Impact of Aquatic Exercise Program on Muscle Tone in Spastic Hemiplegic Children with Cerebral Palsy
Khaled A. Olama1, Hala I. Kassem1, Shimaa N. Aboelazm2, *
1Department of Physical Therapy for Disturbance of Growth and Development in Children and its Surgery, College of Physical Therapy, Misr University for Science and Technology, Giza, Egypt
2Basic Sciences Department, College of Physical Therapy, Misr University for Science and Technology, Giza, Egypt
Abstract
Cerebral palsy is one of the most common causes of serious physical disability in childhood. Exercise for children with cerebral palsy is gaining more popularity among pediatric physical therapists community as an interventional choice. Under water exercise appeals children with cerebral palsy because of the unique quality of buoyancy of water that influences poor balance and poor postural control. The purpose of this study was to investigate the effect of aquatic exercise program on muscle tone in spastic hemiplegic children. Thirty spastic hemiplegic children with cerebral palsy were enrolled in the study and were evaluated before and after treatment using Hoffman reflex and H/M ratio. They were randomly distributed into two groups of equal number; each group consisted of fifteen children. Group A received an exercise therapy program while wearing ankle foot orthosis as a home routine, two sessions per week for twenty weeks. Group B received the same exercise therapy program in addition to an aquatic exercise program for twenty weeks two sessions per week for twenty weeks. Results: The results revealed significant difference in all measured variables regarding group A and B when comparing pre and post treatment mean values (P<0.0001) Statistically significant improvement was observed in favor of group B. Conclusion: Combination of exercise program and aquatic exercise program had significant effect on decreasing H-reflex in spastic hemiplegic cerebral palsy.
Keywords
Cerebral Palsy, Spasticity, Hemiplegia, Aquatic Exercise, H-reflex
Received: April 9, 2015
Accepted: June 19, 2015
Published online: August 12, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Cerebral palsy (CP) is one of the most common causes of activity limitation in children. It has been defined as a non–progressive disorder of posture and movement (1) that occurs due to brain lesion as a part of the central nervous system (2).
Children diagnosed with cerebral palsy demonstrate increased muscle activity to sustain posture, agonist/antagonist co-contraction, impaired postural control, inadequate force production, and restricted voluntary and selective control of movement. These impairments not just interfere with functional activities, but also eliminate opportunities and/or willingness to participate in leisure, community and school activities (3). Hemiplegia is a condition affecting one side of the body. It is often referred to a ‘right’ or’ left sided’ depending on the side of the body that is affected. Sensory loss in the affected arm or leg is common in nearly half of the children who have hemiplegia and can contribute to difficulties, particularly in using the affected arm (4).
Children with spastic cerebral palsy may have decreased strength, balance, and skill in activities of daily living as a result of decreased postural stability. Their mobility may be impaired and they are liable to develop contractures and deformities in their spine and extremities (5).
Spasticity is one of the most frequently observed phenomena in hemiplagia. It is commonly agreed to be ‘a velocity-dependent increase of tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from the hyper-excitability of the stretch reflex, as one component of the upper motor neuron syndrome. Various methods have been proposed in literature for the assessment of spasticity of clinical, biomechanical, and neurophysiological origin. Electromyography (EMG), using surface electrodes, is a reliable method for evaluation of spasticity. Electromyography is a measurement of the electrical activity of skeletal muscles that are recorded with the placement of small metal discs, called "electrodes," applied to the skin’s surface. It is useful for assessing nerve and muscle function. (6). EMG signals are electrical signals that precede mechanical activity of skeletal muscles from which several parameters can be derived to provide information about anatomical, and physiological muscle properties, and neuromuscular control (7).
Hoffmann reflex (H-reflex) is a low threshold, spinal reflex that can be elicited by electrical stimulation of a mixed peripheral nerve. The reflex is usually considered to be monosynaptic, although there is some evidence that it might be disynaptic or trisynaptic in origin. The H- reflex allows assessing the excitability of the alpha motor-neuron. The F- wave is a response of small amplitude that follows the M response. Recording the H- reflex F- response, and H/M or F/M ratio can provide quantitative information about spasticity, (8). The M-wave has a higher threshold for excitation compared to the H-reflex. At low stimulus intensities, the H-reflex appears without the M-wave. When the stimulation level increases, at first the H-reflex amplitude increases and gradually the M-wave occurs, (7).
