Hematological Profile of Patients with Visceral Leishmaniasis at Al-Gaderf State - Sudan
Amna El-Sadig El–Safi, Al-Sara Khalid Adm, Khalda Mirghani Hamza*
Department of Hematology and Immune-Hematology, College of Medical, Laboratory Science, Sudan University of Science and Technology, Khartoum, Sudan
Abstract
This is a case control study conducted during the years (2010-2011) at Al-Gaderf Teaching Hospital, Sudan. The objective of the study is to assess the hematological profile of patients with Visceral Leishmaniais admitted to Al-Gaderf Teaching Hospital. The patients were divided into 2 groups; group A: paediatric Visceral Leishmaniasis 50 patients under 14 years old, 33 (66%) were males and 17 (34%) were females. Complete Blood Cell Count was determined using fully automated hematological analyzer Sysmex KX 21N. Group B included 50 visceral leishmaniasis patients with different age groups, 26 (52%) were males and 24 (48%) were females. Hemostatic profile was determined manually determined. An informed consent was obtained from gardeners of paediatric patients and directly obtained from adult patients. Most affected paediatric patients with age less than 10 years. Among adult patients the most frequent age group ranged between 21 and 30 years. Both Males and females were infected, but males showed higher frequency. Significant decrease was observed in Hb and RBC of paediatric patients (7.2 ± 1.6 g/dl and 3.6 ± 0.7×106 µl respectively compared to control group (12.3 ± 1.1 g/ dl and 4.7 ± 0.4 ×106 µl respectively). Total WBC count and neutrophil percent decreased significantly (p-value=0.000). Thrombocytopenia was also observed in patients in both groups (p-value= 0.000). Significant prolongation in PT and APTT of group B patients was observed compared to control subjects; TT was also prolonged but insignificantly. In conclusion, Visceral Leishmaniasis affects children and young adults.
Keywords
Visceral Leishmaniasis, Anemia, Leukopenia, Coagulopathy
Received:June 14, 2016
Accepted: July 1, 2016
Published online: August 5, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
Leishmaniasis with 3 types of disease: visceral, cutaneous, mucocutaneous leishmaniasis [1]. About 20 species are known to cause Leshmaniasis in man [2]. L. donovani parasite persists in the spleen and bone marrow and its expansion in these sites is associated with increase in local hematopoietic changes [3]. Various hematologic manifestations are found in visceral forms. VL may present with splenomegaly, hepatomegaly, and fever. VL is endemic in more than 60 countries worldwide, including Southern Europe, North Africa, and the Middle East. VL is a systemic infection of the reticuloendothelial system caused by protozoa Leishmani donovani of the genus Leishemania. Genus Leishmania was created by Ross in 1903. Sir William Leishman discovered the parasite in spleen smears simultaneously with Charles Donovan identifying the same parasite in spleen biopsy. The parasite has two forms: a flagellate or amasigotes and flagellate or promastigote. As amastigote exists and proliferate in the mononuclear phagocytic system (MPS), specially spleen, liver and marrow, this leads to hyperplasia of the MPS with resultants disturbances in phagocytic bearing organs producing hematological manifestation [1]. Leishamnia spp. is endemic in tropical and sub- tropical regions and human disease mainly occurs in African parts and Asia, Middle East [4]. L. donovani and the main sand fly vector is phlebotomus orientalis whose habitat is Acacia – Balanites woodland and black cotton soil [5].
Al–Gaderf State is as one of endemic with visceral leishmaniasis, which affects individuals at different age, groups particularly children and young adults. Most of patients presented clinics with anemia, leukopenia and thrombocytopenia.
a. Background
VL is a chronic infectious disease that can cause various hematological manifestations. It is characterized by liver and spleen enlargement, endemic in India, characterized by hypergammglobulinemia, anemia, leukopenia, thrombocytopenia. Thrombocytopenia is detected after long duration of illness, splenic sequestration is possible contributing factor. Liver dysfunction with jaundice, ascites and deranged coagulation may occur in late stage. Liver dysfunction may be caused by protozoa itself or indirectly to the effect related to immune response of the parasite. PT and APTT were prolonged in 11% of patients. Hematological abnormalities in VL are common, chronic inflammation and dietary factors appear to be most common factors [1]. Poverty, wars, conflicts and migration have significantly aggravated leishmaniais in East Africa [5]. VL is characterized by fever, hepatosplenomegaly, anemia, neutropenia and hypergammaglobulinemia, most of them remain a symptomatic with the disease self – limiting. The disease is more frequent among rural population and domains. Around 95% of patients under 5 years, male to female ratio 1.3: 1.6. The appearance of the parasite in the human body stimulates humeral immunity system resulting in antibody production. The principal involved organs are reticuoendothelial system, other organs such as kidney, digestive system mucosa may be filled with macrophages. Bacterial infection is one of the major complications leading to death in patients with VL [6].
b. Pathogenicity of Visceral Leishmaniasis:
Visceral leishmaniasis is a protozoan parasite characterized by chronic course, hepatomegaly and anemia to pancytopenia. VL is an infection of reticular-endothelial system. The parasite migrates to the internal organs such as liver, spleen and bone marrow, and if left untreated, will almost always result in the death of the host, it is found throughout parts of the old and new worlds and can infect humans as well as domestic and wild animals. The occurrence of death from VL is associated with several factors including young age and the presence of co- morbidities such as infections, malnutrition. Hemophagocytosis and granulomatous lesion of the bone marrow, chronic inflammation dietary factors appear to be the most important factors affecting hematological status in VL. 19 boys and 11 girls [7].
