A Study of Hospital Waste Management Practices at Two Tertiary Care Teaching Hospitals: What Are the Alternate Options in Hospitals of Developing Countries
Sanwal Ali1, *, Ishtiaq Ahmed2
1BE Civil Engineering, Department NUST Institute of Civil Engineering (NICE), National University of Science & Technology, Islamabad, Pakistan
2Department of Surgery, Al-nafees Medical College & Hospital, Islamabad, Pakistan
Abstract
Objective: To assess the biomedical waste management system in two major tertiary care hospitals and to look for the alternative measures which are cost- effective and reliable. Study design: A comparative study Place and duration: The study was conducted at two tertiary care teaching hospitals of Rawalpindi and Islamabad city from 27th April 2014 to 16th May 2014. Methodology: The data was collected through presentations given by hospital administration, direct interviews of hospital staff, questionnaires and direct observation methods. All wards, departments, and general areas of both hospitals were visited and methods of waste segregation, storage at ward or department level, internal transportation, dumping sites, external transportation, and on-site and off-site disposal were studied in detail. Special emphasis was given to seeing the method of waste storage Results: Both hospitals have no waste management committees, written protocols or SOPs for waste management. Both hospitals have no effective system in operation to handle and treat the infected or hazardous waste before disposal or transportation to final site. Neither hospital has its own incinerator or any alternative method of waste treatment at local level. The waste was transported for incineration twice a week but no record or SOP of this activity was maintained by both institutions. Conclusion: Disposal of biomedical waste is not practiced properly even in tertiary care hospitals in urban setup from site of generation to final disposal.
Keywords
Bio Medical Waste Management (BMW), Dumping, Landfill, Hospitals
Received: July 21, 2015
Accepted: May 16, 2016
Published online: November 21, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
The proper disposal of biomedical waste has become a hot topic all over the world The risks associated with bio medical waste management are of a major concern to human health and environment. Improper waste disposal can lead to the spread of infectious diseases, water and soil pollution, health hazards due to toxic substances in the atmosphere and radioactivity which can cause deleterious effects on human and animal health and on the environment [1]. Therefore, hospital waste is not only a potential health hazard to the health care workers but also a major hazard for the public and flora and fauna of that area [1, 2].
Biomedical waste (BMW) is defined as "any solid or liquid along with its container and any intermediate product, which is generated during the investigations, treatment or immunization of human beings or animals" [2]. Biomedical waste is produced by the hospitals, nursing homes, clinics, laboratories, physicians’ office, dental and veterinary institutes [3]. The amount and nature of wastes produced by hospitals depend upon different factors like bed occupancy, work load, type of health care facilities, waste management practices, availability of infrastructure, financial and human resources etc. [1, 3]. The hospital waste should be managed properly to avoid the harm to the general public, specifically healthcare and sanitation workers who are continuously exposed to biomedical waste as an occupational hazard [4]. Appropriate handling, treatment and disposal of wastes are essential elements of health care management, which require well trained technical staff and adequate finances. Biomedical waste management in developed countries is under strict regulations from generation, segregation, collection, dumping, processing, transportation to final disposal stage. Recycling, sewage treatment, composting, landfill and incineration are the most common methods of waste management in practice [5]. In underdeveloped and poor countries, these practices are not observed strictly and biomedical waste disposal is rarely conducted properly, mainly due to lack of financial and human resources. The practices currently used for waste management are potentially hazardous, unsustainable and not reliable to protect public health and environmental integrity which leads to lot of health and environmental concerns for the local society [6, 7]. In our country, there is no plan or policy exists even no effective systems are observed for sustainable management of hospital waste in majority of hospitals.
Biomedical waste management is a continuous issue which needs to be tackled vigorously even when resources and technical assistance are scarce. The medical institutions which are responsible for waste production should consider financially and environmentally compatible procedures for waste disposal. The objective of our study is to assess the biomedical waste management system in two major tertiary care hospitals and to look for the alternative measures that are cost- effective and reliable.
