Detection of Staphylococcus aureus-Specific Gene and Simultaneous Confirmation of Methicillin Resistant Staphylococcus aureus (MRSA) by Polymerase Chain Reaction
Kumurya A. S.*
Department of Medical Laboratory Science, Faculty of Allied Health Sciences, Bayero University, Kano, Nigeria
Abstract
Background: The differentiation of Methicillin resistant Staphylococcus aureus (MRSA) strains from other strains of S. aureus has important implications for the treatment and management of patients with S. aureus infections. Detection of the mecA gene by PCR has been described as a rapid method for the identification of MRSA. Objectives: A molecular assay for the simultaneous detection of a Staphylococcus aureus-specific gene and the mecA gene, responsible for the resistance to methicillin in staphylococci, was evaluated. Methods: In a clinical study, 100 isolates of Staphylococcus aureus were investigated. Polymerase chain reaction (PCR) was used (with a Techne TC-5000 instrument-Bibby Scientific Ltd.) to amplify both the S. aureus specific sequence gene and mecA gene of 100 isolates with the amplicon size of 107 and 532bp. To accelerate the procedure of identification in clinical microbiology laboratories, simple and rapid method for DNA extraction directly from a single colony was employed. The assay included a rapid DNA extraction protocol conducted in 15 minutes and PCR conducted. The performance and robustness of the assay was evaluated with a control strain of methicillin susceptible Staphylococcus aureus-ATCC 25923 (MSSA). The specificity of the new molecular assay was tested with a bacterial strain of methicillin susceptible Staphylococcus aureus-ATCC 25923 (MSSA). Results: All clinical the isolates gave positive results for the S. aureus-specific genomic target, and only five isolates (5.0%) were positive for the mecA gene. Conclusion: The new rapid DNA extraction protocol was found to be quick, robust, and labor saving and it proved to be suitable for a routine molecular diagnostic laboratory. On the basis of this finding; establishment of molecular diagnostic laboratory in secondary and tertiary health units is urgently required.
Keywords
Staphylococcus Aureus, MRSA, MecA Gene, DNA Extraction, PCR
Received: April 9, 2015
Accepted: April 23, 2015
Published online: May 28, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Staphylococcus aureus has been known to be a major pathogen causing a wide spectrum of clinical manifestations, such as wound infections, pneumonia, septicemia, and endocarditis, with beta-lactam antibiotics being the drugs of choice for therapy. Since the introduction of methicillin into clinical use in 1961, the occurrence of methicillin-resistant S. aureus (MRSA) has steadily increased and nosocomial infections caused by such isolates have become a serious problem worldwide (Benner and Kayser, 1968; Lowy, 1998).
The differentiation of MRSA strains from other strains of S. aureus has important implications for the treatment and management of patients with S. aureus infections, and glycopeptides are the drugs of choice for infections caused by MRSA strains. Furthermore, evidence of MRSA requires extensive hygienic precautions to limit the spread of such strains (Wenzel et al., 1998; Chaix et al., 1999).
In the clinical laboratory, S. aureus is identified by growth characteristics and by the subsequent detection of catalase and coagulase activities. Conventional susceptibility testing of S. aureus reliably detects resistance to methicillin or oxacillin if agar dilution tests, disk diffusion tests, or agar screening methods are used according to the standards of the National Committee of Clinical Laboratory Standards (NCCLS) (NCCLS, 1993; NCCLS, 1999). Standard susceptibility tests, however, are time-consuming. Because the phenotypic expression of methicillin resistance in vitro is heterogeneous and sometimes difficult to induce, false-negative results may be observed (Ubukata et al., 1989; Ribeiro et al., 1999). Furthermore, S. aureus strains may show a false-negative or non-interpretable result when commercially available kits for coagulase testing (Ruane et al., 1986; Weeres-Pothoff et al., 1987; Fournier et al., 1989; Unal et al., 1994; Wilkerson et al., 1997) are used.
The main mechanism of methicillin resistance is induced by the presence of an additional low-affinity penicillin-binding protein, PBP2a (encoded by the mecA gene), or, in rare cases, induced by the hyper production of β-lactamase (Waxman and Strominger, 1983; Hartman and Tomasz (1984; Chambers, 1993). Detection of the mecA gene by PCR has been described as a rapid method for the identification of MRSA (Tokue et al., 1991; Brakstad et al., 1992; Tokue et al., 1992; Unal et al., 1994; Barski et al., 1996; York et al., 1996; Kearns et al., 1999; Martineau et al., 1998; Kohner et al., 1999).
