Diagnosis, Treatment and Prophylaxis of Aids
Ana Carolina Kogawa*, Hérida Regina Nunes Salgado
Department of Drugs and Pharmaceutics, School of Pharmaceutical Sciences, Universidade Estadual Paulista “Júlio de Mesquita Filho” - UNESP, Araraquara, Brazil
Abstract
AIDS is the final stage of the disease caused by HIV. It attacks the defense cells of the body, leaving the body vulnerable to all kinds of diseases. Therapeutic agents are divided according to their mechanism of action, nucleoside or nucleotide transcriptase inhibitor, non-nucleoside reverse transcriptase inhibitors, protease inhibitors, fusion inhibitor, entry inhibitor and integrase inhibitor. AIDS is diagnosed through different phases. Each with different characteristics. Selection of mutations in HIV genome conferring cross resistance to different compounds of each class is unfortunately a not infrequent occurrence. Drug resistance due to mutations and sub-inhibitory antiretroviral drug concentrations provide treatment failure. Currently, treatment of HIV infection relies on the so-called “Highly Active Antiretroviral Therapy” which proposes the combination of several drugs in a daily regimen. The reduction in the incidence of HIV infection has been a priority for the control of AIDS in the world with an initial prevention strategy based on behavior change. Around the world there are campaigning to mobilize people about prophylaxis of the disease. and 1st of December is celebrated the “International day of fight against AIDS”. All this global involvement is remarkable, since the number of deaths and new infections has been falling. AIDS still has no cure, but HIV patients have a treatment to prolong survival and improve quality of life by reducing the viral load and immune system reconstitution.
Keywords
AIDS, Antiretroviral Drugs, Diagnosis, HIV, Prophylaxis, Treatment
Received: March 30, 2015
Accepted: April 13, 2015
Published online: April 20, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
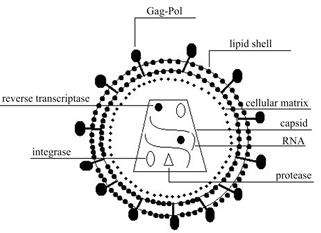
Figure 1. Cell infected with HIV, focusing on its components.
AIDS means Acquired Immunodeficiency Syndrome. It is the final stage of the disease caused by HIV (Human Immunodeficiency Virus), virus belonging to the class of retroviruses, causes severe damage to the immune system. It attacks the defense cells of the body, leaving the body vulnerable to all kinds of diseases. The cells most affected by HIV are the CD4 + T lymphocytes.
It is believed that AIDS was born much longer than is known (50 or more), when the virus responsible jumped the species barrier and began your career in a primate species whose population was booming, man.
AIDS must have originally circulated in African rural areas and in small numbers of patients. However, social changes that hit the Africa in recent years, such as decolonization, the slight improvement of medical care, which is initially reflected in the sharp decline in infant mortality, with fertility maintained, caused a population explosion.
The typical African system in which men come to the mines or where there is work and women stay in the villages helped a lot. The presence of men in the mines, for example, attracted thousands of prostitutes which cultivated and passed HIV in male environment, and probably one or other was in charge of doing the same thing in their spouses.
The spread occurred initially in Africa, but soon spread worldwide. More than 60 million people have been infected with the HIV infection. HIV/AIDS is now the leading cause of death in sub-Saharan Africa, and is the fourth biggest killer worldwide [1]. Since the introduction of zidovudine in the 1980s as the first compound demonstrated to be effective against the HIV, an intense research has led to the development of a wide arsenal of antiretroviral agents. Efforts for expanding the variety therapeutic agents continue and new drugs are constantly approved to improve the efficiency of the treatments [2]. Therapeutic agents are divided according to their mechanism of action. Nucleoside or nucleotide transcriptase inhibitor (NRTIs-NtRTI), non-nucleoside reverse transcriptase inhibitors (NNRTIs) and protease inhibitors (PIs). Moreover, new therapeutic targets and new therapeutic families have been investigated to treatment of the HIV infection, a fusion inhibitor, an entry inhibitor and an integrase inhibitor [1-4]. Table 1 shows the antiretroviral drugs according to their mechanism of action or family.
