Intraoperative Contralateral Massive Extradural Hematoma Development During Decompressive Craniectomy and Evacuation of Traumatic Acute Subdural Hematoma Causing Brain Bulge: Management
Guru Dutta Satyarthee*, A. K. Mahapatra
Department of Neurosurgery, All India Institute of Medical Sciences and associated Jai Prakash Narayan Apex Trauma Centre, New Delhi, India
Abstract
Sequential development of extradural hematoma (EDH) during decompressive craniotomy and evacuation for acute subdural hematoma (ASDH) causing massive brain bulge is rare, it may represent to be first indication of hematoma development. About thirty seven cases are published in the form of isolated case report till date. Management is debated, as first to carry out exploratory burr-hole or necessity of getting CT scan head or intraoperative ultrasonography imaging to ascertain the diagnosis. Authors report a 40-year male, who developed EDH on contralateral side during evacuation of traumatic acute subdural hematoma during intraoperative period, wound was closed, patient was directly shifted to CT scan suit and got CT scan revealed ED, underwent evacuation of EDH by retuning back with good outcome. Awareness of occurrence of EDH development as a cause of massive intraoperative brain - bulge, which is not getting relieved on routine anaesthetic measure, may need urgent CT scan or at least intraoperative ultrasonography imaging is to diagnose early and provide appropriate management.
Keywords
Intraoperative, Extradural Hematoma, Brain Bulge, Decompressive Craniectomy
Received: July 6, 2015
Accepted: July 26, 2015
Published online: August 5, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Development of extra-axial haematoma on contralateral hemisphere during craniotomy surgery for evacuation of traumatic ASDH presenting with brain bulge is a potential life threatening complication, if existence of such occurrence not suspected. [1-8] It may present as extradural, subdural or intracerebral hematoma. However, development of ASDH is well reported in literature [3,9]. However, incidence of EDH, freshly developing is extremely rare, with paucity of literature, only reported in the form of isolated case report [1,4,8]. Intraoperative brain bulge can be commonly caused due to formation ipsilateral enlargement of hematoma volume or intra-parenchymal bleed, hydrocephalus enlargement or rarely but important causes are formation of ASDH, EDH on contralateral side. Authors report an interesting case of severe head injury with ASDH, who developed acute brain bulge intraoperatively during decompressive craniectomy, NCCT head revealed massive extradural hematoma, located on contralateral cerebral hemisphere associated with fracture of overlying calvarium to the surgical procedure, which necessitated emergency evacuation. Current study emphasizes getting immediate CT scan directly from operating room and return back to carry out urgent evacuation of hematoma can be a life saving measure without wasting of valuable time and providing golden opportunity for good neurological recovery.
2. Case Report
A-40-year male was brought in altered consciousness following trauma six hour back to our emergency services. Examination on arrival, vital stable with a G.C.S. Score of 8, with papillary asymmetry, immediately intubated and kept on ventilatory support. NCCT head showed thick left sided ASDH causing with effacement of basal cisterns with midline shift and significant mass effect (fig-1).
He underwent left frontotemporoprarieal scalp flap and decompressive craniectomy. Brain was lax after hematoma evacuation, however suddenly brain bulge noticed just prior to beginning of dural closure, all routine measure was taken to reduce he intracranial pressure, but no relief, so development of hematomas was possibility as it was not responding to routine anaesthetic measure. Hence a decision to get CT scan head after rapid wound closure was planned and shifted to CT scan suit and back to O.T. following NCCT head, which showed thick right sided parietal EDH with gross mid line shift. Decompressive craniectomy with EDH evacuation was carried out. He needed electively ventilated for five days. He was discharged on tenth postoperative day with GCS score of 14). (Fig-2). Subsequently he underwent split autologus cryogenic preserved skull flap cranioplasty at six months following first surgery (fig-3).
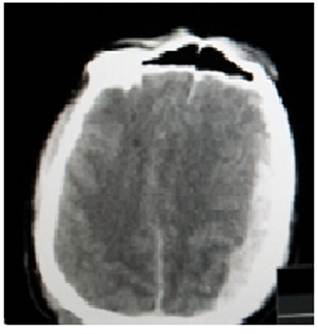
Fig. 1. Initial CT scan head showing thick acute subdural hematoma in left frontotemporo-parietal region causing effacement of basal cistern, subfalcine herniation and significant mass effect.
