also suggested that the increase in MDA in hyperthyroid group may be due to the increase in TH secretion which stimulated oxidation of fatty acid (lipolysis) and increase of free radicals in blood stream. This increase leads to an increased MDA secretion in blood stream to bind with free radicals. It was reported that hyper metabolic condition in hyperthyroidism was associated with an increase in free radical formation and lipid peroxidation levels [49, 52, 53].
On the other hand, the present results are disagreeing with the results of [54], it was demonstrated that the products of lipid peroxidation were decreased in hyperthyroidism and hypothyroidism patients. These discrepancies among results seem to reflect a dependence of pro-oxidative processes on various factors, such as tissue, treatment duration and may be due to changes in the antioxidant defense system. Also, it is not possible to exclude the fact that some conflicting results depend on the different accuracies of the methods used for lipid peroxidation determination. For example the method for evaluating thiobarbituric acid reactive substances is inaccurate, and returns results which differ according to the assay conditions used.
There was only a near significant positive correlation of serum leptin with serum MDA levels. This result supported by other study [55]. This association is the largest for the subjects with obesity, indicating that these people are under severe OS [56].
GSH is the first line of defiance against pro-oxidant stress. The GSH-dependent defiance system plays an important role in detoxification of hydroperoxides and prevents the effect of lipid peroxidation [57]. Results of the present study showed that GSH are significantly lower in both hypothyroid and hyperthyroid cases in comparison with that of euthyroid control group (table 3). This result supported by Asayama et al [58], Das and Chainy [59] and ArÝkan et al [60] studies.
There was a high degree of inverse linear correlation between lipid peroxidation (MDA) and GSH [57]. Therefore, the decreased level of GSH may be due to the overproduction of free radicals and increased lipid peroxidation (MDA) in hyperthyroidism [61] and/or hypothyroidism [50].
However, lowered blood GSH levels may also be explained by some other possibilities, including, an increased oxidation rate and due to increased utilization of GSH during the removal of lipid and other peroxides [62, 63].
The present statically results could be showed that there was only a near significant negative correlation of serum leptin with serum GSH levels as shown in (Figure 4). This result supported by other study [64]. In the same manner, the study by Vincent et al [65] showed that OS levels are elevated in human obesity and data was showed strong evidence that incremental increases in BMI are related to increasing imbalance in the antioxidant-pro-oxidant status. Leptin can shift the pro-oxidant and antioxidant balance to favor ROS formation and OS.
5. Conclusion
We found that leptin concentration was associated with serum MDA and GSH. We suggest that hypothyroidism is more prone for lipid peroxidation that need more supplementation of antioxidants because of low antioxidant level to improve the level of lipid peroxidation as compared to hyperthyroidism.
References
- Al-Jumaily EF, Zgaer SH. A Review: Leptin Structure and Mechanism Actions. Bulletin of Environment, Pharmacology and Life Sciences 2014; 3: 185-92.
- Blüher S, Mantzoros CS. Leptin in humans: lessons from translational research. Am J Clin Nutr 2009; 89 (3): 991S–7S.
- Mantzoros CS, Magkos F, Brinkoetter M, Sienkiewicz E, Dardeno TA, Kim SY, et al. Leptin in human physiology and pathophysiology. Am J Physiol Endocrinol Metab 2011; 301 (4): E567-E584.
- Kaur K, Sidhu S, Kaur G. Association between Leptin and Lipid Profile among Women. Annual Research & Review in Biology, 4 (5): 728-735, 2014.
- Yen PM, ‘Physiological and molecular basis of thyroid hormone action’, Physiol Rev 2001; 81 (3), 1097-142.
- Reinehr T, ‘Obesity and thyroid function’, Mol Cell Endocrinol 2010; 316 (2), 165-71.
- Rotondi M, Leporati P, La Manna A, Pirali B, Mondello T, Fonte R, et al. Raised serum TSH levels in patients with morbid obesity: Is it enough to diagnose subclinical hypothyroidism?. Eur J Endocrinol 2009; 160 (3): 403-408.
- Mancini A, Di Segni C, Raimondo S, Olivieri G, Silvestrini A, Meucci, E, Currò D. Thyroid Hormones, Oxidative Stress, and Inflammation. Mediators Inflamm 2016; 2016: 12 pages.