Table 1. Antiretroviral drugs and their divisions as to the mechanism of action or family
| Family | Antiretroviral drugs |
| Nucleoside or nucleotide transcriptase inhibitor | lamivudine, abacavir, zidovudine, stavudine, didanosine, emtricitabine, tenofovir |
| Non-nucleoside reverse transcriptase inhibitors | efavirenz, etravirine, nevirapine, rilpivirine |
| Protease inhibitors | atazanavir, darunavir, fosamprenavir, indinavir, lopinavir/ritonavir, ritonavir, saquinavir, tipranavir |
| Fusion inhibitor | enfuvirtide |
| Entry inhibitor | maraviroc |
| Integrase inhibitor | raltegravir |
2. Diagnosis
The immune system is attacked when infection by the virus that causes AIDS occurs. Normally, AIDS is manifested through different phases, as shown in Table 2.
Table 2. The different phases of AIDS and its manifestations
| Phase | Manifestation |
| 1 | Acute phase, which can be confused with other diseases |
| 2 | Asymptomatic phase, which lasts for years |
| 3 | Phase when the main symptoms of AIDS are manifested |
| 4 | Phase when opportunistic diseases appear |
In the first phase, called the acute infection, occurs incubation of HIV. This period varies from 3 to 6 weeks and is the time of exposure to virus until the appearance of the first signs of the disease. The body takes 30 to 60 days after infection to produce anti-HIV antibodies. The first symptoms are much like flu symptoms, such as fever and malaise. Therefore, the majority of cases the disease goes undetected. The next phase is marked by the interaction between immune cells and the constant and rapid mutations of the virus. But this does not weaken the body enough to allow new diseases, because viruses mature and die in a balanced way. This period can last many years, it is called asymptomatic.
A person being HIV positive is not the same as having AIDS. Many HIV-positive individuals living years without manifesting symptoms and without developing the disease, although they can transmit the virus to others through unprotected sex, sharing of contaminated syringes or from mother to child during pregnancy and breastfeeding.
Defense cells become less efficient until they are destroyed with frequent attacks. The body becomes increasingly weak and vulnerable to common infections. The initial symptomatic phase is characterized by high reduction of CD4 + T lymphocytes, that come to stay below 200 units per mmof blood (in healthy adults, this value ranges between 800-1200 units). The most common symptoms are fever, diarrhea, night sweats and weight loss.
The low immunity allows the emergence of opportunistic diseases, that take advantage of the weakness of the body to install themselves. Thus, the most advanced stage of the disease, AIDS, is achieved. People who reach this stage can suffer from viral hepatitis, tuberculosis, pneumonia, toxoplasmosis and some types of cancer. People in this stage do not know they have the disease or do not follow the treatment prescribed by doctors.
AIDS is a disease that can be identified through the HIV test that can be done between 40-60 days of risky behavior such as, such as have sex without a condom or share needles, for example.
Thirty days after the first test, it is recommended to repeat the test, even if the first result has given negative. This serves to demonstrate the presence of anti-HVI 1 and anti-HIV 2 antibodies in the body, indicating or not the disease. Between 3 and 6 months, the test should be repeated because of the possibility that the individual is in the immunological window, which is when the disease can not yet be identified, although the individual already be infected.
3. Treatment
Selection of mutations in HIV genome conferring crossresistance to different compounds of each class is unfortunately a not infrequent occurrence. Therefore, there is the need of a new therapeutic tools able to overcome the extensive class resistances observed in multi-treated patients [5].
Drug resistance due to mutations of the viral genome accounts for a large proportion of treatment failures. Sub-inhibitory antiretroviral drug concentrations promote the selection of resistance mutations in the HIV genome during viral replication. Poor penetration of drugs into several profound compartments of the body (sanctuary sites), inadequate treatment adherence, and variability in drug pharmacokinetics may contribute to the occurrence of sub-therapeutic drug level in vivo [6].
Treatment of HIV infection currently relies on the so-called “Highly Active Antiretroviral Therapy” (HAART) which proposes the combination of several drugs in a daily regimen. The complexity of HAART brings clinical issues to be solved such as minimizing the occurrence of viral resistances and preventing adverse effects [2].
HAART is based on the coadministration of drugs from two o three different classes, one non-nucleoside reverse transcriptase inhibitor (NNRTI) or ritonavir in combination with a protease inhibitor (PI) along with two nucleoside reverse transcriptase inhibitors (NRTI), aiming to inhibit multiple viral targets [4,6].
Treatment of HIV infection relies on an association of antiretrovirals drugs, including at least one protease inhibitor (PI) or a non-nucleoside transcriptase inhibitor (NNRTI) and/or one or more nucleoside or nucleotide transcriptase inhibitor (NRTIs-NtRTI) and/or a fusion inhibitor (FI) [5].