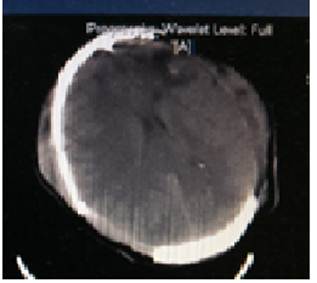
Fig. 2. Post-operative CT scan head showing complete evacuation of extradural and subdural hematoma.
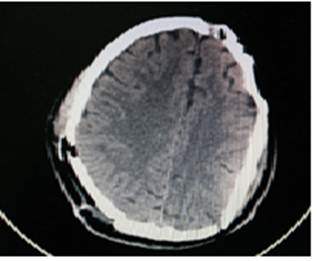
Fig. 3. CT scan with bone window showing cranioplasty utilizing autologus split cryogenic preserved skull flap.
3. Discussion
Development of extra-axial haematoma in opposite hemisphere in a sequential manner during craniotomy surgery for evacuation posttraumatic ASDH can be caused by epidural or subdural hematoma. Such occurrence is extremely rare but presents a challenge for accurate and rapid a diagnostic and surgical management.
Contralateral hemispherical evolution of ASDH development during surgery is reported literature [3,9,11]. However, EDH evolution during craniotomy or decompressive craniectomy surgery for traumatic SDH evacuation is still rarer. [1,4,6,7] In a review by Shen et al, found only 32 published cases, who developed contralateral EDH during craniotomy for traumatic acute SDH evacuation in 2013 [4]. However, exact mechanism of contralateral epidural hematoma development remains unknown. Various postulates are put forward to explain the intraoperative development of EDH, causing significant mass effect and brain bulge. Tomycz et al postulated rapid brain shift caused by craniotomy lead to shear stress on bridging veins of contralateral side, which may got torn leading to formation of EDH and ongoing collection of blood over time, may enlarge to cause brain bulge during surgery, which is unresponsive to anaesthetic mediation [9]. According to Takeuchi et al, early initial CT scan is usually done within few hours following injury and these scan may miss such hematoma development, which may represent as natural course of evolution [4]. However, Feuerman et al tried to define intraoperative hematoma as occurrence of hematoma, which are not observed during initial CT scan, but developing slowly following surgical evacuation either during surgery or in the immediate postoperative period [1].
According to chronology of evolution, such hematoma may manifest either in the period after completion of surgery or during intraoperatively. Former can present in the form of delay reversal from anaesthesia or development of fresh neurological deficit after recovery from surgery during convalescence in the postoperative period. Further, intraoperative development of EDH is much rarer, but can occur during any stage of surgical procedure of intracranial surgery i.e. bone flap elevation or following dura opening or during evacuation of hematoma phase, may present with catastrophic brain bulge as occurred in the current case.
Various factors have been incriminated to promote the evolution of epidural hematoma formation are usage of osmotic dehydrating agent during intraoperative period, hyperventilation, CSF rhinorrhoea, otorhorea, and presence of fracture of skull and may act either alone or in combination causing loss of temponade causing enlargement of EDH and leading to mass effect and rise in intracranial pressure. Authors also reported an interesting case, who developed contralateral epidural hematoma without overlying calvarial fractures as the source of EDH, was bleeding from superior saggital sinus [3]. In current case, fracture of overlying calvarium, compression and temponade effect of left sided ASDH with midline shift probably prevented contralateral extradural hematomas from developing but following evacuation of first hematoma led to decrease in intracranial tension, loss of temponade effect, increase intracranial circulation flow aggravated stripping of dura promoting arterial bleed causing attainment of massive size leading to intraoperative malignant brain bulge. Huang et al. observed remote EDH development in patients, who underwent unilateral decompressive hemicraniectomy for trauma, presence of remote skull fracture and absent contusion are independent risk factors and further observed such remote EDH development is devastating, timely CT scan head and urgent evacuation of hematoma are efficient and important factors determinig neurological outcome [2].
