Hematological Profile of Sudanese Patients with Systemic Lupus Erythematosus
Khalda Mirghani Hamza*, Zeinab Mohamed Bashir
Department of Hematology and Immunohematology, College of Medical Laboratory Science, Sudan University of Science and Technology, Khartoum, Sudan
Abstract
This is a case control study aimed to evaluate hematological status of Sudanese female patients with Systemic Lupus Erythematous. The objective off the study is to assess hematological profile of Sudanese patients with Systemic Lupus Erythematosus. Fifty SLE patients and 50 apparently healthy females were enrolled in the study. Age of participants ranged from 18 to 62 years with 64% with age less than 40 years. Hb was 11.2 ± 1.9 g/dl compared to 12.7 ± 1.1 g/dl in control group (p = 0.000). RBC and PCV significantly decreased (p = 0.000, 0.003) respectively. Neutrophils count was 4.1 ± 2.1× 103 µl compared to 3.0 ± 1.1× 103 µl in control group. Anemia and infection are frequent among SLE patients. Thrombocytes remained within normal range. In conclusion, most common age of SLE patients ranged between 18 and 40 years.
Keywords
Systemic Lupus erythematosus, Hemoglobin, Anemia, Neutrophilia
Received:June 14, 2016
Accepted: July 1, 2016
Published online: August 5, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
SLE is a chronic inflammatory disease of unknown cause that can affect virtually all organs of the body. Immunological abnormalities, especially the production of antinuclear antibodies (ANA) are a prominent feature of the disease [1].
SLE is chronic auto-immune-disease that can be fatal. It is one of the types of lupus which affects multiple organ systems and it is multi-factorial in etiology [2].
Although the causes of SLE remain unknown, considerable evidence has been accumulated to the pathological failure of autoimmune mechanisms. Genetic, hormonal and environmental factors has been attributed certain roles of autoimmunity [3]. Multiple factors are associated with SLE development without specific cause these include, genetic, racial, hormonal and environmental factors [4].
SLE is a common autoimmune disease throughout the world. It varies from 40 -100 per 100.000. In India, the prevalence is 3.2 per 100.000 [5].
Estimation of the incidence and prevalence of SLE in the UK over the period from 1999 to 2012 showed that the incidence was 4.91 per 100.000 persons per year (with an annual 1.8% decline. The prevalence increased from 64.99 per 100.000 in 1999 to 97.04 in 2012 [6]. Among Michigan population of 2.4 million people, incidence and prevalence was 5.5 per 100.000 and 72.8 respectively. Among females, the incidence was 9.3 per 100.000 and the prevalence was 128.7 per 100.000 persons [7]. During the period from 2001 to 2009, 183 new case of SLE (98%) African Caribbean population, affecting 172 women and 11 males. Incidence rates in males compared to females were 12.21 to 0.84 per 100.000 persons per year respectively [8].
A study in Sudan revealed that, the disease was most frequent in tribes of mixed ethnicity (Afro-Arab), and least common in pure African tribes. Afro- Arab ancestry constituted 94.3% of the sample, whereas subjects from Nubian ancestry were 5.7% of the study group. No subjects from Southern or Western Sudan tribes. Female to male ratio = (20.6: 1) with mean age at diagnosis was 31.9 years [4].
SLE is rare in West Africa, increasing in frequency in Central and Southern Africa Despite improvement in overall survival rates, patients with SLE, still have a death rate that is three times that of general population and increasing up to 4.0 and 4.92 folds have been reported in some studies [4]. SLE prevalence was 2-3 folds higher in black persons than in white and 10 – fold higher in females than males. Black SLE patients had a higher proportion of renal disease and end- stage renal disease (40.5% and 15.3% respectively) as compared to white persons (18.8% and 4.5% respectively) [7]. Black women had an incidence rate nearly 3 times higher than white women with a significantly higher rate in the age group 30 -59 years. An epidemiological study from 1956 to 1965 showed for the first time a higher burden of the disease in black women compared to white women. In 2002-2004, a total of 267 SLE cases including 196 black patients, 62 white patients and 9 patients of other racial groups [9].