To establish infection, promastigotes enter macrophages silently to evade triggering host responses. Leshmaniasis promastigotes bind to some of the surface molecules like complement receptor 1and 3 (CR1 AND CR3) of macrophage before they are internalized. Amasigotes replicate by binary fission, rupturing the macrophage and spreading to un –infected cells. Leshmania parasite actively secretes proteases and other factors that affect immune cells and cytokines [6]. Leishmania parasite lives in the phagolysosomes of macrophages in liver, spleen, bone marrow and some lymph nodes. Patients showed marked depressed cellular immune response, as demonstrated by the absence of delayed type hypersensitivity reactions to leishmania antigen. Macrophages are the only cells in vivo allow growth of the intra-cellular pathogen Leishmania, parasites in macrophages cause production of gamma interferon by parasite- specific T- cells. VL is acute and resolved if liver in infected, but it is chronic during spleen infection, so it is characterized by splenomegaly and parasite persistence [8]. L. donoanvi targets bone marrow stromal macrophages in vivo and can infect and multiply in stromal cell lines of macrophage. Infection of stromal macrophages increases their capacity to support myelopoiesis in vitro. VL parasite replicate within Kupper Cells in the liver over the first 28 days of infection and are then cleared by a T-cell dependent granulomatous response. Bone marrow – derived monocytes are also essential for effective clearance of parasites from this organ [3]. Bacterial infection, severe anemia, malnutrition, severe absolute neutropenia, severe thrombocytopenia, and higher neutrophil count, liver injury, kidney failure are the main syndrome of Visceral Leishmaniasis. Bacterial infection and bleeding were mutually exclusive events leading to death [9]. Long incubation period up to 10 years have been occasionally reported. VL is a disease of the mononuclear phagocytic system, commonly affecting spleen, liver, bone marrow and lymph node. Visceral leishmaniasis is a chronic disease evolving slowly over many months or even few years. Spontaneous evolution is fatal in 90% of cases, mainly caused by inter-current infections or hemorrhages [10]. Leishmania spp. do not remain active outside the host or in vitro culture, incubation period of VL = 10 days and become apparent in 2 to 6 months. Appetite loss causes anemia, thrombocytopenia may cause bleeding tendency, leukopenia can result in increased susceptibility to other infections. Post kala-zar dermal Leishmaniasis (PKDL) is a complication of VL occurs after recovery in some cases of VL caused by L. donovani. In Africa PKDL is common usually occurs within 6 months of VL and typically disappears within a year without treatment [4].
c. Incidence of Visceral Leishmaniasis
Leshmania infections are worldwide in distribution; it is endemic in more than 60 countries. WHO estimates the annual global rate for VL prevalence at 2.5 million and incidence at 0.5 million cases and causes 60 – 70 thousands deaths every year (WHO, 2010). VL occurs mainly in Bangladesh, Brazil, Ethiopia, India, Nepal, South Sudan Republic and Sudan. It has been known to exist in Sudan since the beginning of 19th century [11]. Leshmaniasis exists as a disease in 88 countries. Some countries are hit harder than others, these include Bangladesh, India, Nepal, Sudan, Brazil and Syria [12]. VL is present in 47 countries of the world, most of the being developing countries. It is estimated that approximately 400.000 individuals are infected annually worldwide. VL is characterized by anemia and leukopenia. Children are at greater risk than adults of developing VL in endemic areas. According to WHO, Leshmania affects around two million people annually, 500.000 cases of which are of Visceral form. It is estimated that 350 million people are exposed to the risk of infection, with a global prevalence of 12 million infected individuals. VL predominating among five years olds (1-3 ) years, mean age of children was 2.6 years. Children of both sexes were approximately affected [13]. WHO Leshmaniasis Control Team reported that in 2012 endemic leishmaniasis occurred in 98 countries with a reported total of more than 58,000 cases of VL and 220,000 cases of CL, assessing for underreporting, it was thought that approximately 0.2 to 0.4 million VL cases and 0.7 to 1.2 million cases of CL occurred. More than 90% of VL occurred in India, Bangladesh, Sudan, Republic of Southern Sudan, Brazil and Ethiopia [3]. VL affects around 500.000 people every year. Patients have anemia, an enlarged spleen and liver and darkening of the skin. It kills more than 50.000 people worldwide. Among parasitic diseases, only malaria is more deadly. VL is the second largest foci in east Africa, perhaps, as many as 40.000 cases every year and incidence is on the rise [14]. Leishmaniasis is a major public health problem in Bangladesh, North East Asia, Nepal, Sudan and North East Brazil. Leishmaniasis threatens 350 million people in 88 countries. The two Leishmania species responsible for VL are L. donovani and L. infantum. There are estimated 12 million cases worldwide with one and a half to two million cases occurring each year. 90% of VL cases in the world in Bangladesh, India, Sudan and Brazil [10]. In Kenya: Man is the only one reservoir. In Kenya, both CL and VL were endemic, in addition PKDL has also been reported in parts of Kenya from as far as early in the 20th century [5].
