"Occult Renal Cell Carcinoma with Initial Presentation of Pulmonary Embolism and Cervical Vertebra Metastases": Review
Ankit Bansal, Guru Dutta Satyarthee*
Department of Neurosurgery, Neurosciences Centre, AIIMS New Delhi, India
Abstract
Renal cell carcinoma presenting with pulmonary embolism is rare occurrence as evident by published few isolated case reports. However pulmonary embolism associated with compressive myelopathy as presentation is not reported. Authors reports a 32 – years - female who presented with complaints of rapidly progressing difficulty and shortness of breath along with numbness and spastic quadriparesis for seven days and also developing painful swelling involving right upper limb for 5 days. CT pulmonary angiography confirmed diagnosis of pulmonary embolism; Doppler study also revealed thrombosis of right basilic and cephalic veins and managed with anticoagulants. On further evaluation, she was detected to have mass lesion in right kidney and osteolytic lesion of C6 vertebral body. She underwent C6 corpectomy and anterior cervical plating followed by radical right nephrectomy. Our case is unique as it had both pulmonary embolism and cervical myelopathy as initial manifestation of renal cell carcinoma.
Keywords
Occult Renal Cell Carcinoma, Pulmonary Embolism, Surgery, Cervical Vertebral Osteolytic Lesion, Myelopathy
Received: July 31, 2015
Accepted: August 16, 2015
Published online: August 27, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
The renal cell carcinoma (RCC) comprises approximately 2-3% of malignant lesions in adult and associated with high incidence of early metastasis. About 20-30% patients may have distant metastasis at presentation, of these 1.6-3.6% cases include solitary bone metastasis and another 50% may develop during follow-up. 1,-4 It is the one of commonest neoplasm to metastasizing to the head and neck region, preceded only by breast and lung carcinoma.
2. Case Illustration
A 32 - year – old female presented to our emergency with complaints of rapid worsening of shortness of breath for seven days. She also developed numbness and weakness of all four limbs for same duration. She also noticed painful swelling of right upper limbs with increased swelling 5 days prior to admission. Although she had mild neck pain for last six weeks. Examination on admission revealed pulse rate 120/minute with respiratory rate 38 per min with prominent accessory muscle of respiration. She was immediately intubated and kept on ventilatory support. Auscultation showed diminished breath sounds in right infra maxillary and infrascapular region. Neurological evaluation showed spastic quadriparesis of grade upper limbs 2/5, and lower Limb 4/5. Plantars were bilateral extensor associated with graded sensory loss below C7 dermatomes.
Hematological test showed anaemia with positive D dimer test. Doppler study of right upper limb showed thrombosis of right basilic and cephalic veins. CT pulmonary angiography carried out at admission revealed pulmonary embolism. Lung perfusion scintigraphy showed matched perfusion and ventilation defects in medial, lateral, anterior basal, lateral basal and posterior basal segments of lower lobe of right lung. She was started on low molecular weight heparin and later on switched on oral anticoagulant therapy. Her respiratory symptoms improved gradually and weaned off from ventilatory support after 3 weeks. MRI abdomen showed mass lesion located at the upper pole right kidney, without hydronephrosis. (Fig 1). MRI cervical spine showed destruction of C6 vertebral body with epidural collection causing compressing and indentation of thecal sac (Fig 2, 3). Further NCCT cervical spine to evaluate the bone showed osteo lytic area involving body C6 vertebrae and also bilateral pedicle. (Fig 4a, b). She was planned for anterior cervical corpectomy of C6 vertebra and anterior cervical fusion using cervical plate. During surgery highly vascular mass was involving C6 vertebral body with destruction of sixth cervical vertebrae and C6 corpectomy and fusion using iliac crest graft and anterior plating was carried out. In the postoperative period her power improved and started ambulation and doing routine activity of living independently. Post- operative course was uneventful. Six week following anterior cervical fusion, she underwent right radical nephrectomy surgery. She received radiotherapy in the follow-up period. She is doing well at ten months follow-up after anterior cervical surgery with well controlled primacy and stable cervical spine.