88% of patients having SLE were females. The prevalence of SLE was 47.1 per 100.000 and the WHO standardized rate = 40.8 per 100.000. Annual incidence in (2010) was 3.32 per 100.000 with peaks in female age between 30 -39 years and in males aged 50- 59 years [10].
Among women age adjusted rates in black persons were 3 times higher than white persons 13.4 versus 0.7[9]. In women, prevalence rates vary from 164 (white) to 406 (African American) per 100.000. Estimated incidence rates are 1 to 25 per 100.000 in North America, South America, Europe and Asia. Both Geographical and race affect the prevalence of SLE and frequency and severity of clinical and laboratory manifestations. The disease appears to be more common in urban than rural areas [11]. Female dominance = 94.2%. [12]. SLE in women has a high prevalence in Afro- Caribbean populations but has been to be rare in West Africa. Prevalence in women (per 100.000), of SLE in women in an area of south London are estimated to be 177 in Afro-Caribbean’s, 110 in west Africans and 35 in Europeans [13]. The mean age was 35 ± 7.5 years. Out of 33 patients 31 (94%) were females, 2 were males and F/ M ratio was 15.5: 1 [14].
Hematological abnormalities (hemolytic anemia, leukopenia, lymphopenia and thrombocytopenia [2] and anti-phospholipid syndrome (APS) [15] are common manifestation in patients with SLE. Most of the patients exhibit anemia at some point during their disease course. The causes of anemia in these patients may be of immune or non-immune pathogenesis [2]. The most common cause of death in SLE is infection due to immune suppressive medication used to manage the disease.18 (54.5%) out of 33 patients had various infections [13]. Leucocytosis can occur in SLE and is usually due to infection or use of high doses of glucocorticoids. Lymphocytopenia has been observed in 20 to 75% of patients, particularly during active disease. Neutropenia in patients with SLE can results from, immune mechanisms, medications, bone marrow dysfunction [15]. Thrombocytopenia is a major hematological complication in patients with SLE [16-17]. The most common mechanism is believed to be increased platelet clearance mediated by anti- platelet autoantibodies [17].
2. Materials and Methods
This is a case control study conducted in 2014 at Omdurman Military Hospital – Khartoum State. The study aimed to assess complete Blood Cell Count of Sudanese patients with systemic lupus erythromatosus (SLE).
Fifty females already diagnosed with SLE and 50 apparently healthy females as a control subjects were enrolled in the study. Age of patients and control subjected ranged between 18 – 62 years.
Inclusion Criteria: female patients already diagnosed with SLE by clinical symptoms and anti-nuclear antibodies (ANA) profile test who attended Omdurman Military Hospital during the study period.
Exclusion Criteria: Female patients with any disease that may affect the hematological parameters under study such as thalassemia or iron deficiency anemia.
A designed questionnaire was used to obtain all required information concerning the study. An informed consent was obtained from each participant before sample collection. Clinical data was obtained from clinical record of each patient.
Sample collection: 2.5 ml venous blood was collected in EDTA container and Complete Blood Cell Count was determined using automated hematological analyser Sysmex (XT 2000 i).
SPSS software computer program was used to obtain independent t- test, significant level was set at p ≤ 0.05.
3. Results
Table 1. Age frequency of study group.
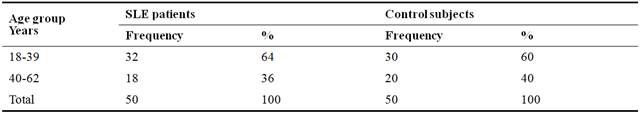
64% of patients with age ranged between 18 to 39 years compared to 36 5% with age above 40 years. This indicated that SLE is more frequent at child bearing age which was confirmed by previous investigators.
Table 2. Frequency of SLE patients according to duration of SLE.