Exercise is a planned structured activity involving repeated movement of skeletal muscles that result in energy expenditure and seek to improve and maintain levels of physical fitness (9). Aquatic therapy, is the use of water and water-induced resistance to improve physical function (10). As a result, aquatic physical activity protects the joint integrity than land-based activity (11). Previous studies have reported that applying motor skills in water can potentially increase confidence and lead to less resistance with difficult tasks when compared to land training (12). Moreover, activities in the water is a pleasure for children, enhancing motivation and interest (13).
Research evaluating the effects of exercise for children with CP has focused primarily on land-based exercise (14) It has been reported that under water exercises are suitable for children with CP, particularly for those with significant mobility impairments. In water, poor balance, poor postural control, and excessive joint loading is reduced (15).
The purpose of this study was to investigate the effect of an aquatic exercise program on muscle tone in spastic hemiplegic children.
2. Subjects, Instrumentations, and Procedures
2.1. Subjects
Of 42 children, 9 did not meet the inclusion criteria, and 3 refused to participate, thus only 30 children (11 females and 19 males) with age ranged from 5 to 7 years participated in the study. Participants were recruited from the outpatient clinic of the Faculty of Physical Therapy, Cairo University. From the 30 children, 13 were right sided and 17 were left sided hemiplegic cerebral palsy children. There were no associated disorders other than spasticity, with minimal non-significant perceptual defects. The study started from June 2013 and lasted to September 2014.
Subjects included in this study were meant to be:
• Able to follow instructions given to them.
• The degree of spasticity ranged from mild to moderate grade according to the modified Ashwroth scale. (16)
• The involved lower limb was free from any structural deformities.
• No genetic disorders.
• No visual or auditory deficits.
Exclusion criteria:
• Children with fixed deformities.
• Children with involuntary movement.
• Children receiving anti-spastic drugs.
• Children with diminished vital capacity and/or unstable cardiac conditions.
• Children with infectious dermatological conditions.
The study was approved by the Ethical Committee of Cairo University. Parents of the participated children were provided with a Volunteer Information Sheet and a written consent informing them about the purpose of the study, its benefits, inherited risks, their commitment to time, and money. The chance to withdraw from the study was allowed any time without providing any reasons. Children who met the inclusion criteria were randomly assigned by the use of computer based 1:1 randomization scheme into 2 groups of equal number (A and B). Five-blind evaluations to determine H/M ratio was conducted for each child individually before and after twenty weeks of treatment.
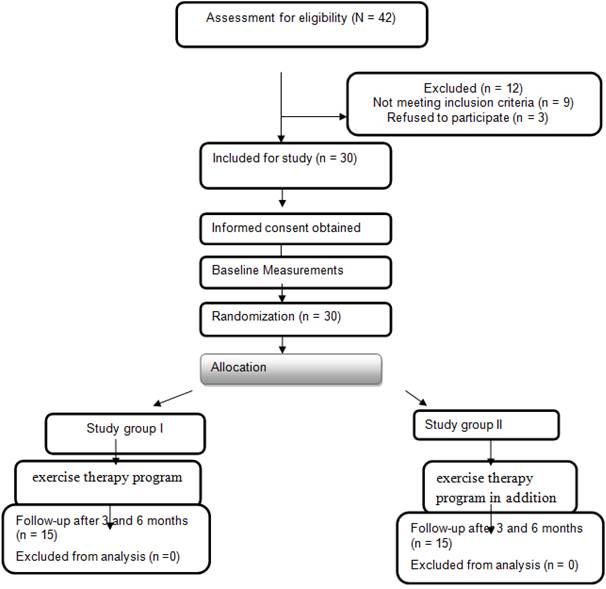
Figure 1. Chart showing the experimental design of the study.
Group A (control group) consisted of 15 subjects with mean age 5.76 ±1.41 years, received exercise therapy program for 20 weeks.
Group B (study group) consisted of 15 subjects with mean age 5.81 ±1.79, received aquatic exercise program twice weekly in addition to the same exercise therapy program given to group A for 20 weeks.