In 200-2001, 904 patients were diagnosed with VL, with patients coming from as far as southern Somalia and south east Ethiopia. Leshmaniasis in Ethiopia: VL caused by L. donovani is endemic in the low lands With incidence of 1000-2000 cases annually, 20-40% of the persons infected with HIV. Leishmaniasis in Uganda: socio- economic status and treating livestock with insecticides as risk factors for VL. VL is also reported in Somalia. [5]. In Ethiopia, recent years have seen the disease spread to previously non-endemic districts. In Uganda – which sees a few hundred cases every year. In Somalia, around 1600 patients treated per year, and there has been a tremendous increase in the past 2 years [10]. VL in Iran is a pediatric infection and the main victims of the disease are children under 10 years old [15].
d. Visceral Leishmaniasis in Sudan
Sudan has the highest prevalence rate of post kala-azer dermal leishmaniasis (PKDL)
Skin complications of VL that mainly affects children bellow age ten.
In Sudan, visceral, cutaneous and muco-cutaneous are prevalent. It is one of the five countries in the world constitutes 90% of VL cases and the highest incidence of PKDL
From 1989 to 2002, 51,000 cases of primary VL, relapsed VL, PKDL in Sudan. 43% 43% were cured (cure rate 90.8%) and 3,900 die during treatment (death rate = 8.2%). VL in Sudan: thought the 20th century, VL has been reported in southern Sudan and major outbreaks have followed population movement, flooding, food shortage and conflicts. The worst recorded epidemic probably killed 100,000 people in the Western Upper Nile area of southern Sudan from 1984 to 1994 [5]. In Sudanese VL patients, risk factors for death were identified as, age less than 2 years, malnutrition, anemia, Hb less than 6 g/dl and splenomegaly [15]. In March 2009, Sudanese Government expelled aid agencies from north Sudan. Al Gaderf State in eastern Sudan is the epicentre of VL in east Africa, WHO is dispatching drugs to the areas [14]. VL is a major health problem in Sudan. Patients age from 1 to 51 years [11]. Sudan, an area that includes endemic eastern states, the last few years have seen an increase in incidence in eastern Sudan [14].
According to the data from Khartoum Leishmania Centre, Al- Gadref City showed highest frequency of patients with visceral leishmaniasis (80.7%) compared to other endemic areas during the period from 2006 to 2010. Al – Gadref City is characterized by a long rainy heavy season, which provides suitable habitat to sand fly multiplication. This is confirmed by higher frequency of patients in the last 2 years (2009-2010 showing that the Visceral Leishmaniasis is still a health problem in Sudan.
Table 1. Frequency of Primary Kala-azar in most Endemic Areas in Sudan (2006-2010).
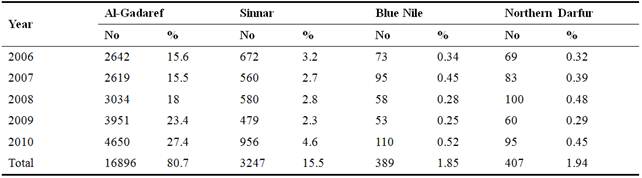
Khartoum Leishmania Center (2011).
●Total number of cases in the 4 endemic areas are = 16896 + 3247 + 389+ 407 = 20939.
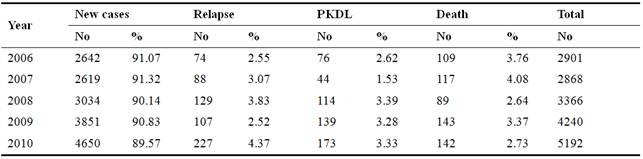
New cases of visceral leishmaniasis in Al –Gadref City constitute 91.07% in 2006 with gradual decrease in 2007 to 2010. This gradual decrease in the number of new cases with Visceral Leishmaniasis could be due to effort of health authorities towards management and control of Leishmania in Eastern Sudan. This is also reflected by decrease in number of deaths from 3.76% in 2006 to 2.73% in 2010.
Table 2. Frequency of Cases with Visceral Leishmaniasis in Al - Gadaref State (2006-2010).
e. Visceral Leishmanaiasis in Al - Gadref State
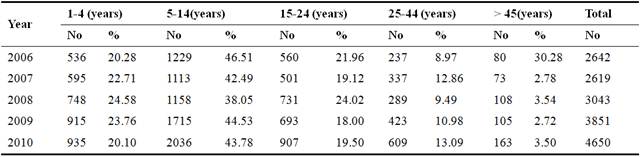
Visceral Leishmaniasis affects individuals at different age group, particularly age group which ranged between 1 to 14 years. The disease and its associated complications will affect the normal growth of patients. The main factor is illiteracy of parents, since most of citizens migrate from neighbouring poor countries where health and educational facilities are lacking. Nutrition could another contributing factor as reported by previous studies.