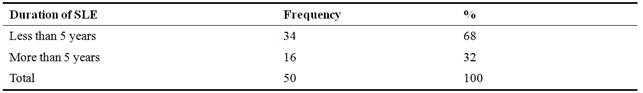
At time of presentation, 68% of patients have SLE on set in less than 5 years, compared to 32% of patients have the disease in more than 5 years. This showed that frequency of SLE increased.
Table 3. Hematological Profile of SLE patients compared to Control Subjects.
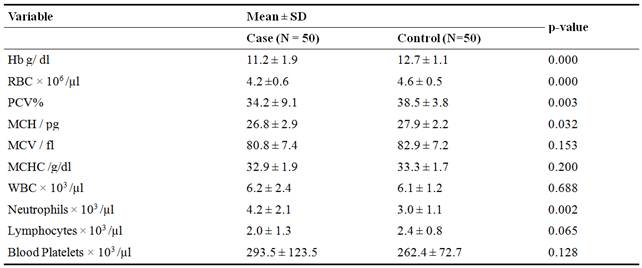
Hemoglobin RBC count, PCV and MCH of patients significantly decreased compared to control. This indicates that the patients were subjected to anemia as reported by many previous studies. White blood cell count increased but insignificantly indication of infection which is often associated with SLE due to immunosuppressive mechanisms. MCH, MCHC and blood platelets remains within normal range. Neutrophils significantly increased in patients compared to control subjects which indicated the association of SLE with infection. Neutrophils are the most abundant circulating lymphocyte population and their major function is the release of proteolytic enzymes, increases apoptosis and aggregation and impaired phagocytosis.
Table 4. Hematological Profile of Patients according to SLE Development.
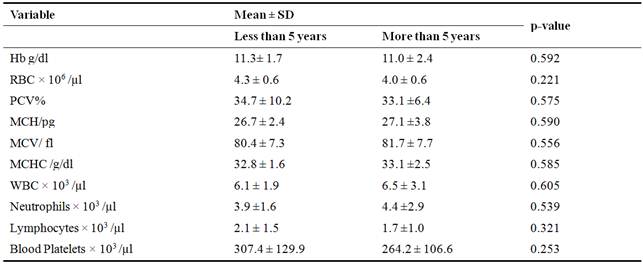
According to duration of the disease, no significant change was observed in hematological profile of SLE patients at different duration of SLE on set. Two factors may contribute to these findings, medication to which patients were exposed and blood transfusion may improve health status of patients. Another factor worth considering is the limitation of samples may not reflect the changes in hematological status of SLE patients.
4. Discussion
All the selected patients were females, since SLE was more common among females compared to males. Many investigators pointed to the possible involvement of multiple factors associated with SLE development such as genetic, hormonal and steroid gonadal hormones [2, 7, 10, 12, 14, and 18]. SLE usually affects young females, the causes are unknown but genetic, environmental and hormonal factors may contribute [12]. Beside genetic and hormonal factors, immunological factors could be another possible cause [2], since fetal cells can persist in mothers circulation for decades after delivery which provide antigenic exposure that may be a source of immune reactions in women
According to the results of the present work, the most frequent age of patients ranged from18 to 39 years which is considered as the child bearing age. This is well documented by many researchers [2,7,10,14,18,9]. Some authors found that the mean age of SLE patients ranged from 35 ± 7.5 to 39. ± 16.6 years [7,14,8]. In another study, the mean age was 28 ± 6.2 years [2]. Being a reproductive age worsens the situation and put this target group at risk.
Changes in hematological profile of SLE patients was observed (table 3), similar findings have been reported by previous authors who concluded that hemolytic anemia, leukopenia, lymphopenia and thrombocytopenia are common manifestation in patients with SLE [2,20].
