A Study on the Prevalence and KAP Regarding Cervical Cancer Among Women Attending a Tertiary Care Hospital in Perambalur
T. Varadheswari1, Rahul Hanumant Dandekar2, *, T. Sharanya3
1Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu
2Dept. of Community Medicine,Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu
3Dept. of Obstetrics and Gynecology, Dhanalakshmi Srinivasan Medical College and Hospital, Siruvachur, Perambalur, Tamil Nadu
Abstract
Article title: A study on the prevalence and KAP regarding cervical cancer among women attending a tertiary care hospital in Perambalur. Background: The level of awareness on cervical cancer of the female population of Perambalur is unknown. Nevertheless, it is an important parameter for the development and monitoring of a screening program and for the follow-up of an eventual vaccination against HPV in the future. A positive attitude towards screening for premalignant cervical lesions can help in bringing down the prevalence of cervical cancer. Methodology: Seventy four women attending the OBG department at a tertiary care hospital in Perambalur were comprised the study population. Pap smear test was done for all the women to estimate the prevalence. A questionnaire was prepared and the women were interviewed to assess their knowledge, attitude and practices regarding cervical cancer. Results: Only one of the women had shown uncertain result (ASC-US) on screening cervical cancer. Intraepithelial neoplasia was not detected in any women participants at the end of screening. Twenty seven of the participants had good knowledge. About 56.75% of the study population had satisfactory knowledge while 6.75% had only poor knowledge about cervical cancer, its screening modalities and its significance. The participants had showed 83.78% positive attitude towards cervical cancer screening. The majority of participants were not undergoing screening for cervical cancer. Only 1.35% were found to have good screening practice on cervical cancer with 1.35% of the women having irregular. Conclusion: The study was revealed that though reasonable knowledge about cervical cancer present among half of the women participants, there was a very low screening rate in the community. This was mostly rendered towards the lack of proper infrastructure, facilities and partly towards the hesitation shown by the women.
Keywords
Cervical Cancer, Knowledge, Attitude, Practice
Received:April 9, 2015
Accepted: May 10, 2015
Published online: June 8, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
In India, cervical cancer is one of the leading causes of death in women and about 72,000 deaths are reported every year.1 As of 2002, the 1 year prevalence of cervical cancer in India was 101,583 and the 5 year prevalence was 370,243 accounting for approximately 26% of global prevalence.2Recent global estimates indicate cervical cancer is the third most common form of cancer diagnosed in women and the fourth leading cause of death due to cancer in women.3Cervical cancer is a proliferation of malignant cells that arise in cervical tissue and represents a continuum of conditions ranging from noninvasive to invasive carcinoma.6
Human Papilloma Virus (HPV) is the primary etiological agent of cervical carcinoma.2 High risk types in our country HPV 16, 18, 31, 33, 52, 58 accounts for most of the cervical cancer7 with HPV 16 and 18 contributing to about 76.7% incidence of cervical cancer.8Transmission of HPV occurs mainly by sexual contact or by skin to skin contact. Many of the predisposing factors for HPV infection including early age of sexual activity, early age at first birth, multiple births, tobacco use, immunosuppression, low socioeconomic status present in the community necessitates study of the knowledge of the disease and its screening which can be held at tertiary care hospital, Perambalur.9The persistence of an oncogenic HPV increases the likelihood of progressive disease.10
The cervical cancer becomes a preventable disease with the most effective method of prevention is through detection and treatment of premalignant lesions of the disease11. Further 91.7% believe cervical cancer could be treated if detected early enough.12 Cytology screening is a well-accepted intervention for the prevention and early identification of cervical cancer. The Pap smear technique has been the standard method of cervical cancer screening13.
Natural history of progression of cervical cancer takes 10 to 15 years to develop. Hence early screening has shown to effectively reduce the incidence of malignancy. In developing countries screening coverage is very ranging from 0.4% to 14% in rural areas and from 2% to 20.2% in urban areas14. For the screening methods to be fully utilized, women need to be aware of the various methods available. Thus, the knowledge, attitude and practice regarding cervical cancer have become essential to prevent disease.