2. Methodology
This observational study was conducted at two tertiary care teaching hospitals of Rawalpindi and Islamabad city from 27th April 2014 to 16th May 2014. Prior permission for the visit from our university (NUST) and administration of both hospitals were requested through official channels. The objective of the study was explained to hospital authorities and verbal consent was obtained. Our group was comprised of students from civil engineering group NUST under supervision of a senior doctor. The data was collected through presentations given by hospital administration, direct interviews of hospital staff, questionnaires and direct observation methods. The hospital administrators were interviewed to get in-depth knowledge regarding hospital waste management procedures, policy and training of the staff.
The team visited all wards, departments, and general areas of both hospitals. Methods of waste segregation, storage at ward or department level, internal transportation, dumping sites, external transportation, and on-site final disposal and off-site disposal were studied in detail. Special emphasis was given to seeing the method of waste storage before transportation for incineration or final damping. Additional information was obtained through literature review and online search. The questionnaire regarding generation and disposal of BMW waste was developed after extensive literature search. All data were collected through a structured format in a similar way from both hospitals to avoid any discrepancy and evaluated at the end of study.
3. Results and Observations
Both hospitals maintain good cleanliness and hygiene inside their premises. The atmosphere in general was healthy and periodic mopping was functional. The operation theatre had high standard of cleanliness and sterilization system in function.
Waste management committee or protocol: There were no waste management committees, written protocols or SOPs for waste management existed at either hospital. Both hospitals have designated supervisors to observe the waste management but no proper SOPs existed as per international standards.
Waste segregation: The segregation of various types of wastes was being practiced at the site of generation. These practices were observed inside the wards or departments but they were not up to satisfactory level as compared to the international standards. The used syringes, drug ampoules and sharps were being disposed of properly in wards. The hospitals try to segregate the waste from the start where it is generated. However, there is no system to check or verify the correct segregation of waste at the later stages. Waste was being segregated, but the color coding for waste bags was not followed as suggested by Hospital Waste Management Rules, 2005 [1]. Hospitals have no system in operation to handle and treat the infected or hazardous waste before disposal or transportation to final site.
Waste transportation: Moreover, the collection and transportation from wards to dumping site were not being carried out as per international standards. The staff was not using proper protection during collection, segregation, and transportation of waste. Separate or designated storage places did not exist inside the hospitals, and the waste was transported and dumped improperly, in an open pit situated in the backyard of hospital premises.
Dumping of waste and final disposal: The dumping site was unmarked, unsupervised, improperly excavated and maintained. All sorts of waste were being dumped at the same place haphazardly without any pretreatment or technical supervision (Fig.-1a & Fig.-1b). Neither hospital has its own incinerator or any alternative method of waste treatment at local level. The waste was transported to another faraway place (about 30 km) for incineration at least twice a week as reported by hospital authorities; however, no record or SOP of this activity was maintained by both institutes.

Fig. 1. a,b: Pictures showing the improper dumping of waste outside hospital premises in a pit.
Staff training and awareness: Regarding training of staff, no system was identified for the proper training or education of staff about biomedical waste hazards and segregation. Further formal interviews of the administrative, medical, paramedical, and sanitary staff revealed a gross lack of awareness among sanitary staff and paramedical staff regarding biomedical waste management and handling in both hospitals.
4. Discussion
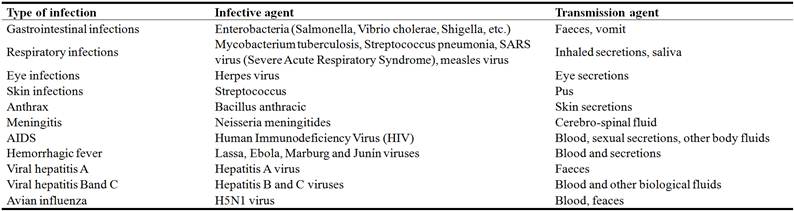
Biomedical waste is usually divided into five categories which pose tremendous risks to human and environment. It include risk of trauma, infection, chemical pollution, fire or explosion, and radioactivity (Table-1). In addition, it also causes environmental contamination and pollution, with subsequent consequences for human health [5, 8].