Fig. 1. Contrast enhanced CT scan of abdomen showing heterogeneously enhancing renal cell carcinoma in right kidney.

Fig. 2. MRI cervical spine- sagittal section –show destruction of C6 vertebral body with epidural collection causing and thecal sac compression.
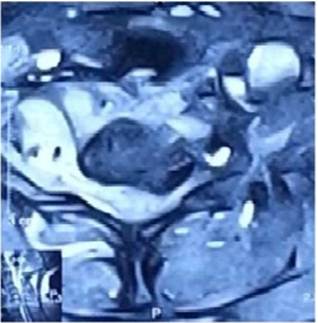
Fig. 3. MRI cervical spine, axial section image showing lytic lesion of C6 vertebral body associated with epidural collection causing compression and indentation of thecal sac.

a. sagittal view showing destruction and expansion of C6 vertebrae body with involvement of bilateral pedicle.

b. axial section depicting lytic lesion of vertebral body.
Fig. 4. Non-contrast cervical spine computerized tomography scan.

Fig. 5. Postoperative CT scan cervical spine showing excision of compressing mass extending into spinal canal with good decompression of spinal canal.
3. Discussion
The classical presentation of RCC comprises pain, mass in the flank region and hematuria as typical triad, however, characteristic symptoms can only be observed in approximately 10% of cases. Occult presentation of RCC as is observed in up to 30%, and is incidentally picked while radiological study carried out for other causes. 1, 3, 5.
Mostly first symptoms of RCC are resultant effect of metastatic lesions or paraneoplastic syndromes. High occurrence of occult RCC is attributed to extremely high vascularity of lesion, associated with multiple arteriovenous shunts caused by high expression of various growth factors including vascular endothelial growth factor, basic fibroblast growth factor and the platelet-derived growth factor.
The hematogenous spread is main route for systemic metastases of RCC. RCC most commonly metastasizes to the lungs (45 %), bone (29 %), lymph nodes (21 %) and the liver (20. %) [6], although metastasis to the neck region much rarer, and occur only in 5% cases. RCC can have bizarre manifestations including pulmonary embolism which may appear during any stage of patient illness, causing severe respiratory distress requiring urgent admission and care including ventilatory support. However, very unusually, pulmonary thromboembolism can be first presentation of occult RCC. 4, 7-9 Pulmonary emboli usually arise from thrombi that originate in the deep venous system of the lower extremities, other rare site include pelvic, renal, or upper extremity veins or the right heart chambers. 7
The thromboembolism presents as complication of underlying venous thrombosis and its classic presentation is of pleuritic chest pain of abrupt onset, hypoxia and difficulty of breath. Hematological tests D dimer test 10, arterial blood gases and total leukocyte count can be supportive. Imaging study like multidetector- C T angiography is the standard for diagnosing pulmonary embolism. Pulmonary angiography, when MDCTA is not available.
Immediate initiation of anticoagulant therapy and full anticoagulation is mandatory for all patients of suspected pulmonary thrombosis. Long-term anticoagulation therapy is administered for prevention of recurrence of deep venous thrombosis or pulmonary embolism. 11
She also noticed painful swelling of right upper limbs with increased swelling could be caused by weakness, immobilization or extension of thrombus from central venous canula or extension superficial thrombophlebitis,