Table 3. Age frequency of Patients with Visceral Leishmaniasis in Al-Gadref State (2006-2010).
f. Visceral Leishmaniasis among Children:
VL is the most severe form of the disease affecting children. The extend and presentation of the disease depend on several factors, including the humoral and cell- mediated immune response of the host, the virulence of the infecting species and the parasite burden. Children are at greater risk than adults in endemic areas. Malnutrition contributes to the development of the disease, and incomplete therapy of initial disease is a risk factor for recurrence of leishmaniasis. Splenomegaly, hepatomegaly, lymph node enlargement, thrombocytopenia, anemia, leukopenia and hypergammagloulinemia are the most common findings in Paediatric leishmaniasis [16]. VL predominating among five years olds (1-3) years, mean age of children was 2.6 years. Children of both sexes were approximately affected [13]. VL is the most severe form of the disease affecting children. The extend and presentation of the disease depend on several factors, including the humoral and cell- mediated immune response of the host, the virulence of the infecting species and the parasite burden. Children are at greater risk than adults in endemic areas. Malnutrition contributes to the development of the disease, and incomplete therapy of initial disease is a risk factor for recurrence of leishmaniasis. Splenomegaly, hepatomegaly, lymph node enlargement, thrombocytopenia, anemia, leukopenia and hypergammagloulinemia are the most common findings in Pediatric Leishmaniasis [16]. Mean age of the patients was 3.7 years, the majority of the cases (91.5%) were ≤ 5 years, 57.1% were males and 42.9% were females. [15]. Kala-azar usually present in older children and young adults with insidious splenomegaly and pancytopenia [17]. The occurrence of death from VL is associated with several factors including young age and the presence of co- morbidities such as infections, malnutrition [7]. Normochromic normocytic anemia is a frequent feature and clinically significant feature in VL and hemoglobin levels of 7-10 g/dl are commonly found, it is more severe in paediatric patients (mean = 6.4 vs. 7.3 g/dl) as compared to adult patients [1]. VL in Iran is a pediatric infection and the main victims of the disease are children under 10 years old. The presence of severe neutropenia and severe thrombocytopenia were reported as independent predictors of death from VL, and thrombocytopenia had the strongest association with death. In Sudanese VL patients, risk factors for death were identified as, age less than 2 years, malnutrition, anemia, Hb less than 6 g/dl and splenomegaly [15].
g. Hematological abnormalities associated with Visceral Leishmaniasis
Anemia is the most common hematological manifestation of VL, the disease may be associated with leukopenia, thrombocytopenia, hem-phagocytosis and disseminated intravenous coagulation. Anemia is normocytic normochromic is frequent significant feature of VL and Hb level of 7-10g/ dl were commonly found. It is more severe in pediatric patients. The cause of anemia in these patients is multifactorial: 1/ sequestration and destruction of RBCs in enlarged spleen. 2/ immune mechanism and alteration in RBC membrane permeability have been implicated. 3/ hemolysis is the major cause of anemia, with plasma volume expansion associated with massively enlarged spleen. Hematological abnormalities in VL are common. Hypersplenism, homo-phagocytosis, chronic inflammation and dietary factors appear to be most important factors [1]. Patients with VL are predisposed to bleeding. BPL count correlated to intravenous activation markers, depending on severity of disease [18]. Hematological abnormalities in VL are common, chronic inflammation and dietary factors appear to be most common factors. PT and APTT were prolonged in 11% of patients [1]. Before treatment the reduction of BPL count was observed in 95%. Prolonged PT and TT was found in severe form of the disease, TT is prolonged in 45.7%. Soluble monomeric fibrin complexes (SFMC) was increased in 80% (p = 0.003), and D-dimer level in 95.6%, protein C in normal value. The results showed that visceral lesihmaniasis affects primary hemostasis, coagulation and fibrinolysis and these alterations are related to the severity of clinical symptoms [19]. Poverty and expensive treatment are contributing factors. Hemolysis is the major cause of anemia, nutritional factor might be common. Leukopenia has been attributed to hypersplenism. Thrombocytopenia is observed in majority of patients and splenic sequestration is possibly the min contributing factor. Significant increase in in the mean APTT, PT and TT and D-dimer level. Alteration in liver function among VL patients is possibly the main contributing factor. Liver dysfunction may be caused directly by protozoa itself or indirectly to the effect related to the immune response of the parasite [11]. Various hematologic manifestations are found in visceral forms. VL. Anemia is the most common hematological manifestation of VL, associated with leukopenia, thrombocytopenia, pancytopenia and intravascular coagulation [1].
h. Vaccination against visceral leishmaniasis
Visceral L is one of neglected tropical diseases recognized by the World Health Organization. The threat of this debilitating disease continues to unavailability of promising drug therapy of human vaccine. An extensive research is undergoing to develop a promising vaccine to prevent this devastating disease. Vaccines based on recombinant protein and antigen – encoding DNA plasmids have given promising results and few vaccines including leishmune have been licensed for canine visceral leishmaniasis. A Systematic investigation of these vaccine candidates can lead to development of promising vaccine for human visceral leishmaniasis, most probably in the near future [20].
