Frequency of Surgery in Patients with Ectopic Pregnancy After Treatment with Methotrexate
Shohreh Malek Khosravi, Farid Arman, Hania Shakeri*
Gynecology Department Imam Reza Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran
Abstract
Background: Ectopic pregnancy is one of the major life threatening conditions during the first trimester of pregnancy. EP increases the risk of maternal mortality and morbidity. The prevalence of Ectopic Pregnancy is about 2% in the developed world. Objective: This observational descriptive cross-sectional study was performed to determine the frequency of surgery in 70 patients who were diagnosed with Ectopic Pregnancy in their first trimester after failed treatment with single or multiple dose of methotrexate (MTX). Materials and methods: In this observational descriptive cross-sectional survey, 70 patients with Ectopic Pregnancy referring to Imam Reza Hospital (affiliated to Kermanshah university of Medical sciences) between years 2008-2010 who received single or multiple dose of methotrexate as primary management were evaluated. Results: The results demonstrated that surgery was required in 16 patients (22.9%). The contraceptive method was effective in determining the probability of requiring surgery after treatment with Methotrexate among these patients (P=0.035) and the most common methods were IUD (100%) and TL (35.7%). Conclusions: Totally, according to the obtained findings, it may be concluded that need to surgery in patients with Ectopic Pregnancy is a multifactorial entity.
Keywords
Ectopic Pregnancy, Methotrexate, MTX
Received:May 12, 2015
Accepted: May 28, 2015
Published online: June 26, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Ectopic pregnancy is one of the major life -threatening complications and leading cause of death due to pregnancy in developed countries (1&2). EP presents with the blastocyst attaching outside of the uterine cavity (3&4). It’s a major health problem for women of childbearing age. Ampullary region of the Fallopian tube is the most common site for Ectopic Pregnancy (5). The rest of the cases are implanted at different locations such as isthmus, ovaries, abdomen, and broad ligament which account for less than 1% of cases (6&7). Since 1970 the frequency of Ectopic Pregnancy has increased, and it now occurs in 2% of all pregnancies (8). Several important factors are thought to contribute to increasing rates of Ectopic Pregnancy such as increasing the use of ovulation induction and assisted reproductive technologies (ART). Previous tubal surgery, history of smoking, failure with contraception are another important risk factors for developing ectopic pregnancy (10). Patients present to the office or ER with lower abdominal pain or vaginal bleeding and lack of menstrual cycle (3). The methods currently used to detect ectopic pregnancy include trans-vaginal ultrasound and serial serum human chorionic gonadotropin (βhCG) levels (11). To detect a β hCG level equal or more than 1500IU/L and an empty uterus in trans-vaginal ultrasound is highly suspicious of Ectopic pregnancy (12&13). Ectopic pregnancy has significant adverse effects on future pregnancies outcome specially if surgery modality is performed to treat it (14).
Methotrexate (MTX) is a folic acid antagonist and cell cycle-specific antimetabolite (15). MTX is an important, beneficial drug on the medical aspect of treatment, although side effects should be monitored closely. Potassium chloride or Etoposide are the other options available for treatment of ectopic pregnancy (16). Hence diagnosis and treatment of Ectopic pregnancy is a crucial matter (13). Treatment modalities according to patients’ sign and symptom depend on factors such as maternal status, βhCG level, Ultrasound findings and desire to save fertility (10&17). The most common treatment for ectopic pregnancy is conservative surgical management with preservation of the fallopian tube (18&19&20). In some cases, if Ectopic pregnancy is diagnosed early in intact gestational sac and the patient is hemodynamically stable, treatment with local or systemic administration of methotrexate is possible (21). Nearly 25–30% of EP patients are eligible to receive Methotrexate, and rate of successful treatment has been reported to be 78–96%in various studies. (22&23&24&25&26).
Treatment with (MTX) in hemodynamically stable EP, have depicted to be appropriate replacement of surgery (27&28&29). This study was designed to determine the frequency of surgery in patients with Ectopic Pregnancy after Methotrexate use. Its a new study. There isn't any report from the rate of patients with Ectopic Pregnancy who undergone surgery.