2.2. Instrumentation
2.2.1. For Evaluation
(i) A computerized electromyography apparatus (Diza 2380) was used to determine the Hoffman reflex and Myogenic response (H/M) ratio.
(ii) Electrogeniometer was used to determine the degree of ankle excursion.
2.2.2. For Treatment
(i) A flexible, light weight, easy worn with regular shoes, ankle foot orthosis (AFO) made of polypropylene was used. It covered the entire calf, medial and lateral borders of the leg and sole of the foot and was fitted by straps crossing the anterior aspect of upper part of tibia and anterior aspect of the ankle.
(ii) Swimming pool to apply under water exercises.
(iii) Floating aids.
(iv) Tumble forms (mat, wedges, rollers and balls) from Preston for the application of the exercise program.
2.3. Procedures
2.3.1. For Evaluation
Five blind evaluations were conducted for each child of both groups in a warm, well lighted, quiet room, before and after twenty weeks of treatment to determine H/M ratio.
(i) H/M ratio: Using computerized electromyography, each child was placed in a comfortable prone position on the examination table. The surface electrodes were then placed for recording the electromyography signals of the soleus muscle. The tibial nerve present in the popliteal fossa was stimulated. The active electrode was placed two centimetres distal to the separation of the gastrocnemius muscle, and secured by adhesive tape. The reference electrode was placed three centimetres distal to the active electrode, while the earth electrode was placed between the two electrodes. Maximum Hoffman reflex and maximum myogenic responses were recorded. The H/M ratio was then calculated to measure the motor neuron pool excitability which reflects the level of spasticity as an indication of central nervous system excitability.
2.3.2. For Treatment
(i) Group A (control) received exercise therapy program including neuro-developmental technique, proprioceptive training, facilitation of righting and equilibrium reactions, stretching techniques for hip flexors, hip adductors, hamstrings and tendo-Achillis. In addition to wearing an ankle foot orthosis as a home routine.
(ii) Group B (study) received the same exercise therapy program given to group A, in addition to the aquatic exercises therapy program for 45 minutes 2/week for a total of 20 sessions. In addition to wearing an ankle foot orthosis as a home routine.
All participants used floating vests to ensure safety throughout the study. The aquatic program consists of the following activities in a 31-32°C pool:
10 minute warm up exercises focusing on the upper and lower extremities as well as cervical motions
15 minute relay race in the deep end of the pool
5 minute "relaxation period" – floating in a supine position, making no active motion
15 minutes aquatic play activity – at the shallow end of the pool; consists of a modified synchronized swim, a balloon game, volleyball, and standing using a floating board Ballaz et al.,2011.
3. Results
The collected data of this study demonstrated the statistical analysis of the results of Hoffman reflex via H/M ratio in hemiplegic cerebral palsy. The raw data for the two groups were statistically treated to show the mean and standard deviation. Student t-test was then applied to determine the significance of treatment for each group, with P value at ˂ 0.05. The results revealed no significant difference, when comparing the pre- treatment mean values of the two groups. Significant improvement was observed in each group when comparing the pre and post treatment mean values of H/M ratio. Significant difference was denoted in favor of group B when comparing the post treatment results of the two groups. The data will be presented in a form of tables and bar graphs.
3.1. Subject Characteristics
There were no device related problems, no systemic or local complications. The baseline characteristics were similar and without statistical significance for both groups (table 1). All patients were re-assessed after treatment period and at 6 months follow-up.
Table 1. Baseline characteristics of both groups.
| Characteristics | Group A | Group B | P value |
| Patients number | 15 | 15 | |
| Male/Female | 7/8 | 6/9 | |
| Mean Age | 5.76±1.41 | 5.81±1.79 | P > 0.05 |
3.2. H/M Ratio
The raw data of the H/M ratio was collected from the gastocnemius muscle of the affected lower limb. The obtained results revealed minimal differences in the H/M ratio when comparing the pre- treatment mean values of the two groups which was not statistically significant. Considerable reduction was observed in the mean values of H/M ratio of the two groups A and B (˂0.05 and ˂0.001 respectively), when comparing their pre and post treatment mean values. Significant differences was observed in favor of group B, while comparing its post treatment mean values with the post treatment mean values of group A.