Psychological and nutrition support and regular physical activity are also important during treatment. It is important that individuals follow the treatment properly, to stop disease progression and help control the AIDS epidemic in the world. Accurate measurement of PIs and NNRTIs plasmatic levels is crucial for pharmacokinetic/pharmacodynamic analyses, drug–drug interaction studies, and therapeutic drug monitoring (TDM). The latter is currently considered a useful tool for the optimisation of antiretroviral therapy in most international guidelines [2,5,9].
However, sampling blood for TDM on specimen collection cards has several advantages over venous blood sampling. First of all, sampling of blood on collection cards allows sampling outside the hospital, for example, in resource-limited settings or for self-sampling by patients at home. Moreover, a drop of blood on a collection card can be obtained with a simple fingerprick or heelprick. This allows easy sample collection in populations where intensive sampling by means of venipuncture may be unethical or difficult, for example, in children, neonates and intravenous drug users who are suffering from phlebitis or abscesses at injection sites. Lastly, dried blood spots can be easily stored or transported without the requirements of special storage. This allows easy and cheap shipment of samples throughout the world [10].
Since its appearance, ritonavir-boosted darunavir has shown its efficacy in different clinical settings. Thus, darunavir/ritonavir became the first PI to be approved by the regulatory agencies at two different daily dosages depending on the clinical setting [11].
Darunavir is an inhibitor of the HIV-1 protease of the latest generation characterized by a good activity against multi-drug resistant viral isolates and is used in association with low-dose ritonavir, in experienced patients with limited treatment options [4, 7, 1, 2]. It selectively inhibits the cleavage of HIV encoded Gag-Pol polyproteins in infected cells, thereby preventing the formation of mature virus particles [8,13,14]. Darunavir is a key component of many salvage therapies in multiexperienced patients [5].
Raltegravir is the first member of the long anticipated class of HIV integrase inhibitors that has reached the final stage of clinical development. Raltegravir has antiviral activity in both naive and antiretroviral-experienced patients with mostly favourable safety profile so far [4,7].
New therapeutic approaches directed to host, not viral, targets are also emerging. They are the entry inhibitor. Maraviroc, an exemplar, is a chemokine CCR5 co-receptor antagonist that is used at present, in experienced, R5-tropic HIV-infected patients for whom previous antiretroviral regimens have failed [4,7].
Nevirapine is a non-nucleoside reverse transcriptase inhibitor (NNRTI) widely used as a part of HAART for treatment of HIV/AIDS and prevention of mother-to-child transmission of HIV.
Abacavir is a novel purine carbocyclic nucleoside analogue that exhibits selective activity against HIV-1 and HIV-2 [3].
Enfuvirtide is an inhibitor of the fusion of HIV-1 with CD4 + cells, the first of a new class of drugs called fusion inhibitors. It inhibits the conformational change of gp41 required for fusion of virions to host cells.
With the advent of new antiretroviral drugs, the objective when treating any HIV-infected patient has become to achieve undetectable viral load, regardless of the previous treatment experience. For example, the protease inhibitors were great therapeutic advance in the mid 1990s for the treatment of HIV infection, which resulted in life expectancy for the patients who had failed prior therapies, because the therapeutic intervention in HIV have been directed mainly to two viral enzymes, reverse transcriptase and protease [7]. However only medicines is not enough, it is also necessary that pharmacotherapy be easily performed without sacrificing users. So, in order to improve adherence and quality of life it is important to build a treatment with few or no side effects, with a low number of pills and administered once daily if possible [11].
These types of drugs require frequent administration in relatively high doses being the major cause of non-adherence to treatment and an obstacle to the fulfillment of pharmacotherapy [15]. Moreover, there are important issues of drug adverse reactions and drug interaction associated with antiretroviral therapy. Chronic treatment even the moderate toxicity can lead to serious complications. Treatment failure not only affects the quality of life of patients, but also contributes significantly to the economic burden of the health system [16].
The main advantages of darunavir/ritonavir once daily are a lower pill burden, better tolerability, lower metabolic impact (half ritonavir dose), improvement in adherence, and lower pharmaceutical cost due to lower darunavir and ritonavir doses [11].
Another benefit of once-daily darunavir/ritonavir administration is the cost, an issue that has become very important as HIV infection requires life-long therapy. The 900/100 mg of darunavir/ritonavir once daily (Є523 per month per patient) and 800/100 mg once daily (Є 468 per month per patient) doses represent a saving of Є 190 and Є 245 per month per patient, respectively, compared with 600/100 mg of darunavir/ritonavir twice daily (Є 713 per month per patient), although the cost may vary between different countries and no formal cost analysis was done. The saving calculation in our study might have been overestimated, but other current switch alternatives have the same price (etravirine costing Є 468 per month per patient) or are much more expensive (raltegravir and maraviroc cost Є 842 and Є 816 per month per patient, respectively) than once-daily darunavir/ritonavir, so the latter can be an excellent option as a switch strategy [11].