Treatment of leishmaniasis is dependent on chemotherapy. A major problem is that these drugs are associated with problems of cost, toxicity, length and duration of treatment and the development of parasite drug resistance. However, there is still no vaccine for use in humans; this has forced researchers to think about other control measures, and in particular, the development and implementation of a new vaccine. Advances in understanding of Leishmania infection parthenogenesis and the generation of the host – protective immunity, together with completed Leishmania genome sequences, has opened new avenues for vaccine research. This study discuss recent advances in the development of vaccines to prevent leishmaniasis and highlighting a new promising approach that targets the parasite hemoglobin receptor [21].
In India, emergence of resistance against commonly available drugs poses a major threat in the treatment of visceral leishmaniasis. Absence of any licensed against VL emphasizes the urgent need to develop an effective alternative vaccination strategy. Promising findings was reported previously, which showed that heterologous prime-boost vaccination was able to protect mice and hamsters from experimental VL induced by L. donavani isolates. In addition, protection in mice is correlated with strong cellular and humoral immune responses. The same author concluded that, vaccination regime could provide a potent strategy for future anti-leishmanial vaccine development [22].
2. Materials and Methods
a. Study design
The study population included patients with visceral leishmaniasis attended Al- Gaderf Teaching Hospital -2010. The study population was divided into 2 groups:
Group A: Pediatric patients with visceral leishmaniasis, both sex, with age ranged between 1-14 years were selected for determination of Complete Blood Cell Count.
Group B: Patients with visceral leishmaniasis, both sex with different age groups were included for determination of hemostatic profile.
b. Study population:
Group A: 50 pediatric patients with visceral leishmaniasis with age ranged between 1-14 years. 25 apparently healthy subjects with matched age were selected as control.
Inclusion criteria: pediatric patients with visceral leishmaniasis confirmed by bone marrow examination, age ranged between 1-14 years.
Exclusion criteria: visceral leishmaniasis newly diagnosed pediatric patients, or with age above 14 years. Patients with associated diseases that may affect their hematological profile were also excluded.
An In informed consent was obtained from parents of patients and control subjects and sample was collected after their agreement to participate. Clinical data was obtained from hospital records.
c. Blood sample analysis: Complete Blood Cell Count was determined using Sysmex KX-21 N hematological analyser. 2.5 ml of venous blood was collected in EDTA container.
d. Study variables: Hb, RBC, RBC Indices, PCV, WBC and Blood platelets.
Group B. 50 patients newly diagnosed with visceral leishmaniasis, all age groups and both sexes were included. 20 apparently healthy individuals with matched age were selected as control group.
Inclusion criteria: Patients with visceral leishmaniasis under treatment, both sex and with different age were included
Exclusion criteria: Patients newly diagnosed visceral leishmaniasis; patients with associated diseases that may affect hemostatic profile were excluded.
e. Blood sample analysis: 5 ml venous blood was collected from each subject 2.5 venous blood was collected in EDTA anticoagulant container and 2.5 ml in tri –sodium citrate anticoagulant and platelet poor plasma (PPP) was used for determination of PT, TT and APTT manually.
f. Study variables: Hemoglobin, Blood platelets, PT, TT, and APTT.
g. Statistical analysis: SPSS computer program was used for t- independent test, p – value was set at ≤ 0.05 significance level.
3. Results
Group A:
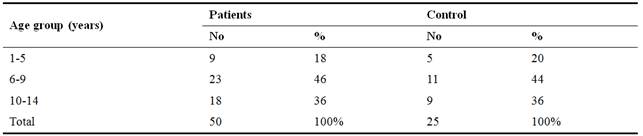
Most frequent age group of patients with visceral leishmaniasis ranged between 6-9 years (46%), followed by age group 10-14 years (36%). This indicates that the disease is more frequent among children bellow above 5 years. Among adult patients, the disease is more frequent among age group from 21 40 years. This showed that visceral leishmaniasis affects young adults who often work as farmers which make them more vulnerable to sand fly bites.
Table 4. Age Frequency of Visceral leishmainsis Pediatric Patients compared to control subjects.
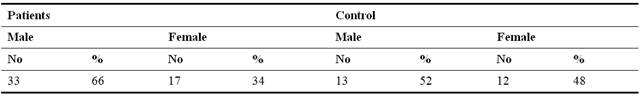
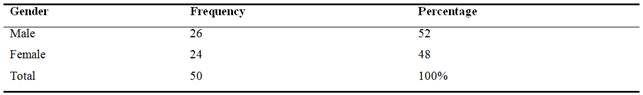
Male visceral leishmaniasis patients were more frequent than females (tables 2 and 7). Male patients constituted 66% and 52% respectively. Males are often works with their parents in the farms which makes them more subjected to insect bites compared to females.
Table 5. Gender Distribution of Visceral leishmaniasis Pediatric Patients compared to control group.