- Mahadik SP, Evans D, Lal H. Oxidative stress and role of antioxidant and omega-3 essential fatty acid supplementation in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 2001; 25: 463–93.
- McCord JM. The evolution of free radicals and oxidative stress. Am J Med 2000; 108 (8): 652–9.
- Patil SB, Kodliwadmath MV, Kodliwadmath MV. Lipid peroxidation and nonenzymatic antioxidants in normal pregnancy. J Obstes Gynecol Indian 2006; 56 (5): 399-401.
- Sabitha K, Venugopal B, Rafi Md, Ramana KV. Rol e of Antioxidant Enzymes in Glucose and Lipid Metabolism in Association with Obesityand Type 2 Diabetes. AJMSM 2014; 2 (1): 21-24.
- Venditti P, Balestrieri M, Di Meo S, De Leo T. Effect of thyroid state on lipid peroxidation, antioxidant defences, and susceptibility to oxidative stress in rat tissues. J Endocrinol 1997; 155: 151–157.
- Iangolenko VV, Okorokov AN. Blood levels of medium molecular weight peptides and lipid peroxidation activity in the differential diagnosis of diffuse toxic guatr. Probl Endokrinol (Mosk) 1991; 37 (1): 10–2.
- Monostori P, Wittmann G, Karg E, Túri S. Determination of glutathione and glutathione disulfide in biological samples: an in-depth review. J Chromatogr B Analyt Technol Biomed Life Sci 2009; 877 (28): 3331-46.
- Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med 2000; 160: 526-34.
- Dariyerli N, Toplan S, Akyolcu MC, Hatemi H, Yigit G. Erythrocyte osmotic fragility and oxidative stress in experimental hypothyroidism. Endocrine 2004; 25: 1-5.
- Dursun B, Dursun E, Capraz, I, Ozben, T, Apaydin A, Suleymanlar G. Are Uremia, diabetes, and atherosclerosis linked with impaired antioxidant mechanisms? J Invest Med 2008; 56: 545-52.
- Hoogwerf BJ and Nuttall FQ. Long-term weight regulation in treated hyperthyroid and hypothyroid subjects," Am J Med. 1984; 76 (6): 963-70.
- Knudsen N, Laurberg P, Rasmussen LB, Bulow I, Perrild H, Ovesen L, et al. Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population. J Clin Endocrinol Metab 2005; 90 (7): 4019-24.
- Bastemir M, Akin F, Alkis E, Kaptanoglu B. Obesity is associated with increased serum TSH level, independent of thyroid function. Swiss Med Wkly 2007; 137 (29-30): 431-4.
- Nannipieri M, Cecchetti F, Anselmino M, Camastra S, Niccolini P, Lamacchia M, et al. Ferrannini, E. Expression of thyrotropin and thyroid hormone receptors in adipose tissue of patients with morbid obesity and/or type 2 diabetes: Effects of weight loss. Int J Obes (Lond) 2009; 33 (9): 001-6.
- Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F. Relationship of thyroid function with body mass index, leptin, insulin sensitivity and adiponectin in euthyroid obese women. Clin Endocrinol (Oxf) 2005; 62 (4): 487-91.
- Yoshida T, Momotani N, Hayashi M, Monkawa T, Ito K, Saruta T. Serum leptin concentrations in patients with thyroid disorders. Clin Endocrinol Oxf 1998; 48 (3): 299-302.
- Kennedy A, Pan Q, Garvey T. The metabolic significance of leptin in humans: gender-based differences in relationship to adiposity, insulin sensitivity, and energy expenditure. J Clin Endocrinol Metab 1997; 82: 1293-300.
- Perry HM, Morley JE, Horowitz M, Kaiser FE, Miller DK, Wittert G. Body composition and age in African-American and Caucasian women: relationship to plasma leptin levels. Metabolism 1997; 46 (12): 1399-405.
- Baig M, Karira KA, Ahmed A, Niaz K, Kamal S. Serum Leptin level in Hyperthyroid Female Patients. JPMA 2003; 53: 176.
- Sharma M, Aronow WS, Patel L, Gandhi K, Desai H. Hyperthyroidism. Med Sci Monit 2011 Apr; 17 (4): RA 85-91.