Only 12 antiretroviral drugs have been approved for use in children (as opposed to the 25 approved for adults). In this context, note the need for the development of antiretroviral drug encapsulation and delivery strategies; work on the technological aspects in order to reduce the dosing frequency and improve compliance of existing pharmacotherapy [15].
Children under seven are usually unable to swallow the solid medications. To make adult medicines suitable for children, tablets or capsules are often processed to adjust dosages and facilitate swallowing. However, liquid formulations, essential for pediatric pharmacotherapy, are cause for growing concern in safety, efficacy and quality. Because organoleptic drawbacks that lead to avoidance and reduced adherence to antiretroviral therapeutic regimes and a decrease in the bioavailability of the drug has been found in many cases [15,17].
The last World Health Assembly approved the resolution “Best medicines for children” and has recently launched the global campaign ‘Make medicines child size’ [15]. Thus, the increased solubility of darunavir when complexed with β-cyclodextrin contributes to a better treatment regimen for adults and children that are able to swallow small tablets or capsules, because the darunavir: β-cyclodextrin complex increased the solubility of the free drug in up to 28 times [17].
4. Prophylaxis
The reduction in incidence of HIV infection has been a priority for the control of AIDS in the world as an initial prevention strategy based on behavior change, such as fidelity to a single partner, condom use, access to sterile injection equipment or to use only disposable material, always disinfect before using every cutting and piercing equipment and in a blood transfusion make sure that the blood passed laboratory tests.
Antiretroviral drugs are used in emergency basis for decades. They avoid infection when there is an accidental exposure or to prevent transmission from mother to baby during pregnancy, childbirth and breastfeeding or to avoid exposure to the virus by health professionals.
A development of this method is for pre-exposure prophylaxis. People in position of vulnerability or exposure, such as men who have sex with men, transvestites, transsexuals, drug users and people living on the street would take a combination of antiretroviral drugs previously.
Around the world there are campaigning for consciousness, information and support to people infected with HIV and 1st of December is celebrated the “International day of fight against AIDS”. The date serves to reinforce solidarity, tolerance, compassion and understanding with people infected with HIV/AIDS.
The red ribbon, which represents blood and passion, is seen as a symbol of solidarity and involvement in the fight against AIDS. The lace design was created in 1991 by a group of art professionals in New York, which wanted to pay homage to friends who had died or were dying of AIDS.
All this consciousness and mobilization is valid because in the last decade, the number of deaths and new infections, even in the poorest countries of Africa, fell. Already there is talk of ending the disease.
However, currently, AIDS has no cure. But HIV patients have a treatment to prolong survival and improve quality of life by reducing the viral load and immune system reconstitution. The antiretroviral drugs used to treat slow the appearance of AIDS and enable greater quality of life to the carrier of the virus.
Acknowledgments
The authors acknowledge to CNPq (Brasília, Brazil), FAPESP, CAPES and PADC/FCF/FUNDUNESP (São Paulo, Brazil). This paper is dedicated to School of Pharmaceutical Sciences on the occasion of its 90th anniversary.
References
- Reddy, B.V.R.; Jyothi, G.; Reddy, B.S.; Raman, N.V.V.S.S.; Reddy, K.S.C.; Rambabu, C. Stability-indicating HPLC method for the determination of darunavir ethanolate.J Chromatogr Sci.,2013, 51, 471-476.
- D’Avolio, A.; Simiele, M.; Siccardi, M.; Baietto, L.; Sciandra, M.; Bonora, S.; Di Perri, G. HPLC–MS method for the quantification of nine anti-HIV drugs from dry plasma spot on glass filter and their long term stability in different conditionsJ. Pharm. Biomed. Anal., 2010, 52, 774-780.
- Rao, R.N.; Shinde, D.D. Two-dimensional LC–MS/MS determination of antiretroviral drugs in rat serum and urine.J. Pharm. Biomed. Anal.,2009, 50, 994-999.
- Else, L.; Watson, V.; Tjia, J.; Hughes, A.; Siccardi, M.; Khoo, S.; Back, D. Validation of a rapid and sensitive high-performance liquid chromatography–tandem mass spectrometry (HPLC–MS/MS) assay for the simultaneous determination of existing and new antiretroviral compounds.J. Chromatogr. B., 2010, 878, 1455-1465.