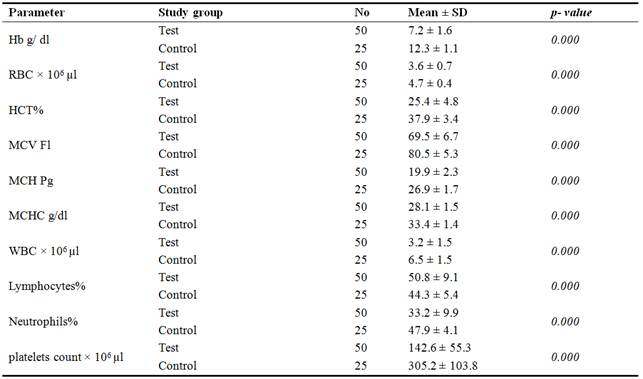
All hematological parameters of patients under study were significantly different compared to control subjects. Although all patients under treatment, Hb, RBC count and RCB indices significantly decreased compared to control subjects, this reflected the severity of the disease among children and young adults. WBC and neutrophils decreased significantly compared to control group, but lymphocytes increased significantly, indicated infection which is often associated with visceral leishmaniasis. Thrombocytopenia was also observed among pediatric patients which indicating bleeding tendency as one of visceral Leishmaniasis complications as reported by many previous investigators.
Table 6. Hematological Profile of Visceral Leshmaniasis Pediatric Patients compared to control group.
Group B
Table 7. Age frequency of Patients with Visceral Leishmaniasis.
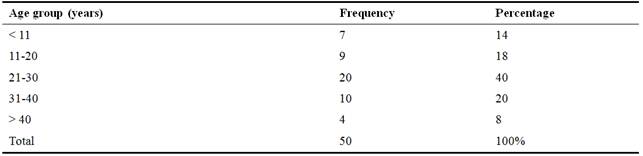
Table 8. Gender frequency of patients with Visceral Leishmaniasis.
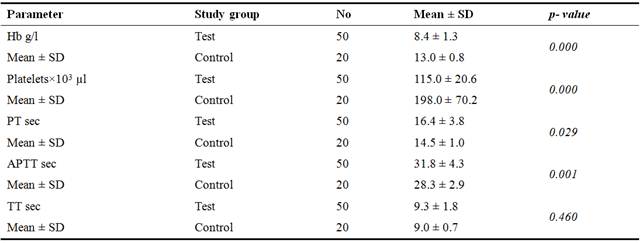
Hb and platelets of Group B patients significantly decreased significantly compared to control subjects. Coagulation profile of Group B patients was also altered. PT and APTT were prolonged significantly compared to control group. TT was prolonged but insignificantly. The man cause of hemostatic alteration is related to liver dysfunction caused Visceral leishmaniasis as previously reported by many researchers.
Table 9. Hemoglobin, Blood platelets, PT, APTT and TT of Visceral Leishmaniasis Patients compared to control group.
4. Discussion
Visceral leishmaniasis affects individuals at different age groups and both sexes were infected (tables 4, 5, 7, 8). Among children, most affected age bellow 10 years. Similar to a study in Yemen which revealed that VL predominating among five years olds mainly (1-3) years [13]. Another study in Iraq [8] showed that both gender were equally infected with mean age ranged between 7 months and 12 years. A study in Iran showed that 91.5% of VL cases were ≤ 5 years, 57.1% of them were females and 42.9% were males [15]. The same author concluded that children under 10 years old are the main victims of VL, as in Sudan where the risk factor for death were identified among pediatric VL with age less than 2 years. Among adult patients, the most affected age ranged between 21 and 30 years (table 7).
Significant hematological changes was observed among Visceral Leishmaniasis pediatric patients (tables 6 and 9). Similar findings were reported by some investigators and concluded that Visceral Leishmaniasis is associated with hematological abnormalities [1,23] and pancytopenia [13,17]. Hematological abnormalities in VL are common, chronic inflammation and dietary factors appear to be most common factors [1]. A study in Yemen revealed that panocytopenia and hepatosplenomagaly are the most common clinical manifestation in Yemen children. The reason for higher frequency of pancytopenia is probably the longer duration of symptoms and splenomegaly before presentation to the hospital and increased peripheral destruction rather than bone marrow failure [13].
Laboratory findings of VL patients in the current study revealed significant decrease in Hb, RBC and RBC indices of visceral leishmaniasis pediatric patients compared to control group (table 6), indicating that anemia is a common among patients with Visceral Leishmaniasis. Similar results were reported by many authors [1,13,15,24,25]. Multiple factors could be leading causes of anemia among patients with Visceral Leishmaniasis of these factors: sequestration and destruction of RBCs in enlarged spleen, immune mechanism and alteration in RBC membrane permeability hemolysis is also a major cause of anemia, with plasma volume expansion associated with massively enlarged spleen, reduced plasma iron level in the presence of greatly increased iron stores suggests that the reticuloendothelial hyperplasia is accompanied by abnormal iron retention by macrophages, typical anemia of chronic disease [1]. This may limit the marrow response to hemolysis. Hypersplenism, nutritional deficiencies of iron, folate and vitamin B12 may play further contributory role [1,24].
Malaria infection could further complicated the situation and may co-exists in the same patients [26], since Al –Gaderf State is characterized by heavy rains which provides suitable habitat to both sand fly and mosquito vectors activities.