If acute brain bulge noticed intraoperatively, which fails to respond well to the anaesthetic maneuver routinely practiced i.e. head elevation, infusion of osmotic agent, diuretics, maintaining air way patency, avoidance of over-rotation of head, hyperventilation, switching over to total intravenous anaesthetic agent anaesthesia and in such resistant brain bulge. Routine intraoperative neurosurgical manoeuvre should be applied first to control further brain bulge, cisternal CSF release, ventricular tapping to release CSF are surgical adjunct. Another important indicator of remote bleeding during craniotomy is progressive brain bulge with recurrent oozing or venous bleeding in the surgical cavity causing repetitive failure to secure hemostasis. But in few cases, brain continue to bulge and not responding favourably to either surgical or anaesthetic maneuver, a possibility of remote hemorrhage should be kept. Awareness of such remote hematoma occurrence is very essential for neurosurgeons.
Ascertaining the causes of brain bulge and providing appropriate remedial measure is very important requiring urgent neuro-imagings. It can be diagnosed with intraoperative ultrasonography or CT scan or exploratory burrhole placement without imaging study or getting CT scan first and planning of subsequent surgery depends on immediate availability of CT scan or Ultrasound machine. However, CT scan of head is time consuming in addition requires shifting out and in off the operating room unless or institution having Intraoperative mobile CT scanner.
Management depends upon mass effect, size of hematoma, rate of progression of mass effect, effect of anaesthetic measure. A large acute EDH requires evacuation; however small contralateral EDH collection developing or detected in postoperative period can be monitored however, our case needed urgent surgical intervention. Singh et al advocated intraoperative anaesthetic measure, rapid closure of scalp wound without placing bone and getting immediate CT scan head and immediately shifting to operating room without delay and craniotomy with evacuation of extradural hematoma [5].
4. Conclusion
Acute brain budge during surgery may be first indication of developing contralateral extraxial collections or parenchymal contusions in severe head injury. Authors advocate getting rapid imaging is paramount importance, either intraoperative ultrasonography or urgent CT scan for proper diagnosis is important.
References
- Feuerman T, Wackym PA, Gade GF, Lanman T, Becker D. Intraoperative development of contralateral epidural hematoma during evacuation of traumatic acute subdural hematoma. Neurosurg 23: 480-484, 1988
- Huang YH, Lee TC, Lee TH, Yang KY, Liao CC. Remote epidural haemorrhage after unilateral decompressive hemicraniectomy in brain-injured patients. J Neurotrauma. 30(2): 96-101, 2013
- Sarkari A, Satyarthee GD, Mahapatra AK, Sharma BS. Delayed opposite frontal epidural hematoma due to bleeding from superior saggital sinus with no cranial fracture- a case report Indian J Neurotrauma 9:133-135, 2012
- Shen J, Pan JW, Fan ZX, Zhou YQ, Chen Z, and Zhan RY. Surgery for contralateral acute epidural hematoma following acute subdural hematoma evacuation: five new cases and a short literature review. Acta Neurochir (Wien). 155 (2):335-41, 2013
- Singh M, Ahmad F U, Mahapatra AK. Intraoperative development of contralateral extradural hematoma during evacuation of traumatic acute subdural Hematoma: A rare cause of malignant brain bulge during surgery. Indian Journal Neurotrauma (IJNT) 2: 139-140, 2005
- Su, Thung-Ming; Lee, Tsung-Han; Chen, Wu-Fu; Lee, Tao-Chen; Cheng, Ching-Hsiao. Contralateral Acute Epidural Hematoma after Decompressive Surgery of Acute Subdural Hematoma: Clinical Features and Outcome J Trauma-Injury Infection & Critical Care.; 65: 1298-1302, 2008
- Takeuchi S, Takasato Y Contralateral Acute Subdural Hematoma after Surgical Evacuation of the Initial Hematoma: Two Case Reports and Review of the Literature Turkish Neurosurg 23: 294-297,2013
- Thibodeau M, Melanson D, Ethier R. acute epidural hematoma following decompressive surgery of a subdural hematoma. Can Assoc Radiol J. 38(1):52-3, 1987
- Tomycz ND, Germanwala AV, Walter KA: Contralateral acute subdural hematoma after surgical evacuation of acute subdural hematoma. J Trauma68:E11-12, 2010
- Thibodeau M, Melanson D, Ethier R Acute epidural hematoma following decompressive surgery of a subdural hematoma. Can Assoc Radiol J. 1987; 38(1):52-3
- Satyarthee GD, Gaurang V., Sharma B.S., Contralateral development of massive acute subdural hematoma occurrence during decompressive craniectomy and surgery for evacuation of ipsilateral acute subdural hematoma: Literature review, Indian Journal of Neurotrauma 2014; 11: 118–121