2. Aims and Objectives
1. To estimate the prevalence of cervical cancer among women attending a tertiary care hospital.
2. To assess the knowledge of the participants on cervical cancer, its symptoms, risk factors, prevention and treatment.
3. To know the attitude and practice of women towards the screening methods.
3. Material and Methods
Type of study and Study design: It is a cross-sectional observational study. The study was carried out in Dhanalakshmi Srinivasan Medical College and Hospital, a tertiary care institute at Perambalur for 2 months duration form April and May 2014. It is a primary medical research type of study with focus on KAP among women regarding epidemiology of cervical cancer.
Study population: All women participants with age 18 years and above visiting the hospital in two months period were included in the study. All participants were given a full explanation of the project methodology and purpose with an assurance of confidentiality. Participants were also assured that their participation in the study was voluntary and that they could refuse to participate at any time during the interview.
Selection criteria: All participant women age 18 years and above comprised the study population. Exclusion criteria were set as active heavy vaginal bleeding, pap smear taken within last three years, history of total abdominal hysterectomy, women who were never sexually active, diagnosed case of carcinoma cervix, patients with placenta previa and patients delivered within last three months. Study participants were chosen by Systematic Random Sampling.
Sample size estimation: The sample size was calculated by the formula N= [Z² x P (1-P)]/ ε² (where N is required sample size, Z is reliability coefficient at 95% confidence interval, p is proportion of population with characteristics of interest is 26% as per 2002 WHO report 2 and ε is margin of error at 10%). Since N= 1.962 x 26x 74/ 10 x 10= 73.91, sample size was taken as 74.
Data collection procedures: The study participants were explained about the study in detail and were invited to take part in the study. The response sheets were filled, collected and checked for completeness by the author. The identification digits were used in place of names of women to maintain confidentiality.
Statistical analysis: The data will be entered and analysed with the help of Epi Info™ 7 software and Microsoft Excel software. The knowledge score was calculated by adding all positive responses of items, each item was assigned 1 for positive response and 0 for no response and then all items were included by applying a 12 points scale. Modified Bloom’s cut off points were used for assessment of knowledge. To assess the attitude of the participants, Likert’s scale was used.
Tools: A self-administered, structured, open ended and pretested questionnaire comprising of questions on the general characteristics, awareness, perceptions and actual practices of women was used to gather information about cervical cancer. The questionnaire was translated into Tamil language and explained in such a way that each of the participants understood the questions substantially for independent answers. The questionnaire was pilot-tested in a sample of 10 women who were not part of the study sample to ensure cultural acceptance and level of validity and degree of repeatability.
Ethical considerations with all required forms: The Ethical clearance for conduct of the study was obtained from the institutional ethical and research committee before starting the study. Informed consent was taken from all the study participants.
4. Results
A total of 74 participants took part in the study. Majority of the participants belonged to 40-50 years age group (74.3%). Only one of the participants was less than 20 years of age and two belonged to 20-30 years age group [Refer Table -1]. Of the 74 participants only one woman had undergone college and school education respectively. Most of them (78.3%) had no formal education and had never been to school. 17.5% of the participants have opted out of schooling with primary education [As shown in Figure -1]. Most of the participants were married women with only 1.3% of the women accounting for unmarried and another 1.3% for divorced. About 82.1% of the participants were multipara with more than 50% of them having two children. About 2.7% of the participants were nulliparous women [As shown in Figure -2].
Table 1. Distribution of respondents by socio-demographic characteristics (N=74).
| Socio-demographic characteristic | Number (n) | Percentage (%) |
| Age | ||
| <20 Years | 1 | 1.3 |
| 20 - 30 Years | 2 | 2.7 |
| 30 - 40 Years | 16 | 21.7 |
| 40 - 50 Years | 55 | 74.3 |
| Education | ||
| No Formal Education | 18 | 24.3 |
| Primary Education | 13 | 17.5 |
| School Education | 2 | 2.7 |
| College Education | 1 | 1.3 |
| Marital Status | ||
| Married | 72 | 97.2 |
| Unmarried | 1 | 1.3 |
| Others | 1 | 1.3 |
| Parity | ||
| Nullipara | 2 | 2.7 |
| Primipara | 11 | 14.8 |
| Multipara | 61 | 82.4 |
Table 2. Knowledge of the participants regarding cervical cancer screening.