2. Methods and Materials
It was an observational descriptive cross-sectional study among 70 consecutive women with diagnosis of Ectopic Pregnancy was organized in a main teaching and general hospitals that characterize highly qualified centers for diagnosis and treatment of Ectopic Pregnancy pregnancy in Iran,which are reviewed in the duration between 2008 to 2010. Inclusion criteria for this study were patients who developed to Ectopic Pregnancy that was confirmed by βhCG level and trans vaginal ultrasound who received single or multiple dose regimen of Methotrexate as medical treatment of Ectopic Pregnancy. Exclusion criteria for this study were Patients with ectopic pregnancy who received surgical treatment as the first approach of treatment. Required data were collected by a checklist from medical records .and following data were collected: age, gravid ,parity, gestational age, contraception method, side of ectopic pregnancy ,need to surgery, βhCG level, mass size, Methotrexate doses .of total 120 patients were selected, In this study Fifty patients were excluded from the study because their primary treatment was surgery.
Study was approved by ethical committee of Kermanshah University of Medical Sciences and the Helsinki Declaration was respected.
The initial data from 70 consecutive women with Ectopic Pregnancy diagnosis were applied into the computer document file. All statistical analysis were performed using (Statistical package for social sciences) SPSS software version 16 (SPSS, Inc., Chicago, IL, USA). Categorical variables are expressed with prevalence and continuous variables are described with mean ± standard deviation. Comparison of means was performed using One-way Analysis of Variances (ANOVA) and the comparison of categorical values between groups was done by Chi-square test. P-value <0.05 was considered significant (30).
3. Results
Totally, we evaluated 70 pregnant women who develop to EP, mean age was 29.79 ± 6.7, The mean gravid was 2.31 ± 1.26 times and the mean parity was 1.17 ± 1.23 times. The mean gestational age was 5.36 ± 1.24 weeks. OCP was the most common contraceptive method in ectopic pregnancy (35.7%). (Table1)
Table 1. Contraception Methods in EP patients.
| Contraception Method | Surgical treatment | Non-Surgical treatment | Total |
| Natural | 4(16.7%) | 20(83.3%) | 24 |
| IUD | 2(100%) | 0 | 2 |
| Condom | 0 | 5(100%) | 5 |
| OCP | 5(20%) | 20(80%) | 25 |
| TL | 5(35.7%) | 9(64.3%) | 14 |
| Total | 16(22.9%) | 54(77.1%) | 70 |
Right side was involved in 44.3% and the left side was involved in 55.7%. The surgery was required in 22.9%. of Ectopic Pregnancy patients .The mean Beta HCG was 458.36 ± 232.57 mu/ml. The mean mass size was 27.36 ± 9.2 mm. The mean methotrexate dose was 68.64 ± 10.99 mg.
There was a significant differences between contraception method and subsequent need to surgery (P=0.035). The surgery was more common in patients who have used IUD (100%) and TL (35.7%) as contraception method. Age, gravid, parity, Methotrexate dose, involvement side, had no effect on need to surgery (P > 0.05).
The mean gestational age was significantly (P < 0.0001) higher in those needing to surgery (6.5 versus 5.02 weeks). The mean beta HCG was significantly (P=0.001) higher in those need to surgery (648.19 versus 402.11 mu/ml). The mean mass size was significantly (P=0.001) higher in those needing to surgery (33.66 versus 25.5 mm).
4. Discussion
Management of Ectopic Pregnancy is one of the major clinical challenging and one of the most important cause of medical emergency during pregnancy worldwide. The diagnosis of Ectopic Pregnancy performed by trans-vaginal ultrasound and serial serum βhCG level (31). Identification of best method of treatment is very useful .This study was performed to determine the frequency of surgery treatment in patients with Ectopic Pregnancy after single dose or multiple dose Methotrexate regimen use. Our study showed that surgery was required in 16 patients (22.9%) that the contraceptive method, gestational age, mass size, and, initial βhCG level were higher in those requiring surgery. Methotrexate (single or multiple dose regimen) was first line treatment method as a successful option for Ectopic Pregnancy in the 1980's by Tanaka et al (2&26). In a study by Fatih Karaaslan showed Methotrexate is partially effective alternative to surgery in patients with hemodynamically stable patients tubal pregnancies, but suggest that it be used with caution in view of septic events (43). Successful rate for treatment with MTX in Ectopic Pregnancies after daily follow-up evaluation βhCG level are lower than prior document (44). Similar to our study results Potter M. B.et al treatment by Methotrexate has 76.2% successful rate (32).Another similar study Feras Sendy showed using of medical treatment of Ectopic Pregnancy results in 71% success (13). In contrast with our study Ayaz showed that the successful rate with Methotrexate was 3.8 % (33). Odejinmi et al reported that there was a progressive rise in the proportion of Ectopic Pregnancies managed by operative laparoscopy approving our results with a 1:6 ratio for need to surgery in women with Ectopic Pregnancy (34). In the study by NG et al it was seen that fifty-two cases were managed by laparoscopy, and one was converted to laparotomy. Nine patients received Methotrexate injection after surgery because of persistently high serum βhCG level (35).