- Hueston WJ, Pearson WS. Subclinical hypothyroidism and the risk of hypercholesterolemia. Ann Fam Med 2004; 2: 351-5.
- Yu H, Yang Y, Zhang M, Lu H, Zhang J, Wang H, et al. Thyroid status influence adiponectin, acylation stimulating protein (ASP) and complement C3 in hyperthyroid and hypothyroid subjects. Nutr Metab 2006; 3: 1-13.
- Kung AW, Pang RW, Lauder I, Lam KS, Janus ED. Changes in serum lipoprotein (a) and lipids during treatment of hyperthyroidism. Clin Chem 1995; 41: 226–31.
- Pearce EN. Hypothyroidism and dyslipidemia: modern concepts and approaches. Curr Cardiol Rep 2004; 6 (6): 451-6.
- Duntas LH. Thyroid disease and lipids. Thyroid. 2002; 12 (4): 287-93.
- Fabbrini E, Magkos F, Patterson BW, Mittendorfer B, Klein S. Subclinical hypothyroidism and hyperthyroidism have opposite effects on hepatic very-low-density lipoprotein-triglyceride kinetics. J Clin Endocrinol Metab 2012; 93: E414-E418.
- Ito M, Takamatsu J, Matsuo T, Kameoka K, Kubota S, Fukata S, et al. Serum concentrations of remnant-like particles in hypothyroid patients before and after thyroxine replacement. Clin Endocrinol (Oxf) 2003; 58: 621-6.
- Nikkila EA, Kekki M. Plasma triglyceride metabolism in thyroid disease. J Clin Invest 1972; 51: 2103–14.
- Verdugo C, Perrot L, Ponsin G, Valentin C, Berthezene F. Time-course of alterations of high density lipoproteins (HDL) during thyroxine administration to hypothyroid women. Eur J Clin Invest 1987; 17: 313-6.
- Diekman MJ, Anghelescu N, Endert E, Bakker O, wiersinga WM. Changes in plasma low- density lipoprotein (LDL)- and high- density lipo protein cholesterol in hypo- and Hyperthyroid patients are related to changes in free thyroxin, not to polymorphisms in LDL receptor or cholesterol ester transfer protein genes. J clin Endocrinol Metab 2000; 85: 1857-62.
- Kung AW, Pang RW, Lauder I, Lam KS, Janus ED. Changes in serum lipoprotein (a) and lipids during treatment of hyperthyroidism. Clin Chem 1995; 41: 226–31.
- Efstathiadou Z, Bitsis S, Milionis HJ, Kukuvitis A, Bairaktari ET, Elisaf MS, et al. Lipid profile in subclinical hypothyroidism: is L-thyroxine substitution beneficial. Eur J Endocrinol 2001; 145 (6): 705–10.
- Heimberg M, Olubadewo JO, Wilcox HG. Plasma lipoproteins and regulation of hepatic metabolism of fatty acids in altered thyroid states. Endocr Rev 1985; 6: 590-607.
- Teixeira Pde F, Reuters VS, Ferreira MM, Almeida CP, Reis FA, Buescu A, et al. Lipid profile in different degrees of hypothyroidism and effects of levothyroxine replacement in mild thyroid failure. Transl Res 2008; 151 (4): 224–31.
- Haluzik M, Fiedler J, Nedvidkova J, Ceska R: Serum leptin levels in patients with hyperlipidemias. Nutrition 2000; 16 (6): 429-33.
- Al-Shoumer KA, Anyaoku V, Richmond W, Johnston DG. Elevated leptin concentrations in growth hormone-deficient hypopituitary adults. Clin Endocrinol 2000; 47: 153-9.
- Rosenbaum M, Leibel RL: The role of leptin in human physiology. N Engl J Med 1999; 341: 879-84.
- Comizio R, Pietrobelli A, Tan YX, Wang Z, Withers RT, Heymsfield SB, et al. Total body lipid and triglyceride response to energy deficit: relevance to body composition models. Am J Physiol 1998; 274: 860-6.
- Cheserek MJ, Wu G-R, Ntazinda A, Shi YH, Shen LY, Le GW. Association between thyroid hormones, lipids and oxidative stress markers in subclinical hypothyroidism. J Med Biochem 2015; 34 (3) 323–31.