Anemia was frequent among SLE patients compared with control (table 3) which is evident by significant decrease in Hb level, RBC count and PCV. These findings were confirmed by many previous studies [[1, [14, [15,[ 19, and [21]. Many mechanisms contribute to the development of anemia, including inflammation, renal insufficiency, blood loss, infection. A frequent cause of anemia in SLE is suppressed erythropoiesis from chronic inflammation (anemia of chronic disease or anemia of chronic inflammation), being the most common form (60 to 80%). This type of anemia is normocytic normochromic [15]. Many authors stated that ACD and IDA are the most frequent types of anemia among SLE patients [2,19,20]. The same authors relate these types of anemia to inflammation, EPO impairment and disturbance in iron hemostasis. Iron deficiency anemia was found in 9 (30%) patients, 12 (40%) had anemia of chronic disease and 7 (23.33%) patients had hemolytic anemia. Anemia of chronic disease which is the second more prevalent after iron deficiency anemia, occurs in patients with acute or chronic immune activation. Some authors associated causes of SLE development to immunological and non-immunological pathogenesis [2]. Other investigator related ACD to immunological causes, since, cytokines and cells of reticuloendothelial system induce changes in iron hemostasis, the proliferation of erythroid progenitor cells, the production of erythropoietin, and the life span of red cells leading to disturbance of iron hemostasis, which increased up and retention of iron within cells of reticuloendothelial system [2]. A study in Athens showed in 132 SLE patients, anemia of chronic disease (ACD) was 49 (37.1%), iron deficiency anemia (IDA) was 47 (35.6%), autoimmune hemolytic anemia (AHA) n 19 (14.4%) and other causes was 17 (12.9%). Recently suggested, autoantibodies, T lymphocytes and deregulation of the cytokines network can affect bone marrow erythropoiesis leading to anemia [20].
Evidence for infection is derived from increase in WBC count and neutrophils of SLE patients compared with control (table 3). Similar findings was previously reported which related leucocytosis to SLE patients due to infection [22], or due to high doses of glucocorticoids [15]. Another study further confirmed the results of the present study which revealed that the most common cause of death in SLE is infection due to immune suppressive medication used to manage the disease,18 (54.5%) out of 33 patients had various infections [14]. Other investigators reported that due to inherent immune abnormalities and immune suppressive treatment they are exposed to, patients with SLE are highly susceptible to infection [23]. In consistent findings revealed that leukopenia was found at the time of diagnosis in 51.6% SLE patients and leukopenia was common in SLE but usually not persistent and the association between leukopenia and infection is a time dependent relationship. Thus the number of WBC at diagnosis or at only one time point may not predict an infection in subsequent times [18].
Neutrophils of SLE patients significantly increased compared to control subjects (table 3). There is a controversy in the literature regarding the association of neutrophils with SLE [15,18,23,27]. Many researchers correlate neutrophils count to SLE [15,26,28], and neutropenia in patients with SLE can results from, immune mechanisms, medications, bone marrow dysfunction [15]. Another study showed that circulating neutrophils from SLE patients released more neutrophil extracellular traps (NETs) than those from healthy donors, this was further stimulated by the antimicrobial autoantibodies, suggesting a mechanism for the chronic release of immunogenic complexes in SLE, these data establish a link between neutrophils and autoimmunity in SLE, providing new potential targets for the treatment of this devastating disease [26]. Furthermore recent discoveries implicate neutrophils as important regulators of innate and adaptive immunity and in the development of organ damage in SLE. Various putative biomarkers are neutrophil related, including neutrophil granular proteins and histones [28]. Other researchers [23-25], found no correlation between neutrophils function and clinical activity of SLE [23,25]. Other study reported a role of neutrophils in the pathogenesis of SLE, but the exact nature of their contribution remains unknown [24].
No significant difference in lymphocytes of patients compared to control group, although, many authors reported that lymphopenia was a common hematological abnormality among SLE patients with prevalence ranges from 20 to 81% and its degree may correlate with disease activity both T and B lymphocytes are reduced. Furthermore, there are numerous reports of lymphotoxic antibodies in SLE with frequency ranged from 36-90% but their pathogenic significance remains unclear. [27]. The association between leukopenia and severe infection remains controversial in SLE. Some studies showed lymphopenia at presentation and neutropenia associated with infection in SLE, but other studies do not support the role of leukopenia as predisposition to severe infection in SLE [18]. However, Lymphopenia is reported in 15-82%, some studies found strong association between low lymphocytes, neutrophils count and the risk of infections [29].