- D’Avolio, A.; Siccardi, M.; Sciandra, M.; Lorena, B.; Bonora, S.; Trentini, L.; Di Perri, G. HPLC–MS method for the simultaneous quantification of the new HIV protease inhibitor darunavir, and 11 other antiretroviral agents in plasma of HIV-infected patients.J. Chromatogr. B.,2007, 859, 234-240.
- D’Avolio, A.; Simiele, M.; Siccardi, M.; Baietto, L.; Sciandra, M.; Oddone, V.; Stefani, F.R.; Agati, S.; Cusato, J.; Bonora, S.; Di Perri, G.A HPLC–MS method for the simultaneous quantification of fourteen antiretroviral agents in peripheral blood mononuclear cell of HIV infected patients optimized using medium corpuscular volume evaluation.J. Pharm. Biomed. Anal.,2011, 54, 779-788.
- Fayet, A.; Béguin, A.; Zanolari, B.; Cruchon, S.; Guignard, N.; Telenti, A.; Cavassini, M.; Gunthard, H.F.; Buclin, T.; Biollaz, J.; Rochat, B.; Decosterd, L.A. A LC–tandem MS assay for the simultaneous measurement of new antiretroviral agents: Raltegravir, maraviroc, darunavir, and etravirine.J. Chromatogr. B., 2009, 877, 1057-1069.
- Gupta, A.; Singhal, P.; Shrivastav, P.S.; Sanyal, M. Application of a validated ultra performance liquid chromatography–tandem mass spectrometry method for the quantification of darunavir in human plasma for a bioequivalence study in Indian subjects. J. Chromatogr. B., 2011, 879, 2443-2453.
- Heine, R.; Alderden-Los, C.G.; Rosing, H.; Hillebrand, M.J.X.; Gorp, E.C.; Huitema, A.D.R.; Beijnen, J.H. Fast and simultaneous determination of darunavir and eleven other antiretroviral drugs for therapeutic drug monitoring: method development and validation for the determination of all currently approved HIV protease inhibitors and non-nucleoside reverse transcriptase inhibitors in human plasma by liquid chromatography coupled with electrospray ionization tandem mass spectrometry. Rapid Commun. Mass Spectrom., 2007, 21, 2505-2514.
- Heine, R.; Rosing, H.; Gorp, E.C.M.; Mulder, J.W.; Steeg, W.A.; Beijnen, J.H.; Huitema, A.D.R. Quantification of protease inhibitors and non-nucleoside reverse transcriptase inhibitors in dried blood spots by liquid chromatography–triple quadrupole mass spectrometry. J. Chromatogr. B., 2008, 867, 205-212.
- Curran, A.; Gutirerrez, M.; Deig, E.; Mateo, G.; Lopez, R.M.; Imaz, A.; Crespo, M.; Ocan˜a, I.; Domingo, P.; Ribera, E. Efficacy, safety and pharmacokinetics of 900/100 mg of darunavir/ritonavir once daily in treatment-experienced patients. J. Antimicrob. Chemother., 2010, 65, 2195-2203.
- Rezk, N.L.; White, N.R.; Jennings, S.H.; Kashuba, A.D.M. A novel LC–ESI-MS method for the simultaneous determination of etravirine, darunavir and ritonavir in human blood plasma.Talanta, 2009, 79, 1372-1378.
- Ganduri, R.B.; Lanka, R.A.; Pamidi, S.; Peddareddigari, J.R.; Rao, J.V.L.N.S. New RP-HPLC method for the determination of darunavir in tablet dosage form.Asian J. Pharmaceut. Res.,2011, 1, 10-14.
- García, S.P.;Tunica, D.G.; Serra, M.B.Desarrollo y validación de un método para la determinación de darunavir en plasma mediante LC-MS/MS.Rev. Lab. Clin., 2011, 4,127-133.
- Sosnik, A.; Chiappetta, D.A.; Carcaboso, A.M. Drug delivery systems in HIV pharmacotherapy: What has been done and the challenges standing ahead. J. Controlled Release, 2009, 138, 2-15.
- Sharma, P.; Garg, S. Pure drug and polymer based nanotechnologies for the improved solubility, stability, bioavailability and targeting of anti-HIV drugs. Adv. Drug Delivery Rev., 2010, 62, 491-502.
- Kogawa, A.C.; Corrêa, J.C.R.; Salgado, H.R.N. Influence of darunavir:β-cyclodextrin complexo on the solubility of darunavir. RRJPTS, 2014, 2, 50-55.