Accidental exposure to blood or to other body fluids is one example of accidental exposure to hazardous medical waste. Various studies conducted in high-income or developed countries reported that the risk of infection in persons employed in the processing of medical waste is about six times higher than that for persons processing general domestic waste. Among these persons, the risk of contracting an allergic pulmonary disease is 2.6 times, chronic bronchitis 2.5 times, and hepatitis about 1.2 times higher. Respiratory diseases and bronchitis, in particular, are due to exposure to the bio-aerosols present in atmospheric air at the sites where the biomedical waste is dumped, stored and processed [9].
The majority of chemical and pharmaceutical products used in medical institutions entail a health risk due to their toxic, irritant, mutagenic, carcinogenic, corrosive, sensitizing, explosive, or inflammable properties. These substances produce their effects when contacted through various exposure routes, such as ingestion, inhalation of droplets, vapors or gas, and with mucous membranes or skin [9, 10]. These bio-aerosols may also contain bacteria (gram-negative or positive), aerobic actinomyces and sewage fungi [11]. Another toxic substance, mercury (a heavy metal in liquid form at room temperature and pressure) is used in thermometers, manometers, certain types of batteries, electronic components, dental alloys, fluorescent or compact fluorescent light tubes, and blood pressure apparatus. After spillage, mercury readily evaporates and can remain in the atmosphere for up to one year. It also accumulates in sediments and is converted into methylmercury, which is more toxic. Health-care facilities are one of the main sources of mercurial pollution of surface water. The mercury in the atmosphere is also due to the incineration of medical waste [8, 10].
Table 1. Examples of infections that can be caused by hazardous medical waste.
The reduction of waste generation should be encouraged by healthcare institutes. This can be achieved by reducing the amount of waste at the source, choosing products that produce less waste (e.g., products with less wrapping material), choosing suppliers who can take back empty containers, returning the gas cylinders to supplier for refilling, and preventing wastage [5].
The choice of disposal and treatment techniques of waste depends on a number of parameters. These include the quantity and type of wastes produced, waste treatment site near the hospital, cultural acceptance of treatment methods, availability of reliable means of transport, and space around the hospital. In addition, the availability of financial, material and human resources, national legislation on waste management, the climate and groundwater level should also be considered [11]. [12].
There is no universal solution for medical waste treatment. The method should be selected with a view to minimize negative impacts on environment and health. The option selected may be a compromise which depends on local circumstances. If there is no infrastructure available in the vicinity for treatment of waste before disposal, then the hospital is responsible for treating or pre-treating its waste products on-site. Pre-treatment of waste also has the advantage of avoiding hazards and complications involved in the transport of hazardous substances [1, 13].
Hazardous medical waste should be treated or disposed depending on the type and circumstances of waste produced. It can be disinfected by adding chemical disinfectants (chlorine dioxide, sodium hypochlorite, per acetic acid, ozone, alkaline hydrolysis) [10]. The waste may be treated thermally at low temperatures (100° to 180°C), by vapours (autoclave, micro-waves), by hot air (convection, combustion, infrared heat), high temperatures (200° to over 1000°C), or by incineration (combustion, pyrolysis and/or gasification). Selected waste may also be treated by irradiation (UV rays, electron beams) or biologically by adding enzymes [4, 14].
In addition, waste may also be disposed by mechanical processing (shredding), encapsulation (or solidification), and through burial i.e., in sanitary landfills, trenches or pits. These procedures can be used effectively and alternatively in hospitals having scarce technical expertise, lack of finances like rural area hospitals in our setup [15].