- Santi A, Duarte MMF, deMenezes CC, Loro VL. Association of lipids with oxidative stress biomarkers in subclinical hypothyroidism. Int J Endocrinol 2012; 2012: 7 pages.
- Dumitriu L, Bartoc R, Ursu H. Significance of high levels of serum malonyldialdehyde (MDA) and ceruloplasmin (CP) in hyper- and hypothyroidism. Endocrinologie 1988; 26 (1): 35–38.
- Torun AN, Kulaksizoglu S, Kulaksizoglu M, Pamuk BO, Isbilen E, Tutuncu NB. Serum total antioxidant status and lipid oxidation marker malondialdehyde levels in overt and subclinical hypothyroidism. Clin Endocrinol (Oxf) 2009; 70: 469–74.
- Costantini F, Pierdomenico SD, de Cesare D, de Remigis P, Bucciarelli T, Bittolo-Bon G, et al. Effect of thyroid function on LDL oxidation. Arterioscler Thromb Vasc Biol 1998; 18: 732-7.
- Kumari NS, Sandhya, Gowda KM. Oxidative Stress in Hypo and Hyperthyroidism. Al Ameen J Med Sci 2011; 4 (1): 49 -53.
- Bozhko AP, Gorodetskaia IV, Solodkov AP. Restriction of stress-induced activation of lipid peroxidation by small doses of thyroid hormones. Biull Eksp Biol Med 1990; 109: 539–41.
- Faure M, Lissi EA, Videla LA. Evaluation of the antioxidant properties of thyroid hormones and propylthiouracil in the brain-homogenate autoxidation system and in the free radical-mediated oxidation of erythrocyte membranes. Chem Biol Interact 1991; 77: 173–85.
- Boşnak M, Kelekçi S, Yel S, Koçyiğit Y, Şen V, Ece A. Oxidative Stress in Marasmic Children: Relationships with Leptin. Eur J Gen Med 2010; 7 (1): 1-8.
- Pandey G, Shihabudeen MS, David HP, Thirumurugan E, Thirumurugan K. Association between hyperleptinemia and oxidative stress in obese diabetic subjects. J Diabetes Metab Disord 2015; 14: 24.
- Maddaiah VT. Glutathione correlates with lipid peroxidaiton in liver mitochondria of triiodothyronine-injected hypophysectomised rats. FASEB J 1990; 4: 1513–18.
- Asayama K, Kato K. Oxidative muscular injury and its relevance to hyperthyroidism. Free Radic Biol Med 1990; 8 (3): 293–303.
- Das K and Chainy GB. Thyroid Hormone influences antioxidant defense system in adult rat brain. Neurochem Res 2004; 29 (9): 1755-66.
- ArÝkan E, Sabuncu T, KonukoÛlu D, Üynem H, Akcay T, Hatemi H. The Effects of Hyperthyroidism on Lipid Peroxidation, Erythrocyte Glutathione and Glutathione Peroxidase. Turkish Journal of Endocrinology and Metabolism 2001; 1: 17-19.
- Hotta K, Funahashi T, Arita Y, Takahashi M, Matsuda M, Okamoto Y, et al. Plasma Concentrations of a Novel, Adipose-Specific Protein, Adiponectin, in Type 2 Diabetic Patients. Arterioscler Thromb Vasc Biol 2000; 20: 1595-9.
- Ali WJ, Ali RK, Alfallouji S. The Correlation between Oxidative Stress and Thyroid Hormones in Serum and Tissue Homogenized of Hypothyroidism Patients. Medical Journal of Babylon 2012; 9 (4): 843-9.
- Messarah M, Boumendjel A, Chouabia A, Klibet F, Abdennour C, Boulakoud MS, et al. Influence of thyroid dysfunction on liver lipid peroxidation and antioxidant status in experimental rats. Exp Toxicol Pathol 2010; 62 (3): 301-10.
- Ahmed OM, Gabar MA, Ali TM. Impacts of the coexistence of diabetes and hypothyroidism on body weight gain, leptin and various metabolic aspects in albino rats. J Diabetes Complications 2012; 26 (6): 491–500.
- Vincent HK, Taylor AG. Biomarkers and potential mechanisms of obesity-induced oxidant stress in humans. Int J Obes (Lond) 2006; 30 (3): 400-18.