Thrombocytes remained within normal range (table 3) since 34% of patients received blood transfusion as a part of treatment which may improve their health status. Previous investigators reported thrombocytopenia as a major hematological complication in patients with SLE and the most common mechanism is believed to be increased platelet clearance mediated by anti- platelet autoantibodies [17,30]. Other authors related thrombocytopenia seen in SLE patients to adverse effects of medication, hypersplenism [16], or presence of antibodies against thrombopoietin and some thrombopoietin receptor have been found in some thrombocytopenic patients with SLE [30], or due to platelet consumption associated with hemolytic anemia [15].
The inconsistency of results of the current study compared with previous studies could be due to many reasons, of these the limited sample size of study group; secondly, all patients were under treatment. So, more investigation is highly recommended to clarify the association of WBC differential count as indicator to infection and its role in pathogenicity of SLE, since vaccination may be a new reliable option to reduce risk of infection in SLE patients [22].
5. Conclusion
Anemia, leucocytosis and neutrophilia are common hematological features among SLE Patients. No significant difference in hematological profile of patients with respect to SLE on set. Further study is recommended to identify most common types of anemia associated with SLE.
References
- Daniel J Wallace. Diagnosis and differential diagnosis of systemic lupus Erythematosus.2015.http://www.Uptodate.com. Wolters Kluwer.
- Mumatz Ali Shakih, Igbal Memon and Rafi Ahmed Ghori. Frequency of Anemia inPatients with systemic lupus erythematosus at Tertiary Care Hospital. Journal ofPakistan Medical Association JPMA2010; 60:822.
- Robert G. Lahita. Systemic Lupus Erythematosus. 4th edition. International StandardBook 0-12-433901-8. 2004. Elsevier Academic Press.
- Babikir G K, Abubakr A W, Musa M N, et al. Ethnic distribution and clinical features ofSystemic lupus erythematosus. Sudan Medical Journal 2009; 45(2):49-57.
- Rudrajit P, Pradip R, Pradip K S, et al. Prevalence of Systemic Lupus ErythematousAmong patients of hyperthyroidism in a tertiary care centre. Indian Journal EndocrinolMetab2012; 16(4):569-574.
- Frances R, Michael D, Mathew G, et al. The Incidence and Prevalence of SystemicLupus Erythematous in UK. 1999-2012. Ann Rheum Dis 2014; doi: 10.1136/ annrheum-2014- 206334.
- Somers EC, Marder W, Caqnoli P, et al. Population – based incidence and Prevalence ofSystemic lupus erythematosus. Journal of Arthritis Rheumatol 2014; 66(2):369-378.
- Flower C, Hennis AJ, Hamblton IR, et al. Systemic Lupus Erythematosus in an AfricanCaribbean population: incidence, clinical manifestations and survival In the BarbadosNational Lupus Registry. PubMed. Arthritis Care Res 2012; 64 (8):1151-1158.
- S. Sam Lim, A. Rana Bayakly, Charles G. H, et al. The Incidence and Prevalence of SLE2002-2004. The Georgia Lupus Registry. Journal Arthritis and Rheumatology 2014;66(2):357-368.
- Arnaud, Laurent, Fagot, et al. Incidence and Prevalence of SLE A 2010 Nation – WidePopulation – Based Study using French National Administrative Database. JournalArthritis and Rheumatoid2013; 65(10):1067.
- Peter H Schur, and Bevara H Hahh. Epidemiology and Pathogenesis of SLEhttp://www.uptodate.com. 2015. Updated 2015.
- Hassan A A Eltom, Hyder O M, Tayseer H A, et al. Clinical Implications of thePresence of Anti Ro Antibodies in Systemic Lupus Erythematosus in Sudan. SudanJournal of Medical Sciences2015; 10(3):93-98.