Encapsulation: Encapsulationor solidification is a process in which a small number of hazardous waste items are mixed with a mass of inert material. The purpose of this treatment is to protect humans and the environment from any risk of contact with waste. In this method the containers are filled with waste along with an immobilizing material and sealed for some time [16]. For this purpose, either cubic boxes made of high-density polyethylene or metallic drums are used and filled up to three-quarters with hazardous medical waste like sharps, chemical, pharmaceutical material or incinerator ash. These boxes or containers are then filled with aninert medium such as lime, clay, cement mortar, plastic foam, or bituminous sand. After the medium has dried, containers are sealed and disposed of in a waste burial pit or a sanitary landfill [13].
As an example, for 65% of pharmaceutical waste, 15% lime, 15% cement and 5% water is recommended [7]. The main advantage of this process is that it is very effective in reducing the risk of scavenger’s access to the hazardous waste. The other advantages are that it is simple, inexpensive and safe, especially for sharps and pharmaceutical waste. The encapsulation of sharps is generally not considered as a long-term solution. Encapsulation of sharps or unwanted vaccines could, however, be envisaged in rural areas, temporary settings, such as camps or vaccination campaigns. The main drawbacks of this disposal procedure are that it is regarded as a temporary solution, quantities of treated waste are small and the weight and volume of the waste are increased after treatment [13].
Disposal in a sanitary landfill: The disposal of untreated health-care waste in an uncontrolled dumping site is not recommended and must only be used as a last resort. It can be disposed off in a sanitary landfill, subject to certain precautions. Before discarding hazardous medical waste at municipal landfill, the water and habitat engineer must inspect the site [14].
Advantages of disposal by burial at sanitary landfill site are that it is simple and inexpensive in terms of operating costs. It can be carried out efficiently by using an existing municipal waste management system. Scavengers cannot access the health-care waste if the landfill site is well managed. The problems encountered during this procedure are that this untreated waste remains hazardous, so the landfill should be fenced, secured and guarded. There is also a risk of water pollution. Scavengers and animals need to be controlled.
To avoid risk to other people and environment, the landfill should be covered instantly. One of the recommended techniques is to dig a trench down to the level of old municipal refuse (over 3 months old) and to immediately dump the medical waste under a 2-metre layer of fresh municipal refuse. Before designing sanitaryl and fill it should be ensured that the access should be restricted and controlled. The bottom of the landfill must be water proof and the water table must be more than 2 meters below the bottom of the landfill. It is very important that there should be no drinking water sources or wells in the vicinity of this area. Moreover, the chemicals should not be disposed off, waste should be covered on daily basis and vectors access (insects, rodents, etc.) must be controlled. The competent staff should be available at the site and the discarding areas should be planned well before use. The landfill site must be equipped with a final step to prevent rainwater infiltration and the leachates must be collected and treated [17].
Moreover, a high degree of coordination is essential between collectors and landfill operators for efficient operation. Transport to the landfill site can be a lengthy and costly operation. Authorities are of the opinion that it makes health workers less aware of the need to sort the various types of waste on long-term basis [18].
Disposal in a waste burial pit: Alternatively, a purpose-built separate burial pit could be used, preferably on the hospital site. Ideally, this pit should be lined with low-permeability material such as clay to prevent the pollution of shallow groundwater and should be fenced to prevent scavenger access. Health-care wastes should be immediately buried under a separate soil layer at each turn. It is suggested to spread lime on the waste for added health protection (especially in the event of an epidemic) or to eliminate odour after each unloading operation. The pit should be 3 x 2 x 2 m, having annual capacity of 1200 kg, and it should be planned to keep for five years. The pit should be sealed once it has been filled to 50 cm from the top with a layer of soil (5-10 cm) or cement. The area should be marked (Fig.-2). A protective barrier should be erected to limit access for animals, children, or scavengers [17].