Table 2. Pre and post-treatment mean values of H/M ratio for groups A and B.
| Group A (control) | Group A (study) | |||
| Pre | Post | Pre | Post | |
| X` | 67.7 | 56.8 | 69.6 | 43.2 |
| ± SD | ± 3.72 | ± 3.92 | ± 3.98 | ± 4.91 |
| P-value | < 0.05 | < 0.001 | ||
| Level of Significance | Significant | Significant | ||
X`: Mean SD: Standard deviation P-value: Level of significance Sig.: Significance
Significant improvement was also observed when comparing the post-treatment mean values of H/M ratio of the two groups in favor of group B (P<0. 001)
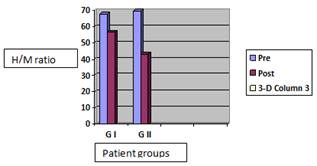
Figure 2. Pre and post-treatment mean values of H/M ratio (mV.) for groups A and B
4. Discussion
Functional limitations of the children with cerebral palsy are mainly in mobility, balance and delay in acquiring motor milestones (17). H-reflex evoked in the soleus was used for evaluation of muscle tone since H- reflex persists to adult life to determine the excitability changes in the spinal motor neurons in spastic children. This comes in accordance with Mayston (18), who stated that, various clinical and electrophysiological tests are used for assessing the degree of spasticity. Electrophysiological studies are considered more reliable measures of spasticity in childhood community.
In addition, the dynamic systems theory of motor development explains the acquisition of motor skill as a dynamic and self-organizing process resulting from the interaction of multiple subsystems within the child, the environment, and the task. Approaches based on the principles of the dynamic systems theory emphasize, the child’s active and volitional role in therapy and target subsystems within the child in addition to the central nervous system. The dynamic systems theory has encouraged therapists to consider the influence of fitness parameters, such as muscle strength, cardiovascular fitness, and flexibility, on the movement abilities and participation levels of children with CP (19).
Gromley, 2001(20) reported that in hemiplegia, hypertonia contributes to muscle weakness in coordination and range limited movement. Spasticity is a major cause of disability and handicap and it usually represents a major challenge to the management of different neurological disorders. It is considered as one component of the upper motor neuron lesions.
Spasticity-related changes in muscle tone probably result from alterations of the balance of inputs from reticulospinal and other descending pathways to the motor and interneuronal circuits of the spinal cord, along with the absence of an intact corticospinal system. Loss of descending tonic or phasic excitatory and inhibitory inputs to the spinal motor apparatus, alterations in the segmental balance of excitatory and inhibitory control, denervation supersensitivity, and neuronal sprouting may be observed. (21)
During the development of spasticity, the spinal cord undergoes neurophysiologic changes in the excitability of motor neurons, interneuronal connections, and local reflex pathways. The excitability of alpha motor neurons increased, as it was suggested by enhanced H-M ratiosand F-wave amplitudes. Judging by the recordings from Ia spindle afferents, muscle spindle sensitivity has not increased in human spasticity. (22).
Statistical analysis of the post treatment results of the present study revealed great improvement in H/M ratio for both control and study groups of A and B when comparing their pre and post treatment mean values. Improvement was noticed in favor of group B receiving aquatic therapy program, in addition to the exercise therapy program and AFO, when comparing its post treatment mean values with that of group A.
These results reinforced the evidence of using aquatic therapy program in children with spastic hemiplegic cerebral palsy who demonstrate muscle spasticity. In this present study, neuro-developmental techniques and a home routine of AFO together with aquatic exercise program was applied to the study group. This comes in agreement with Thorpe and Reilly 2000(23) who reported that, aquatic resistive exercise program therapy could improve functional mobility and balance in adults with cerebral palsy. This coincided with Peganoff 1984 (24) who stated that, aquatic exercises can improve flexibility in adolescence with cerebral palsy. The results supports that of Dorval et al., 1996 (25) who mentioned that, aquatic therapy program can improve movement and function in adolescent cerebral palsied patients. This also agrees with Poyhonen et al., 2002(26) who cleared that, the aquatic resistance training improved neuromuscular performance in healthy women. This confirms the findings of Ballaz et al., 2011(27) who posted that, the Group aquatic training improves gait efficiency in adolescents with cerebral palsy.