In the present study, a molecular assay for the rapid identification of MRSA was established and evaluated. The new assay targeted both the S. aureus gene and the mecA gene within a single PCR and was based on automated DNA isolation and real-time PCR.
2. Materials and Methods
2.1. The Study of Areas
A total of 8 health institutions located in six states in Northwestern Nigeria, were enrolled in the study. The health institutions were two teaching hospitals [Aminu Kano Teaching Hospital (AKTH) and Ahmadu Bello University Teaching Hospital (ABUTH)], three Federal Medical Centres [Federal Medical Centres Birnin Kudu (FMCB), Federal Medical Centre Gusau (FMCG) and Federal Medical Centre Katsina (FMCK) located in Jigawa, Zamfara and Katsina state in Northwestern Nigeria respectively], two Specialist Hospitals [Murtala Muhammad Specialist Hospital, Kano (MMSH) and Specialist Hospital Sokoto (SHS) located in Kano and Sokoto states of Northwestern Nigeria respectively] and the Infectious Diseases Hospital (IDH) located in the city of Kano, Kano State.
2.2. Specimen Collection
A total of 100 consecutive non – duplicated Staphylococcus aureus isolates were obtained from clinical samples in 8 health institutions across Northwestern Nigeria. The isolates were collected from the eight hospitals during two years period from February 2008 to April 2010. Routine clinical microbiology specimens were selected during the period. The quality control and rejection criteria of specimen were followed (Isenberg, 1998). Staphylococcus aureus ATCC 25923 was used as a reference control organism. Specimens were processed within 2 hours of collection by the standard microbiology technique. The sheep blood agar and mannitol salt agar were used for inoculation and the agar plates were then incubated at 350C for 18-24 hours in aerobic atmosphere (NCCLS, 2003).
2.3. Study Design
A molecular assay for the detection of MRSA based on rapid DNA extraction method was established. The new assay was based on rapid DNA extraction and PCR with a Techne TC-5000 instrument (Bibby Scientific Ltd).In the first step, 100 clinical isolates of Staphylococcus aureus were tested. S. aureus strains were identified by their characteristic growth morphologies, Gram stain characteristics, reaction to catalase, and coagulase production were detected. After identification, the strains were stored at −80°C [Micro bank (Diagnostic pro-lab)]. For molecular testing, clinical specimens were thawed and recultured on blood agar overnight at 37°C. Portions of individual bacterial colonies were suspended in 25µl of sterile distilled water. In the second step, the specificity of the new molecular assay was determined with a suspension of the S. aureus strain of methicillin susceptible Staphylococcus aureus-ATCC 2592 (American Type Culture Collection, Manassas, Va.). In the third step, the molecular assay of the 100 Staphylococcal isolates was determined.
2.4. DNA Extraction
After overnight culture on brain heart infusion (Difco Laboratories) agar plates, one colony of each sample was resuspended in 25 µl of sterile distilled water and the suspension was then placed in a 100°C heat block for 15 min. From this suspension, a 5-µl volume was directly used as a template for PCR amplification (Pérez-Roth et al., 2001).
2.5. Primers
The oligonucleotide primers used in this study have been previously described (Martineau et al., 1998; Meshref et al., 2011) and were obtained from a commercial source (Inqaba Biotechnical Industries (Pty) Ltd., South Africa). The 3-end region of the S. aureus specific gene was amplified using A 30 nucleotide forward primer 5’- AATCTTTGTCGGTACACG ATA TTCTTCACG -3’ and A30 nucleotide reverse primer, 5’-CGTAAT GAG ATT TCAGTA GAT AATACAACA-3’ (which hybridize to 5-34 and (112-83), respectively, (Martineau et al., 1998). While The 3-end region of the mecA gene was amplified using A 22nucleotide forward primer 5’- AAA ATC GAT GGT AAA GGTTGG C - 3’ and A22 nucleotide reverse primer, 5’- AGTTCTGCAGTACCG GAT TTG C-3’ (which hybridize to sites 1282-1301 and 1814-1793) (Robert Koch institute, 2003) (Table 1). Staphylococcus aureus specific gene and mecA gene have the amplicon size of 107 and 532 bp using primers described by (Meshref et al., 2011).