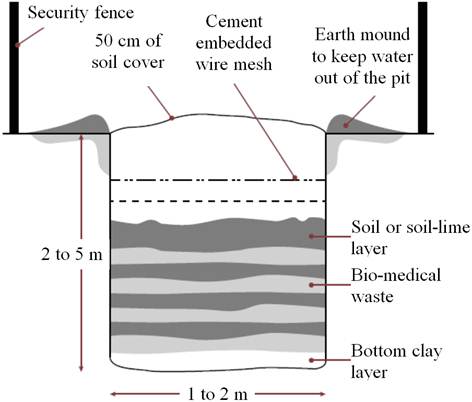
Fig. 2. Diagrammatic sketch of standard purpose built waste burial pit with measurements.
The advantages of this separate pit are that it is simple and relatively inexpensive to build and manage on hospital site. Dangerous substances will not be transported outside the hospital, which minimizes the risk of hazards spread and pollution. The concern is that, since this biomedical waste is not properly treated before dumping, it remains hazardous. There is also a risk of water pollution, badodour, and vectors’ control (insects, rodents, etc.). Space is also needed around the hospital, and proper control must be facilitated. This procedure is unsuitable for areas subject to heavy rains or flooding and where the water table is near the surface (<1.5-2m). These pits are difficult and dangerous to build in sandy areas. By this method the waste volume is not reduced and it also requires 24/7 supervision and surveillance to prevent scavenging [18].
Burial pit for anatomical waste: Anatomical waste should be buried in a separate pit, with an annual capacity of 1,200 kg and dimensions of 3 x 2 x 2 m, with lifespan of 5 years. The best way of operating this pit is that the waste has to be inserted through the opening. The loading chute should be removed when the pit is almost full. Then concrete or a mixture of cement, lime and water should be poured in through the opening (Fig.-3). The area should be marked after that. This method is unsuitable for areas subject to heavy rains or flooding. It is unsuitable if the water table is near the surface (<1.5-2m). There is also a problem of odour. On the other hand, it is simple, inexpensive and offers good security for the disposal of anatomical waste [17].
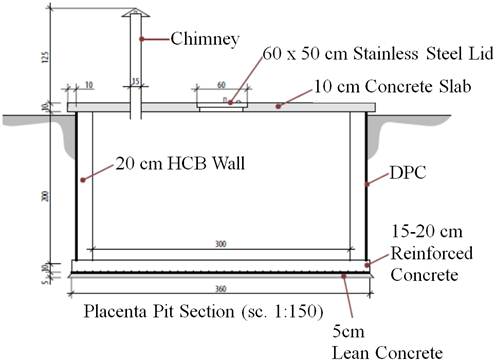
Fig. 3. Diagrammatic sketch of standard anatomical waste burial pit having capacity of 1200kg with measurements.
Burial pit for sharps: This pit should have dimensions of 1m x 1m x 1.4m, annual capacity of 480 kg and lifespan of 3 years. This burial pit is also unsuitable for areas subject to heavy rains or flooding and if water table is near the surface. The waste volume is not reduced but it is simple, inexpensive, and offers good security for the disposal of sharps. The best practice is to insert the sharps through the opening. The loading chute must be removed when the pit is almost full. Concrete or a mixture of cement, lime and water should be poured in through the opening (Fig.-4). This area should also be marked [17].
The above mentioned methods can be used effectively and efficiently in hospitals where the waste management can not be conducted as per international standards due to logistic, technical or financial problems especially in poor or underdeveloped countries or in rural area hospitals. There is a dire need to take realistic and concrete measures aimed at safeguarding the environment for current and future generations. Although, the finding softhe present study are imperative for the management of Bio Medical Waste in Pakistan and other developing countries but the wide spread application of our findings may be limited because of the small sample size of the study. It will be useful to consider the waste management practices at lower levels of health care practice, such as Primary Health Care Centers or Town Hospitals.
Fig. 4. Diagrammatic sketch of standard sharp waste burial pit having capacity of 480 kg with measurements.