This may be attributed to that; aquatic exercise is an attractive form of exercise for children with CP. The buoyancy of water decreases the influence of gravity and provides increased postural support. These characteristics may allow children with CP to exercise in water with more freedom than on land. The resistive forces of buoyancy and viscous drag permit a variety of aerobic and strengthening activities that can be easily modified to accommodate the wide range of motor disabilities of children with CP. An additional benefit of aquatic exercise is the reduced levels of joint loading and impact, providing a gentler environment for children with unstable joints who experience persistent and abnormal loading (28). Studies involving developing children and children with asthma report a magnificent improvement in aerobic capacity for children engaging in aquatic exercise two or more times a week. When a body is immersed in warm water (30°to 31°C), its core temperature increases, causing reduction in gamma fiber activity which in turn reduces muscle spindle activity, facilitates muscle rehabilitation techniques and reducing spasticity, thus resulting in increased joint range of motion and consequently creating better postural alignment (29).
Buoyancy is one of the physical properties of water which provides postural support and reduces loading on unstable joints to allow children with CP to move independently (15). Bouyancy is a force which can assist, resist and support movement in water (30). Unrestrained movement and the ability to use muscles which have trouble overcoming gravitational constraints are the primary reasons why swimming and any related aquatic activities are suitable for individuals with a wide range of physically disabling conditions which include amputation, cerebral palsy and even paraplegia (31). Aquatic activities also enhance breath control and improve the functions of cardiorespiratory system to move and swim without help of others, he seems to improve his self-esteem and self-awareness (32). Water actually represents a medium in which everyone can take part in recreational and therapeutic activities, irrespective of their age (33).
5. Conclusion
Adding underwater exercises to the exercise program are effective for controlling spasticity in hemiplegic cerebral palsy children.
Conflict of interest: The authors declared no conflict of interest .
Funding: The authors received no fund from any individual or organization
References
- Nolan K, Cole Land Liptak G (2006).Use of botulinum toxin type A in children with cerebral palsy .Phys Ther:(86): pp:573-584.
- Koman L, Smith B, Kalkrishnan R. (2003). Spasticity associated with cerebral palsy in children: guidelines for the use of botulinum A toxin. Paediatr Drugs (5) pp:11-23.
- Prosser L, Lee S, VanSant A,et al (2010).Trunk and hip muscle activation patterns are different during walking in young children with and without cerebral palsy. Phys Ther; 90(7):90–97
- Park S and Nottingham A (2010). Information for parents Cerebral palsy , 3rd edition pp:8
- Wilsdon J (1996).Cerebral palsy. In: Turner A, Foster M., Johanson S.E. and Steward. Occupational therapy and physical dysfunction (principles, skills and practice), Churchill Livingstone, New York, pp:395-431.
- Zhu P(2010). Design of Surface Electromyography Detection Circuit, International Conference on Future Information Technology and Management Engineering, 978-1-pp:4244-9088
- Voerman G, Gregoric M. & Hermens H (2005). Neurophysiological methods for the assessment of spasticity: The Hoffmann reflex, the tendon reflex, and the stretch reflex. pp. 450-455.
- Nielsen J, Klinge K and Biering S (2006). Spasticity-assessment a review( 44) pp:708–722
- Katsimanis G, Evaggelinou C, Christoulas K, Kandrali I, Angelopoulou N. (2002) Using a training program to enhance the aerobic power in young individuals with spastic diplegia. In: Koskoulou M, Geladas N, Klissouras V, editors. 7th Annual Congress of the European College of Sport Science. Athens, Greece: p 153.
- K. S. Ondrak and D. E. Thorpe, "Physiologic responses of adolescents with CP when walking on land and in water: a case series," Journal of Aquatic Physical Therapy, vol. 15, pp. 10–15, 2007.
- M. A. Fragala-Pinkham, H. M. Dumas, C. A. Barlow, and A. Pasternak, "An aquatic physical therapy program at a pediatric rehabilitation hospital: a case series," Pediatric Physical Therapy, vol. 21, no. 1, pp. 68–78, 2009.