| Responses | Number | Percent |
| Is there a way of screening for cervical cancer? | N=74 | |
| Yes | 63 | 85.13% |
| No | 3 | 4.05% |
| Don’t know | 8 | 10.81% |
| Who should be screened? | N=71 | |
| Any woman | 32 | 43.24% |
| Women of 25 years and above | 3 | 4.05% |
| Elderly women | 36 | 48.64% |
| Methods of screening for cervical cancer | N=71 | |
| Visual Inspection | 47 | 63.51% |
| Cytology(pap smear) | 24 | 32.43% |
| Don’t know | 19 | 25.67% |
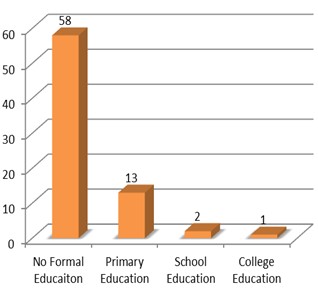
Figure 1. Education level of the respondents.
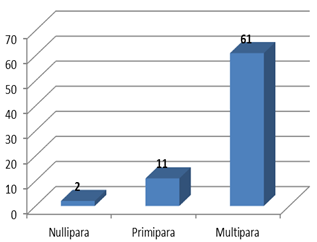
Figure 2. Parity of the study population.
4.1. Knowledge
Many of the participants (87.3%) believed that lower abdominal pain will be a symptom of cervical cancer. Menstrual problem associated with cervical cancer was mentioned by a comparative population of the women (71.6%). A less than half of the women believed that vaginal bleeding could be a symptom of cervical cancer. About a quarter of the respondents expected weight loss with cervical cancer [Refer Figure -3]. About 28.3% of the study population considered vaginal discharge to be a symptom of cervical cancer. Majority of the population, around 74.3% thought that having multiple sexual partners predisposes to cervical cancer. Also 62.1% of the population believed that a family history of cervical cancer shall be present. About thirty-three of the participants conceived that early onset of sexual activity predisposes to cervical cancer.[As shown in Figure – 4]. Seven of the participants thought presence of visual warts is another risk factor. When asked about the treatment modalities a bulk of the patients responded with surgical therapy to be the important option [As shown in Figure -5]. About 32.4% of the participants opted that chemotherapy could be another major modality of cervical cancer treatment.
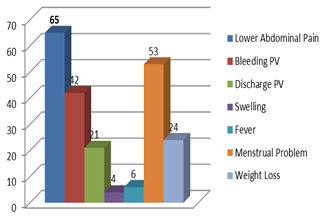
Figure 3. Knowledge of the respondents about the symptoms of cervical cancer.
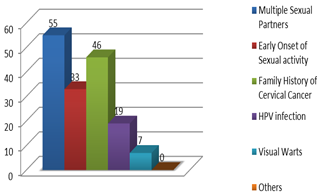
Figure 4. Knowledge of the respondents about the risk factors of cervical cancer.
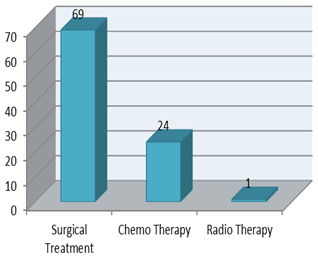
Figure 5. Knowledge of the respondents regarding the treatment modalities of cervical cancer.