5. Conclusion
Disposal of biomedical waste is not practiced properly even in tertiary care hospitals in urban setup from site of generation to final disposal.
Recommendations
Hospitals that are unable to manage their wastes properly due to lack of funds can consider cheaper waste management techniques. By adopting cheaper hospital waste management procedures such as encapsulation, burial in sanitary landfill and waste burial pit etc., hospitals can equip themselves with effective waste management system. Better management of hospital waste will ensure healthier working environment for hospital staff, patients and will also help in protecting the environment.
References
- Hirani D P, Villaitramani K R, Kumbhar S J. Biomedical Waste: An Introduction to its Management. Int J of Innovative Res in Advanced Eng (IJIRAE). 2014; 1 (8): 82-7.
- Singh H, Rehman R. Management of bio-medical waste: a review. Int J of Dental and Med Res. 2014; 1 (1): 12-19.
- Mathur P, Patan S, Shobhawat S. Need of Biomedical Waste Management System in Hospitals - An Emerging issue - A Review. Curr World Environ 2012; 7 (1): 117-24.
- Kumar S, Manjunatha M, Vijetha B, Pradeep PR. Biomedical Waste Management: a review. J Oral Health Comm Dent. 2012; 6 (3): 141 -44.
- Hossain M S, Santhanam A, Norulani NAN, Omar AKM. Clinical solid waste management practices and its impact on human health and environment – A review. Waste Manag. 2011; 31 (4): 754-66.
- Hegde V, Kulkarni RD, Ajantha GS. Biomedical Waste Management. Journal of Oral and Maxillofacial Pathology 2007; 11 (1): 5-9.
- Abah SO, Ohimain EI. Healthcare waste management in Nigeria: Acase study. J of Public Health and Epidemiol. 2011; 3 (3): 99-110.
- Udofia EA, Nriagu J. Health-care Waste in Africa: A silent crisis? Glob. Health Perspect. 2013; 1 (1): 3-10.
- Biswal S. Liquid biomedical waste management: An emerging concern for physicians. Muller J Med Sci Res 2013; 4: 99-106.
- Squire JNT. Biomedical Pollutants in the Urban Environment and Implications for Public Health: A Case Study. ISRN Public Health. 2013. Website: [http://dx.doi.org/10.1155/2013/497490].
- Ogbonna DN, Chindah A, Ubani N. Waste management options for health care wastes in Nigeria: A case study of Port Harcourt hospitals. Journal of Public Health and Epidemiology 2012; 4 (6): 156-69.
- WHO (2014). Safe management of wastes from healthcare activities (2nd edn). Geneva, Switzerland: WHO Press, pp. 102, 136-138, 181-90.
- Forastiere F, Badaloni C, de Hoogh K, von Kraus MK, Martuzzi M, Mitis F et al. Health impact assessment of waste management facilities in three European countries. Environmental Health. 2011, 10: 53.
- Reinhart DR, McCreanor PT. Medical Waste Management: Where Does the Solid Waste Go? Lab Medicine. 2000; 31: 141-45.
- Hassan MM, Ahmed SA, Rahman KA, Biswas TK. Pattern of medical waste management: existing scenario in Dhaka City, Bangladesh BMC Public Health 2008, 8: 36.
- Hegde V, Kulkarni R D, Ajantha G S. Biomedical waste management. J Oral Maxillofac Pathol 2007; 11: 5-9.
- Ajimotokan HA, Aremu SA. Case Study Evaluation of Health-Care Waste Challenges in Hospitals within Ilorin Metropolis. Civil Engineering Impact on National Development: 1st Annual Civil Engineering Conference, University of Ilorin, Nigeria, 26-28 August. 2009; 130-34.
- Abor PA. Managing healthcare waste in Ghana: a comparative study of public and private hospitals. Int. J. Health Care Qual. Assur. 2013; 26 (4): 375-86.