- R. Retarekar, M. A. Fragala-Pinkham, and E. L. Townsend, "Effects of aquatic aerobic exercise for a child with cerebral palsy: single-subject design," Pediatric Physical Therapy, vol. 21, no. 4, pp. 336–344, 2009.
- D. E. Thorpe, M. Reilly, and L. Case, "The effects of an aquatic resistive exercise program on ambulatory children with cerebral palsy," Journal of Aquatic Physical Therapy, vol. 13, pp. 21–35, 2005.
- Blundell SW, Sheperd RB, Dean CM, Adams RD, Cahill BM. (2003) Functional strength training in cerebral palsy: a pilot study of a group circuit training class for children aged 4–8 years. Clin Rehabil 17: 48–57..4,7,17,23–29
- Kelly, M., & Darah, J. (2005). Aquatic exercise for children with cerebral palsy. Developmental Medicine & ChildNeurology, 47, 838–842.
- Bohannon R. and Smith M (1987). Interrater reliability of a modified Ashworth scale of muscle spasticity." Physical Therapy 67(2) pp:206.
- Kott, K.: Orthosis for patients with neurological disorders. Clinical decision making. In: Seymour, r., (ed.), Prosthetics and Othotics: Lower limb and spinal. Lippincott Williams and Wilkins, London. 367-426, 2002.
- Mayston M (2004). Physiotherapy management in cerebral palsy: an update on treatment approaches. Clinics in Developmental Medicine (161)pp : 147-160.
- Darrah J, Law M, Pollock N. (2001) Family-centered functional therapy – a choice for children with motor dysfunction. Infants Young Child 13: 79–87.
- Gormley,M E, JR., L E, Kratch, (2001): Spasticity management in the child with spastic quadriplegia. Eur J neural 8 (supply,5):127-135.
- Shinohara T, Suzuki N, Oba M, Kawasumi M, Kimizuka M, Mita K. (2002) Effect of exercise at the AT point for children with cerebral palsy. Bull Hosp Joint Dis 61: 63–67.
- Stein, J. (2004) Motor Development, the Brain, and Aquatic Therapy. American Therapy Journal, 6 (2) July 2004
- Thorpe DE, Reilly M. (2000) The effect of an aquatic resistive exercise program on lower extremity strength, energy expenditure, functional mobility, balance and self-perception in an adult with cerebral palsy: a retrospective case report. J Aquat PhysTher 8: 18–24.
- Peganoff SA. (1984) The use of aquatics with cerebral palsied adolescents. Am J Occup Ther 38: 469–473.
- Dorval G, Tetrault S, Caron C. (1996) Impact of aquatic programmes on adolescents with cerebral palsy. Occup Ther Int 3: 241–261.
- Poyhonen T, Sipila S, Keskinen KL, Hautala A, Savolainen J, Malkia E. (2002) Effects of aquatic resistance training on neuromuscular performance in healthy women. Med Sci Sports Exerc 34: 2103–2109.
- Ballaz L, Plamondon S, Lemay M. Group aquatic training improves gait efficiency in adolescents with cerebral palsy. Disabil Rehabil. 2011; 33 (17-18): 1616-1624.
- Dodd KJ, Taylor NF, Damiano DL. (2002) A systematic review of effectiveness of strength-training programs for people with cerebral palsy. Arch Phys Med Rehabil 83: 1157–1164.
- Dumas H, Francesconi S. (2001) Aquatic therapy in pediatrics: annotated bibliography. Phys Occup Ther Pediatr 20: 63–79.
- Irion, J.M. (2009). Aquatic properties and therapeutic interventions In: L. T. Brody, P.R. Geigle (Eds), Aquatic exercise for rehabilitation and training (pp. 25-34). Champaign: Human Kinetics.
- Prins, J.H. (2009). Aquatic rehabilitation. Serbian Journal of Sports Sciences, 3(1-4), 45-51.
- Lepore, M. (2005). Aquatics. In: J.P. Winnick (Ed.), Adapted Physical education and Sport (pp.435-454). Champaign: Human Kinetics.
- Daly, D., & Lambeck, J. (2007). New trends in adapted swimming. In Colomina R., Molina J., Valdivieso F., Ortiz E., Contreras G. (Eds.), Swimming science I (pp. 19-30). Granada, Spain: Editorial Universidad de Granada.