Agdi et al demonstrated that similar to the case with tubal ectopic pregnancy in general, women with non-tubal Ectopic Pregnancy such as cervical, interstitial, or cesarean scar pregnancy should be first treated medically with Methotrexate (36). In this study need to surgery was increased by contraception by OCP and IUD (Figure 1). Similar to our study some meta-analyses showed IUD and OCP and women sterilize could increase the risk of develop EP to contraceptive failure (37&38). Although in our study there didn't same result about OCP. Ghosh et al reported that the use of levonorgestrel as emergency contraception is a safe and effective measure to prevent unwanted pregnancy (39). In a study showed there isn't any relationship between LNG-EC with the risk of EP compared with case group without contraception but , current use of LNG-EC decreased the risk for normal intrauterine pregnancy but did not increase the risk for EP (42). Pereira et al showed that emergency contraceptive methods are more possible to increase the rate of Ectopic Pregnancy but we found no similar results (40). The more prominent role of barrier methods was seen in Brenner et al study as well as findings in our study (41)
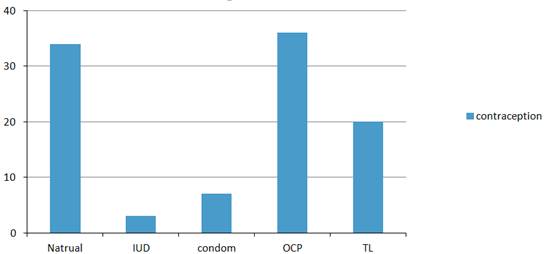
Figure 1. Contraception.
5. Conclusion
Totally, according to the obtained findings and comparison with other similar studies, It may be concluded that the surgery was required in 22.9%, and need to surgery in patients with ectopic pregnancy is a multifactorial entity. The contraceptive method was effective on need to surgery (P=0.035) (Table 1), and the surgery was more common in IUD (100%) and TL (35.7%) users. Level of BHCG was not associated with need to surgery after treatment with single dose or multiple doses with Methotrexate. Age, gravid, parity, gestational age, side of Ectopic Pregnancy, need to surgery, mass size, methotrexate dose were also not determinant factor. However further studies should be performed to obtain more definite results
References
- Maliheh Arab, 1,* Seyyedeh Neda Kazemi, 1 Zahra Vahedpoorfard, Adeleh Ashoori. A Rare Case of Bilateral Ectopic Pregnancy and Differential Diagnosis of Gestational Trophoblastic Disease J Reprod Infertil. 2015 Jan-Mar; 16 (1): 49–52.
- Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet (2006) 367(9516): 1066–7410
- Walker J. J. Ectopic pregnancy. Clinical Obstetrics and Gynecology. 2007; 50 (1): 89–99
- Varma R., Gupta J. Tubal ectopic pregnancy. Clinical Evidence. 2009
- Shaw JL, Diamandis EP, Horne AW, Barnhart K, Bourne T, Messinis IE. Ectopic pregnancy. Clin Chem. 2012; 58: 1278–85.
- Wong J. A., Clark J. F. Correlation of symptoms with age and location of gestation in tubal pregnancy. Journal of the National Medical Association. 1968; 60 (3): 221–223.