4.2. Knowledge Score
The knowledge of carcinoma of the cervix and screening for premalignant cervical lesion was assessed using a 12 points scale. There were seven multiple choice questions that carried a total of 12 correct responses. Each correct response was given a score of 1 and a wrong response a score of 0. Total points to be scored were 12 and the minimum was 0. Points were about risk factors for acquiring the disease (any 3 points), symptoms of carcinoma of the cervix (any 3 points), preventive measures (any 2 points) and treatment modalities, availability of screening procedures, eligibility for screening, and frequency of screening and methods of screening. The Modified Bloom’s cut off points16was used for assessment with a score of 80-100% of correct responses meant a good knowledge, a score of 50-79% put a scorer in a level of satisfactory knowledge and a poor knowledge for a score less than 50% of the correct responses. Therefore the scores with the respective knowledge levels were good knowledge between 9 and 12, satisfactory knowledge between 6 and 8 and a poor knowledge with score between 0 and 5.
Table 3. Distribution of respondents by level of knowledge, attitude, practice (N=74).
| Variables | Number (n) | Percentage (%) |
| Knowledge | ||
| Good knowledge | 27 | 36.48% |
| Satisfactory knowledge | 42 | 56.75% |
| Poor knowledge | 5 | 6.75% |
| Attitude | ||
| Positive | 62 | 83.78% |
| Negative | 9 | 12.16% |
| Practice | ||
| Good practice | 1 | 1.35% |
| Irregular practice | 1 | 1.35% |
| No practice | 72 | 97.29% |
When asked if there was any way of screening for cervical cancer, 85.1% of the women responded positively while 4% of the women were unaware that there was any screening method. Eight of the participants did not know about screening for cervical cancer. Of the ones who responded yes, 43.2% believes that all the women should undergo screening while a slightly more number of participants (48.6%) conceive that it would be sufficient to screen elderly women alone. About 4% of the respondents think that women of 25 years and above should be screened. When demanded for the methods of screening, 63.5% of the study population was able to respond with visual inspection by the doctor as the answer [Refer Figure – 6]. Twenty-four of the participants stated that cytological examination helps in cervical cancer screening. About a quarter of the women (25.6%) of the women were unaware of any of the screening methods for cervical cancer. By applying Modified Bloom’s cut off points to our study it is obtained that twenty seven of the participants had good knowledge. About 56.75% of the study population had satisfactory knowledge while 6.75% had only poor knowledge about cervical cancer and its screening modalities [Refer Table – 3]
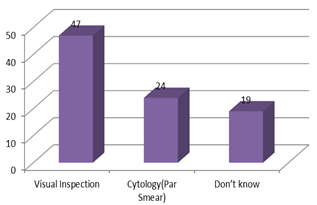
Figure 6. Knowledge of the participants about the methods of screening for cervical cancer.
4.3. Attitude
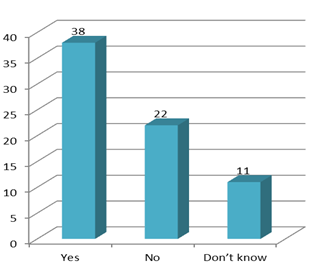
Figure 7. Responses given by the participants regarding transmission of cervical cancer from person to person.
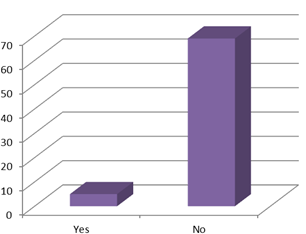
Figure 8. Responses of the participants if the screening procedure is costly.
Regarding the prevalence of cervical cancer in the country, about 81% of the participants were able to respond that carcinoma of the cervix is highly prevalent in the country whereas 2.7% of the women strongly objected that the disease is so rare in India. Another 12.1% of the women had no knowledge about the prevalence of cervical cancer. When asked who can acquire cervical cancer thirty-five women said that any woman can acquire it. About 48.6% of women believe that elderly women usually develop cervical cancer while 4% of the women believe women above 25 years of age acquire cervical cancer. More than half the participants think that cervical cancer can be transmitted from one person to another. 29.7% of the study population thinks that person to person transmission is not possible while another 14.8% of them had no idea if it could be transmitted from one to another [As shown in Figure– 7]. About 83.9% of the women believe that screening helps in the prevention of carcinoma of the cervix whereas 12.1% did not have any idea if screening helps in prevention or not. Only 2.7% of the women told that undergoing screening is a painful event while all the others said that screening does not cause any harm. About 6.7% of the population finds screening as a costly procedure [Refer Figure– 8]. When asked if the women would undergo screening if it was available free of cost and after ensuring that it does not cause any harm, only 2.7% of the respondents still remained hesitant to undergo screening but the rest of the population agreed.