The early diagnosis of spinal metastasis is important as prognostic indicator of functional outcome, which depend on neurologic status just prior to neurosurgical intervention. Vertebral body is the most frequent site in the vertebrae and predisposed by presence of bone marrow and abundant vascularity. The metastatic deposit cause substitution of the healthy bone by metastatic tissue and sometimes an acute pathological fracture can cause compression of neural structure with secondary spinal canal stenosis causing myeloradiculopaythy. Cervical spinal metastasis from RCC can also cause neck pain, compressive myelopathy and sensory loss. It is interesting to note that combined feature of thromboembolic event and feature of compressive myelopathy as initial presentation is not reported in the literature till date and represents first report of such cases in the world.
Our patient improved following decompressive anterior spinal surgery. 12 MRI is considered the gold standard technique for evaluation of spinal metastatic lesions; further fat suppressed MRI images can be useful in osseous lesions evaluation that may show contrast. However, imaging provides an accurate anatomical estimation, but biopsy of lesion in vertebra by suitable Ultrasound or CT guided is necessary. 7, 9, 11
The main role of surgery of metastatic spinal lesion is improvement of quality of life and treatment target of primary bone tumor is to preserve life. The best treatment is local control of the disease and restoration of the Spinal function. 13
4. Conclusion
Every cases of thromboembolism presenting to emergency services should be investigated for suspected occult malignancy including occult renal cell carcinoma and detailed history, systemic examination and detailed imaging is advised to early detection and provide prompt management and to avoid potentially treatable condition. A very high degree of vigilance is required to suspect such occult lesions.
References
- Leibovich BC, Pantuck AJ, Bui MH, Ryu-Han K, Zisman A, Figlin R, Belldegrun. A Current staging of renal cell carcinoma. Urol Clin North Am 2003; 30 (3): 481-97.
- Ogunyemi O, Rojas A, Hematpour K, Rogers D, Head C, Bennett C. Metastasis of genitourinary tumors to the head and neck region. Eur Arch Otorhinolaryngol 2010; 267:273–279.
- Griffin N, Gore ME, Sohaib SA: Imaging in metastatic renal cell carcinoma Am J Roentgenol 2007; 189:360-370?
- Kozlowski JM. Management of distant solitary recurrence in the patient with renal cancer. Contralateral kidney and other sites. Urol Clin North Am 1994; 21:601-624.
- Curti BD. Renal cell carcinoma. JAMA 2004; 292:97-100.
- Bianchi M, Sun M, Jeldres C, Shari at SF, Trinh QD, Brigantine A, Tian Z, Schmitges J, Graefen M, Perrotte P, Menon M, Montorsi F, Karakiewicz PI (2012). Distribution of metastatic sites in renal cell carcinoma: a population-based analysis. Ann Oncol 2012; 23:973-80.
- Daughtry JD, Stewart BH, Golding LAR, Groves LK. Pulmonary embolus presenting as the initial manifestation of renal cell carcinoma. Ann Thorac Surg1977; 24:178–181
- Gayer G, Mini S, Olchovsky D, Leibovitch I, Apter S, Weitzen R, Hertz M Pulmonary embolism initial manifestation of renal cell carcinoma in young woman. Emerg Radiol 2003; 10:43-5.
- King MB, Harmon KR Unusual forms of tumor embolism. Clin Chest Med 1994; 15:561–580.
- Schouten HJ, Geersing GJ, Koek HL, Zuithoff NP, Janssen KJ, Douma RA, van Delden JJ, Moons KG,Reitsma JB Diagnostic accuracy of conventional or age adjusted D-dimer cut-off values in older patients with suspected venous thromboembolism: systematic review and meta- analysis. BMJ 2013; 346: 2492.
- Trujillo-Santos J, Monreal M (2013) Management of unsuspected pulmonary embolism in cancer patients. Expert Rev Hematol.2013; 6:83-88.
- Arguello F, Baggs RB, Duerst RE, Johnstone L, McQueen K, Frantz CN (1990). Pathogenesis of vertebral metastasis and epidural spinal cord compression. Cancer 1990; 65:98–106.
- Alessandro Gasbarrini, Christiano Esteves Simões, Michele Cappuccio Stefano Boriani. Management of Renal Cell Carcinoma Metastasis of the Spine, Emerging Research and Treatments in Renal Cell Carcinoma, Dr. Robert Amato (Ed.), 2012; 311-335.