- Kellogg A. Intratubalmethotrextate versus laproscopicsalpingotomy. World Journal of Laparoscopic Surgery. 2009; 2(2): 18–20
- Oron G, Tulandi T. A pragmatic and evidence-based management of ectopic pregnancy. J Minim Invasive Gynecol. 2013; 20(4): 446–54
- Bassem Refaat,corresponding author Elizabeth Dalton, and William L Ledger.Ectopic pregnancy secondary to in vitro fertilisation-embryo transfer: pathogenic mechanisms and management strategies
- Sivalingam V., Duncan W., Kirk E., Shephard L., Horne A. Diagnosis and management of ectopic pregnancy. Journal of Family Planning and Reproductive Health Care. 2011; 37: 231–240
- Barnhart KT, Katz I, Hummel A, Gracia CR. Presumed diagnosis of ectopic pregnancy. Obstet Gynecol. 2002; 100: 505–510.
- Lozeau A.-M., Potter B. Diagnosis and management of ectopic pregnancy. American Family Physician. 2005; 72 (9)
- Feras Sendy, Eman AlShehri, Amani AlAjmi, Elham Bamanie, Surekha Appani, and Taghreed Shams
- J Bouyer, N Job-Spira, PJ Pouly, J Coste, E Germain, H Fernandez. Fertility following radical, conservative-surgical or medical treatment for tubal pregnancy: a population-based study. BJOG. 2000; 107(6): 714–21 Failure Rate of Single Dose Methotrexate in Managment of Ectopic Pregnancy. Obstet Gynecol Int. 2015; 902426
- Huffman DH, Wan SH, Azarnoff DL, Hogstraten B. Pharmacokinetics of methotrexate. Clin Pharmacol Ther. 1973;14:572–579.
- Chen CL, Wang PH, Chiu LM, Yang ML, Hung JH.. Successful conservative treatment for advanced interstitial pregnancy. A case report. J Reprod Med (2002) 47(5): 424–6
- Panayotis Xiromeritis, Chrysoula Margioula-Siarkou, * Entity Dimosthenis Miliaras, and Ioannis Kalogiannidis Laparoscopic Excision of Coexisting Left Tubal and Right Pseudotubal Pregnancy after Conservative Management of Previous Ectopic Pregnancy with Methotrexate: An Unusual Clinical
- Gaddagi Rashmi A, Chandrashekhar AP. A clinical study of ectopic pregnancy. Journal of Clinical and Diagnostic Research. 2012; 6 (5): 867–69.
- CJ Sultana, K Easley, RL Collins. Outcome of laparoscopic vs traditional surgeries for ectopic pregnancies. Fertil Steril. 1992; 57: 285
- A Delacruz, DC Cumming. The factors which determine the fertility after a conservative or radical surgical treatment for ectopic pregnancy. Fertil Steril. 1997 Nov; 68(5): 871-4.
- Zalel Y, Caspi B, Insler V. Expectant management of interstitial pregnancy. Ultrasound Obstet Gynecol (1994) 4(3): 238
- Skubisz M., Dutton P., Duncan W. C., Horne A. W., Tong S. Using a decline in serum hCG between days 0–4 to predict ectopic pregnancy treatment success after single-dose methotrexate: a retrospective cohort study. BMC Pregnancy and Childbirth. 2013; 13, article 30 doi: 10.1186/1471-2393-13-30.
- Practice Committee of American Society for Reproductive Medicine. Medical treatment of ectopic pregnancy. Fertility and Sterility. 2008; 90 (5, supplement): S206–S212.
- Barnhart K. T., Gosman G., Ashby R., Sammel M. The medical management of ectopic pregnancy: a meta-analysis comparing ‘single dose’ and ‘multidose’ regimens. Obstetrics and Gynecology. 2003; 101(4): 778–784
- Farquhar C. M. Ectopic pregnancy. The Lancet. 2005; 366 (9485): 583–591.
- Morlock R. J., Lafata J. E., Eisenstein D. Cost-effectiveness of single-dose methotrexate compared with laparoscopic treatment of ectopic pregnancy. Obstetrics and Gynecology. 2000; 95(3): 407–412.
- Hajenius P. J., Engelsbel S., Mol B. W. J., et al. Randomised trial of systemic methotrexate versus laparoscopic salpingostomy in tubal pregnancy. The Lancet. 1997; 350(9080): 774–779.