4.4. Attitude Score
Attitude was assessed by seven questions put on Likert’s scale. The questions on Likert’s scale had positive and negative responses that ranged from strongly agree, agree, neither agree nor disagree, disagree and strongly disagree. The scoring system used with respect to participant’s responses is as follows: strongly agree 5, agree 4, neither agree nor disagree 3, disagree 2, and strongly disagree 1. The responses were summed up and a total score was obtained for each respondent. The mean was calculated and those who scored above the mean value has positive attitude and the ones who scored less than the mean value has negative attitude towards screening for premalignant cervical lesions. After applying Likert’s scale, among the study population 83.78% of the women were found to have positive attitude whereas more than one-tenth (12.16%) of the population had negative attitude towards cervical cancer screening [Refer Table – 3].
4.5. Practice
Of all the study participants, only 2.7% have undergone screening for cervical cancer. [As shown in Figure – 9]. Of those who had undergone screening no one have been screened two or more times indicating no frequent screening practice in the community. Among the participants only 1.3% has undergone screening within the past three years indicating that meager regular practice of screening. And 1.3% had undergone screening but not within the past five years indicating irregular screening practice.
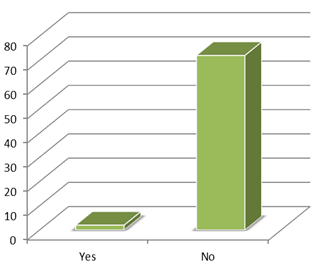
Figure 9. Response given by the participants regarding whether they have undergone screening before.
4.6. Practice Score
The practice was assessed by looking on the respondent’s screening activity. Those who ever screened within the past few years were regarded as having regular practice, those who ever screened but more than three years ago from the time of data collection were regarded as having irregular practice and those who never screened were regarded as having no practice on screening. In our study, as stated above only 1.35% were found to have good practice with another 1.35% of the women having irregular practice. 97.28% of the participants had no practice regarding cervical cancer screening [Refer Table – 3].
4.7. Prevalence
From the cytology test reports of the cervical smear sample of the participants it is found that only one of the women had uncertain result (ASC-US). No woman with intraepithelial neoplasia was found at the end of screening. One each of the women remained negative but with atrophic and menopausal changes. Two of the participants (2.7%) turned out to be negative with inflammatory changes [As shown in Table -4].
Table 4. Result of the cytology (Pap smear) test of the participants.
| Cytology results | Frequency (%) |
| Positive | 0 |
| Negative | 98.6 |
| Uncertain | 1.7 |
| Pattern of cytology results among positive respondents: | |
| High grade squamous intraepithelial lesion (HSIL) | - |
| Low grade squamous intraepithelial lesion (LSIL) | - |
| Atypical squamous cells of Undetermined Significance (ASC-US) | 1.7 |
| Pattern of cytology results among negative respondents: | 1.7 |
| Negative with atrophic changes | - |
| Negative with menopausal changes | 2.7 |
| Negative with inflammation | 98.6 |
| Negative (NSIL) | - |
5. Discussion
Cervical cancer is the most dreadful type of human cancer next to breast cancer15. It has been estimated that 100,000 new cases of cancer of the cervix occur in India every year and 70% or more of these are stage III or higher at diagnosis16. In our study among the participants it was found that only one of the women had uncertain result (ASC-US).