Various studies in different countries concluded that malnutrition is a main contributing factor associated with VL, in Athens [16], Iran [7], in Iraq, out of 132 children, 65.1% were malnourished [27], Yemen [13], Bangladesh [28] and Sudan [11, 15], or due to iron, folate and vitamin B12 deficiencies [1, 23]. In Brazil endemic areas moderate to severe malnutrition was related to a 13.2% mortality rate compared to 7.0% in well-nourished children. In Southern Sudan (The New South Republic) epidemic Visceral Leishmaniasis areas, the approximate relative risk factor for death was 12.2 for those with body mass index less than 12.2 kg/m2 [25].
TWBC count and neutrophil % of VL patients significantly decreased while percentage of lymphocytes significantly increased compared to control (p = 0.000), (table 6). Many studies showed similar results and concluded that leukopenia and neutropenia was common among pediatric patients [1, 8, 23, 29]. Bacterial infection is one of main causes which are frequently a cause of death due to massive bleeding or severe anemia as reported by previous investigators [9,25]. Splenomegaly associated with Visceral Leishmaniasis is another contributing factor [15,17] or due to hypersplenism [11,24]. Bone marrow failure is an additional contributing factor [8,25], as the parasite infects macrophage in the spleen, liver and bone marrow [11]. In addition, suppression of immune system was expected in patients with VL as previously reported [8], since the parasite actively secretes proteases and other factors that affects immune cells and cytokines [6]. Furthermore, humoral and cell- mediated immune response of the host depends on severity of VL and parasite burden [16].
Thrombocytopenia was observed among all visceral Leishmaniasis patients (table 6 and 9). Many studies confirmed these findings [7,13,23,24]. Patients with VL are predisposed to bleeding and BPL count was correlated to intravenous activation markers, depending on severity of disease [18], peripheral BPL destruction [24] or due to poor platelet formation [13]. Splenic sequestration is possibly the main contributing factor and liver dysfunction with jaundice, caused directly by protozoa parasite itself or indirectly to the effect related to immune response of the parasites [1].
According to table (9), PT and APTT of Visceral Leishmaniasis patients were significantly prolonged compared to healthy control subjects. These finding were confirmed by previous studies [1,9,11]. Accordingly, bleeding tendency among patients with VL in the current study was identified. This may be due to liver dysfunction, coagulopathy and exhaustion of plasma proteins. Previous authors concluded that bleeding is one of the main causes of death of patients with Visceral Leishmaniasis [2,9,10,25,30]. The main causes of bleeding tendency; are liver dysfunction and jaundice [30], or due to hypersplenism [1]. Severity of the disease is another contributing factor since Visceral Leishmaniasis affects primary hemostasis, coagulation and fibrinolysis [19].
5. General Comments
Al Gaderf State is characterized by heavy rainy season which provides suitable habitat for both sand fly and mosquito activities, which makes citizen vulnerable to malaria and Visceral Leishmaniasis infections. Most of patients are citizens who migrate from surrounding countries and rural areas where medical centres are limited and patients presented these centres at latest stage of illness.
6. Conclusion
VL was common in Al- Gadref State. The disease affects individuals at different age groups, but it is more frequent among children bellow 10 years and adults at age ranged between 21 and 30 years. Males and females are affected.
Hematological profile of Visceral Leishmaniasis patients was significantly different compared to control group. Anemia, leukopenia and thrombocytopenia were common features associated with VL among children. Bleeding tendency was observed among adult patients.
Recommendations
Vector control may be on of effect control measures for eradication of Leishmaniasis in endemic areas in Sudan. Well-equipped medical centres should be established in endemic Sudanese States and in rural areas in particular. Health authorities should encourage vaccination research - which is currently undergoing. This will open new avenues for development and implementation of an effective vaccination against VL in Sudan
References
- Neelam Varma and Shano Naseem. Hematological Changes in Visceral Leishmaniasis/Kala Azar. Indian Journal of Hematology and Blood Tranfusion 2010, 26 (3):78-82.
- Piet A. Kager. Leishmania species (Leishmaniasis). Leishmaniasis- Infectious Disease andAntimicrobial Agents. Am J Trop Med Hy 2014;91: 901-4.
- Sara E. J. Cotterell, Christian R. Engwerda and Paul M. Kaye. Leishmaniasis donovaniInfection of bone marrow stromal macrophages selectively enhances myelopoiesis, by amechanism involving GM-CSF and TNF- α. Blood 2000; 95 (5):1642-1651.
- Centre of Food Security and Public Health- Iowa State University. Institute for InternationalCooperation in Animal Biologics 2009: 1-11.
- P Ngure, A Kimutai, W Tonui, Z Nganga. A Review of Leishmaniasis in Eastern Africa.Original Article. The internet Journal of Parasitic Diseases. 2008; 4 (1).
- Abdolvahab Alborzi, Gholam Reza Pouladfar, Mohammed Hassan Aelami. VisceralLeishmaniasis; literature review and Iranian experience. Iranian Journal of ClinicalInfectious Diseases2007; 2(2):99-108.
- Ali Fattahi Bafghi, Seyed Hossein Shahceraghi, Sedigheh Nematollahi. Comparison ofHematological Aspects: Visceral Leishmaniasis and Healthy Children. TropicalParasitology2015, 5(2):133-135.