- Molokhia, M; MC Keigue, PM; Caudrado, M; Hughes, et al. Systemic LupusErythematous in Migrants from West Africa compared with Afro-Caribbean people.Lancet2001; 357(9266):1414-5.
- Shaikh M A, Jehangir S and Rizwan C.Various Modes of Presentation of SystemicLupus Erythematosus at a Tertiary Care Hospital. Original Article. Medical Channel(MC)2011; 17(2):42-45.
- Janoudi Nahid and Bardisi Ekhlas S. Hematological Manifestations in SystemicLupus Erythematosus. Saudi Arabia. Text book. ISBN 978-953-51- 0266-3. 2012Publishers: In Tech. Chapter 17:364-382.
- Arthur K. Thrombocytopenia Assed with Systemic Lupus Erythematosus. MedscapeRheumatology2001; 3(1).
- M. Kuwana, J. Kaburaki, Y. Okazaki, H. Miyazaki and Y. Ikeda. Two types ofAutoantibody- mediated thrombocytopenia in patients with systemic lupus erythematosus.Oxford Journals Medicine and Health Rheumatology2006; 45(7):851-854.
- Kamoltip L, Nuntana K, Suparaporn W, et al. An Evaluation of the Association ofLeukopenia and Severe infection in Patients with Systemic Lupus Erythematosus. J.Clin Rheumatol2013; 19 (30):115-120.
- Michalis V, Styliani I G Kokori, John P A Loannidis, et al. Anemia in Systemic LupusErythematous: etiological profile and the role of erythropoietin. Ann Rheum Dis 2000;59:217-222.
- S Giannouli, M Voulgarelis, P D Ziakas and A G Tzioufas. Anemia in Systemic LupusErythematosus: from Pathophysiological to Clinical Assessment. Annals of the RheumaticDiseases2006; 65(2):144-148.
- Hirano, Y., Itonaga, T., Yasudo, H, et al. Systemic lupus erythematosus Presenting withMixed-type fulminant autoimmune hemolytic anemia. Paediatrics International.2016. doi: 10.1111/ped.12849.
- Murdaca G, Orsi A. Spano F, et al. Vaccine – preventable infections in Systemic LupusErythematous. Hum Vaccin Immunother 2016. PubMed.
- D. Martinez-Banos, J. C. Crispin, A. Lazo and J. Sanchez-Guerrero Moderate andSevere Neutropenia in Patients with Systemic Lupus Erythematosus.Rheumatology2006;45(8): 994-998.
- Nick Ward. Autoimmunity: The Role of Neutrophils in SLE untangling the Net. NatureReview Rheumatology2011; 7:252.
- H Al-Hadithy, D A Isenberg, I E Addison, et al. Neutrophils Function in Systemic LupusErythematosus. Ann Rheum Dis 1982; 41(1): 33-38.
- Roberto L, Dipyaman G, Valeria F, et al. Neutrophils Activate Palsmacytoid DendriticCells by Release Self- DNA – Peptide Complexes in Systemic Lupus Erythematosus.Science Translation Medicine2011; 3(73):73ra19.
- Alastair L. Hepburn, Santosh N and Justin C Mason. The Management of peripheralBlood cytopenias in Systemic Lupus Erythematosus. Rheumatology 2010; 49(12):2243-2254.
- Carolyne K S and Mariana K. The Role of Neutrophils in the Pathogenesis of SystemicLupus Erythematosus. PubMed. Current Opinion in Rheumatology. 2015; 27 (5).
- Linda C, Chiara, Sabrina V, et al. Leukopenia, Lympnopenia and Neutropenia inSystemic Lupus Erythematosus: Prevalence and Clinical Impact. 2015; 45(2): 190-194.doi: http://dx.doi-org/ 10.1016/I: Semarthrit.Elsevier.
- Bashal F. Hematological Disorders in Patients with Systemic Lupus Erythematosus.Open Rheumatol Journal2013; 7:87-95.