- Ory S. J., Villanueva A. L., Sand P. K., Tamura R. K. Conservative treatment of ectopic pregnancy with methotrexate. The American Journal of Obstetrics and Gynecology. 1986; 154(6): 1299–1306.
- Stovall T. G., Ling F. W. Single-dose methotrexate: an expanded clinical trial. The American Journal of Obstetrics and Gynecology. 1993; 168(6): 1759–1765
- Bimbo Ayoola Ashaolu, Mopelola Christianah Asaleye, Adebayo Victor Adetiloye, and Isaac Olusegun Alatise. Spectrum of Diseases and Diagnostic Values of Ultrasound in Adult Patients with Nontraumatic Acute Abdomen in a Nigerian Tertiary Health Facility Niger J Surg. 2015 Jan-Jun; 21(1): 6–12.
- Chen-Yu Chen, Yuh-Ming Hwu,Chie-Pein Chen and Chia-Chen Chang Quantitative analysis of total β-subunit of human chorionic gonadotropin concentration in urine by immunomagnetic reduction to assist in the diagnosis of ectopic pregnancy.Int J Nanomedicine. 2015; 10: 2475–2483.
- Potter M. B., Lepine L. A., Jamieson D. J. Predictors of success with methotrexate treatment of tubal ectopic pregnancy at Grady Memorial Hospital. The American Journal of Obstetrics and Gynecology. 2003; 188 (5): 1192–1194
- Ayaz A., Emam S., Farooq M. U. Clinical course of ectopic pregnancy: a single-center experience. Journal of Human Reproductive Sciences. 2013; 6 (1): 70–73
- Odejinmi FO, Rizzuto MI, Macrae RE, Thakur V. Changing trends in the laparoscopic management of ectopic pregnancy in a London district general hospital: 7-years experience.J Obstet Gynaecol. 2008 Aug; 28 (6): 614-7
- Ng S1, Hamontri S, Chua I, Chern B, Siow A.Laparoscopic management of 53 cases of cornual ectopic pregnancy. Fertil Steril. 2009 Aug; 92 (2): 448-52.
- Agdi M, Tulandi T.Surgical treatment of ectopic pregnancy Best Pract Res Clin Obstet Gynaecol. 2009 Aug; 23 (4): 519-27
- Mol B. W., Ankum W. M., Bossuyt P. M. & Van der Veen F. Contraception and the risk of ectopic pregnancy: a meta-analysis. Contraception 52, 337 (1995)
- Xiong X., Buekens P. & Wollast E. IUD use and the risk of ectopic pregnancy: a meta-analysis of case-control studies. Contraception 52, 23 (1995)
- Ghosh B1, Dadhwal V, Deka D, Ramesan CK, Mittal S..Ectopic pregnancy following levonorgestrel emergency contraception: a case report. Contraception. 2009 Feb; 79 (2): 155-7.
- Pereira PP, Cabar FR, Raiza LC, Roncaglia MT, Zugaib M. Emergency contraception and ectopic pregnancy: report of 2 cases. Clinics (Sao Paulo). 2005 Dec; 60(6): 497-500
- Brenner PF. Obstetrics and Gynecology—Epitomes of Progress, ectopic pregnancy: current etiology ,West J Med. 1980 Mar; 132 (3): 230
- Association between levonorgestrel emergency contraception and the risk of ectopic pregnancy: a multicenter case-control study Jian Zhang, 1,* Cheng Li, 1,* Wei-Hong Zhao, 1 Xiaowei Xi, 2 Shu-Jun Cao,3 Hua Ping, 4 Guo-Juan Qin, 5 Linan Cheng, 6 and He-Feng Huanga, 7
- Fatih Karaaslan, Musa Uğur Mermerkaya, Emre Yurdakul, Özlem TanınInt. Bilateral septic knee arthritis after treatment of an ectopic pregnancy with methotrexate Med Case Rep J. 2015; 8: 33–35.
- Am J Obstet Gynecol. 2014 Aug; 211 (2): 128.e1-5. doi: 10.1016/j.ajog.2014.03.043. Epub 2014 Mar 19. Methotrexate success rates in progressing ectopic pregnancies: a reappraisal. Cohen A1, Zakar L1, Gil Y1, Amer-Alshiek J1, Bibi G1, Almog B1, Levin I2.