- Mohamed Maroof Middib, Fadil Abass Al- Mouktar. Hematological Changes including theImmune system in Patients with Visceral Leshmaniasis at Al-Muthanna Governorate;Journal of Babylon University/ Pure and Applied Sciences/No. (4)/ 22:2014.
- Carlos Henrique Nery Costa, Guilnerme Loureiro Werneck, Drcas Lamounier et al. IsSevere Visceral Leishamniasis a systemic Response Syndrome? A case Control Study. Soc.Bras. Med. Trop2010.43 (4).
- Sameer Gulati, HP Paljor, Sanjay Panadit, et al.. Kala Azar without Splenomegaly. Annalsof Tropical Medicine and Public Health2009; 2 (2): 57-60.
- Omaima Abd ELsied A. and Mahdi H. A. Abdalla. Visceral Leishmaniasis:Hematological and Hemostatic Changes among Sudanese Patients. International Journalof Current Research2014; 6 (12): 11037-11039.
- Carson-Dewitti, Rosaly; Odle, Tersa.Leishmaniasis. Gale Encyclopedia of Medicine, 3rded. 2006. http://www.encyclopedia.com 2015.
- Gamal Abdul Hamid, Ghada A. Gobah. Clinical and Hematological Manifestation ofVisceral Leishmaniasis in Yemen Children. Turk J Hematol 2009; 26: 25-8.
- Talh Burki. East African Countries Struggle with Visceral Leishmaniasis; World Report.The Lancet2009; 374(9687):371-372.
- Bahdor Sarkari, Tahereh Naraki, Mohammad Amin Ghatee et al. Visceral LeishmaniasisIn Southern western Iran: A Retrospective Clinico-Hematological Analysis of 380Consecutive Hospitalized Cases (1999-2014). PlOS ONE Neg Trop Dis 2016; 11(3).
- Kafetzis D A. An Overview of Pediatric Leishamniasis. PubMed SYMPOSIUM 2003;49(1):31-8.
- Ruma Pahwa, Sanjeer Kumar Gupta, Tejinder Singh et. al. Acute Fulminant VisceralLeishmaniasis in Children – A report of Two Cases. Indian Journal of Pathology andMicrobiology2004; 47(3):428-430.
- Lomtaze ML, Khochava MA, Shalamberidze IA et al. Study of Intravenous CoagulationActivation markers in Patients with Visceral Leishmaniasis. Georgian Med News 2005;(124-125):47-50.
- Lomtadze ML, Khochava MA, Shalamberidze IA et al. Functional Status of HemostasisSystem in Patients with Visceral Leishmaniasis PubMed Georgian Med News2005;(128):59-62.
- Guha R, Das S, Ghosh J, Naskar K et al. Heterologus priming-boosting with DNA andVaccinia virus expressing kinetoplastid membrane protein – 11 Induces potent cellularImmune response and confers protection against infection with antimony resistant andsensitive strains of Leishmania donovani. PubMed Vaccine 2013;31(15):1905-15.
- Rajiv Kumar and Christian Engwerda. Vaccines to prevent Leishmaniasis. Clinical andTranslation Immunology2014; 3.
- Jain K and Jain NK. Vaccines for Visceral Leishmaniasis: A review J Immunol Methods2015; 422:1-12.
- Muhammad O. Al- Muhammadi, Gafil S. Hassan Al- Shujiri and Mudar H. Noor.Hematological changes in children suffering from Visceral Leishmaniasis (Kalaz-azar).Medical Journal of Babylon2004; 1(3 and 4) pp: 325.
- Muhammad O. Al- Muhammadi, Gafil S. Hassan Al- Shujiri and Mudar H. Noor.Hematological changes in children suffering from Visceral Leishmaniasis (Kalaz- azar).Medical Journal of Babylon1:4, 2014: doi: 1812-156X1-4.
- Zainab H., Meaad K. Hassan and Abdul Mohsin H. Jassim. Outcome of HospitalizedChildren with Visceral Leishmaniasis in Basrah, Southern Iraq. The Medical Journal ofBasrah University2008; 26(2): 121-126.
- Erika van den Bogaart, Al- Badawi A Talha, Masja Straetemans et al. Cytokine ProfileAmongst Sudanese Patients with Visceral Leishmaniasis and Malaria co-infection.BMCImmunology2014; 14 (16): doi: 10.1186/ 1471-2172-15-16.
- Zeinab Hameed Gani, Meaad Kadhum Hassan- Abdul- Mohsin Hameed Jassim.Infectious Complications of Visceral Leishmaniasis in Basrah Iraq. Kerbala Journal ofMedicine2011; 4 (1):972-979.
- H A M N Ahasan, FCPS, M A J Chowdhury, FCPS, et al. Deaths in VisceralLeshimanaisis (Kala-azar) During Treatment. Original article Med J Malaysia1996; 51(1):29-32.
- Agrawal Y., AK Sinha, P Upadhyaya et al. Hematological Profile in VisceralLeishmaniasis. International Journal of Infection and Microbiology 2013; 2(2):39-44.
- Elfakey Walyeldin, Ahmed Muawia Abdurrahman and Suwar M. Children with VisceralLeishmaniasis Presented to Omdurman Emergency Hospital for Children. SudaneseJournal of Paediatrics and Child Health2010; 10:46-50.