A study by Hoque et al. (2008) showed low uptake of Pap smear test and low level knowledge on prevention of cervical cancer and risk factors. Similarly our study also shows a very poor rate of screening by Pap smear test thus warranting urgent extensive health education program for this rural communities.17 Terefe and Gaym (2008) noted that most respondents had never heard of Pap smear screening. In our study 98.6% of the women had never undergone pap screening. This necessitates the need for social awareness programs to clear the fear and hesitation among women to undergo screening.18
Mathew and George (2009) suggested that Pap smear screening has played a significant role in the reduction in cervical squamous cell carcinoma (SSC) in the US, Canada, New South Wales and in almost all European countries as well as in some of the Asian countries.19 This again shows the significance of screening in reduction of mortality due to cervical cancer which is not at all practiced in a community like Perambalur. Poor knowledge and awareness of cervical cancer among women of different demographic and other characteristics has been reported from many countries20-23. But our study shows that nearly half of the study population had satisfactory knowledge about cervical cancer.
A Korean survey (Oh et al., 2010) found 31.5% women aged more than 20 years to know that sexually transmitted infections can cause cervical cancer24. Fifty-five of the participants of our study also recognized the same, comparably. A study by Ayinde et al., (2004) reported that 5.9% of the participants mentioned cost as one of the barriers of cervical cancer screening25. This is consistent with our study in a tertiary care hospital where 6.75% of the participants also found the screening procedure as a costlier one.
About 2.7% of our study participants conceived that undergoing screening procedure will be a painful experience. This misconception about the test being painful were found to be the barriers among women in another study among Arab women (Bener et al., 2001)26A study carried out in Houston, USA (Cyrus-David et al., 2002) suggested that age at first sexual intercourse less than 18 years carried a higher risk of developing Cervical Intraepithelial Neoplasia27. This was recognized as a risk factor for cervical cancer by 44.5% of our study population.
6. Conclusion
Seventy-four participants took part in the study. On screening only one of the women came out with uncertain result (ASC-US). 98.6% of the women were found to be negative on cytology test. The study was revealed that though reasonable knowledge about cervical cancer present among half of the women participants, there was a very low screening rate in the community. This was mostly rendered towards the lack of proper infrastructure, facilities and partly towards the hesitation shown by the women. Though majority of the women’s attitude was positive that has not contributed much to the practice of screening amongst them. Anyhow the women’s reluctance to undergo screening for cervical cancer appears to be based not only on lack of knowledge about cervical cancer and its risk factors but also lack of knowledge on the eligibility and availability of screening services.
Recommendations
The efforts to promote cervical cancer screening among women should focus on informing women of their susceptibility to cervical cancer. Women should be encouraged to take responsibility for their own health and be active participants in the screening programs. A woman undergoing gynaecological examination or seeking reproductive healthcare is more likely to receive a recommendation for a screening procedure.
Limitations
In the present study, sample size was low. In a vast community like Perambalur a large study population is required to know the exact prevalence or to understand their knowledge, attitude and practice regarding cervical cancer and its screening. Being a hospital based study; the reluctant people to attend the hospital were still not brought under the study.
Acknowledgements
Authors would like to acknowledge Indian Council of Medical Research (ICMR) and Secretary, Department of Health Research for approval of this research project through Short Term Studentship Program (STS 2015) and thereafter awarding it. Also, authors are very much thankful to Dhanalakshmi Srinivasan Medical College and Hospital Siruvachur, Perambalur– 621212, Tamil Nadu for supporting and funding this research project.
References
- Cervical Cancer Global Crisis Card. May report by the Cervical Cancer Free Coalition, a U.S.-based advocacy group. Available at: http://www.cervicalcancerfreecoalition.org/wp-content/uploads/Cervical-Cancer-Global-Crisis-Card_2013.pdf
- Park TW, Fujiwara H, Wright TC. Molecular biology of cervical cancer and its precursors. Cancer. 1995 Nov 15;76(10 Suppl):1902-13. Review.
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C, and Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, and Forman D. Global cancer statistics. CA Cancer J Clin. 2011 Mar-Apr;61(2):69-90.
- World Health Organization. Human papillomavirus and related cancers. Summary Report Update, June 22, 2010. 2010. Available at:http://screening.iarc.fr/doc/Human%20Papillomavirus%20and%20Related%20Cancers.pdf
- National Cancer Institute and U.S.Institute of Health. What is cancer: defining cancer. 2010. Available at: http://www.cancer.gov/cancertopics/cancerlibrary/what-is-cancer
- Robbins and Cotran ‘Pathologic Basis of Disease’8th edition
- Munoz N1, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ. Epidemiologic classification of human papillomavirus types associated with cervical cancer. International Agency for Research on Cancer Multicenter Cervical Cancer Study Group. N Engl J Med. 2003 Feb 6;348(6):518-27.
- Williams Gynecology Second edition by Hofman, Schore, Schaffer, Halvorson, Bradshaw,
- Kitchener HC et al and ARTISTIC Trial Study Group. ARTISTIC: a randomised trial of human papillomavirus (HPV) testing in primary cervical screening. Health Technol Assess. 2009
- ‘Textbook of Pathology’by Harsh Mohan 6th edition
- Yu CK, Rymer J. Women’s attitudes to and awareness of smear testing and cervical cancer.Br J Fam Plan. 1998; 23(4): 27-33
- Pap smear and Cervical Cancer Screening: Accessed from MedIndia on 10th October 2014 www.medindia.net/patients/patientsinfo/cervialcancer.htm
- K. S. Louie, S. De Sanjose, and P. Mayaud, "Epidemiology and prevention of human papillomavirus and cervical cancer in sub-Saharan Africa: a comprehensive review," Tropical Medicine and International Health, vol. 14, no. 10, pp. 1287–1302, 2009.
- Mitra S. Study of the risk factors for cancer cervix in a speciality hospital in Kolkata. J of Community Medicine,5,1-5.
- Nandakumar A, Anantha N, Venugopal TC. Incidence, mortality and survival in cancer of the cervix in Bangalore, India. Br J Cancer. 1995 Jun; 71(6): 1348–1352.
- Hoque M, Hoque E, Kader SB. Evaluation of cervical cancer screening program at a rural community of South Africa. East Afr J Public Health. 2008 Aug;5(2):111-6.
- Terefe Y, Gaym A. Knowledge, attitude and practice of screening for carcinoma of the cervix among reproductive health clients at three teaching hospitals, Addis Ababa, Ethiopia. Ethiopian J of Reproductive Health, 2, 14-7.
- Mathew A, George PS. Trends in incidence and mortality rates of squamous cell carcinoma and adenocarcinoma of Cervix-worldwide. Asian Pac J Cancer Prev. 2009 Oct-Dec;10(4):645-50.
- Lambert EC. College students’ knowledge of human papillomavirus and effectiveness of a brief educational intervention. J Am Board Fam Pract. 2001 May-Jun;14(3):178-83.
- Ralston DJ, Taylor VM., Yasui Y et al. Knowledge of cervical cancer risk factors among Chinese immigrants in Seattle. J Community Health. 2003 Feb;28(1):41-57.
- Peter NA, Navkiran KS. Cervical cancer screening among college students in Ghana: Knowledge and health beliefs. Int J Gynecol Cancer.2009 Apr;19(3):412-6.
- Wong LP, Wong YL, Low WY, et al. Knowledge and awareness of cervical cancer and screening among Malaysian women who have never had a Pap smear: A qualitative study. Singapore Med J. 2009 Jan;50(1):49-53.
- Oh JK, Lim MK, Yun EH, Lee EH, Shin HR. Awareness of and attitude towards human papillomavirus infection and vaccination for cervical cancer prevention among adult males and females in Korea: A nationwide interview survey. Vaccine. 2010 Feb 17;28(7):1854-60.
- Ayinde OA, Omigbodun AO, Ilesanmi AO. Awareness of cervical cancer, papanicolaou’s smear and its utilisation among female undergraduates in Ibadan. Afr J Reprod Health. 2004 Dec;8(3):68-80.
- Bener A, Denic S, Alwash R. Screening for cervical cancer among Arab women (brief communication). Int J Gynecol Obstet, 74, 305-7.
- Cyrus-David MS, Michielutte R, Paskett ED, DAgostino R Jr, Goff D. Cervical cancer risk as a predictor- pap smear use in rural North Caroline. J Rural Health. 2002 Winter;18(1):67-76.