Table 1. Oligonucleotide Primers used in the PCR assay
| Oligonucleotide | Sequence | Target |
| Position | Nucleotide | gene |
| A30fwd5-34 | AATCTTTGTCGGTACACGATATTCTTCACG | Sa |
| A30 rev112-83 | CGTAATGAGATTTCAGTAGATAATACAACA | Sa |
| A22fwd1282-1301 | AAAATCGATGGTAAAGGTTGGC | mecA |
| A22 rev1814-1793 | AGTTCTGCAGTACCGGATTTGC | mecA |
2.6. PCR Amplification
PCR assays were all directly performed from the bacterial suspension obtained after the rapid DNA extraction method described above. An aliquot of 5 µl of this suspension was added to 95 µl of PCR mixture consisting of 1× reaction buffer [16 mM (NH4)2SO4,67 mMTris-HCl (pH 8.8)], a 0.5mM concentration of each of the four deoxyribonucleoside triphosphates (dATP, dCTP, dGTP, and dTTP) (Inqaba Biotechnical Industries (Pty) Ltd., South Africa), 1.0μM of each primer, and mecA primer, and 1.25 U of The Dream Taq™ Green PCR Master Mix (2x) (Fermentas Life Sciences, supplied by Inqaba Biotechnical Industries (Pty) Ltd., South Africa) is a ready-to-use solution containing Dream Taq™ DNA polymerase, optimized Dream Taq™ Green buffer and 4mMMgCl2. For each sample, one reaction was performed with the pair of primers to identify S. aureus specific sequence gene and with the mecA pairs of primers to detect both resistance gene (mecA). In order to reduce the formation of nonspecific extension products, a hot-start PCR protocol was used; the tubes were placed in the thermal cycler when the denaturing temperature was reached. All PCR assays were carried out with a negative control containing all of the reagents without DNA template. DNA amplification was carried out in a Techne PCR system TC-5000 thermo cycler (Bibby Scientific Ltd.) with the following thermal cycling profile: an initial denaturation step at 94°C for 5 min was followed by1 cycle of amplification this was followed by denaturation at 94°C for 30 s, annealing at 55°C for 30 s, and extension at 72°C for 60 s ending with a final extension step at 72°C for 5 min. After PCR amplification,5 µl was removed and subjected to agarose gel electrophoresis(1.5% agarose, 1× Tris-borate-EDTA, 100 V, 40 min) to estimate the sizes of the amplification products by comparison with a 100-bp O’ GeneRuler™ 100bp molecular size standard DNA Ladder, ready-to-use designed by Ferment as Life sciences (supplied by Inqaba Biotechnical Industries (Pty) Ltd., South Africa) The gel was stained with ethidium bromide, and the amplicons were visualized using a UV light box. This protocol, including the rapid DNA extraction method from a single colony and electrophoretic analysis of the amplified products on an agarose gel, was completed within 4 hours.
3. Results
When a suspension of an MRSA strain with a turbidity equivalent to a McFarland standard of 0.5 was repeatedly tested by a molecular assay based on the rapid DNA extraction protocol and rPCR on an instrument, the crossing points of both targets were always found to be within one cycle. All the isolates (n=100) expressed S. aureus specific sequence gene in their PCR products which confirmed the assumption that all the strains were Staphylococcus aureus. Fig. 1 shows a representative agarose gel electrophoresis of PCR products. Only 5 isolates (5.0%) were confirmed as MRSA based on the detection of mecA gene. No contamination was observed at any time during the study. The size of the amplicon was expected to be 532 base pairs (bp). An amplicon of 532bp was seen in only 5 of the 100 isolates (which were found to be MRSA isolates using the by phenotypic method) tested. PCR amplification of mecA gene demonstrating amplicon of 532bp products are given in Fig. 2.
The 100 Staphylococcus aureus of isolates were derived from wounds (31 samples), the urine samples (26 samples), the high vaginal swabs (12 samples), the sputum samples (11 samples), the ear swabs (9 samples), the blood cultures (8 samples), the urethral swabs (2 samples), and the semen samples (1 sample). Among the MRSA strains, three MRSA isolate was detected in wound samples. The remaining 2 MRSA isolates were detected in urine samples. The overall distribution of Staphylococcus aureus used in the PCR assay according to the study area is given in Table 2.
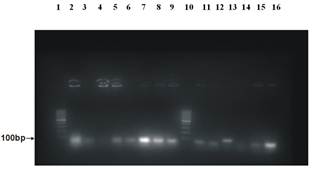
Figure 1. Agarose gel electrophoresis patterns showing PCR amplification products from S. aureus isolates. A 100 molecular weight size marker (O’ GeneRuler™ 100bp ladder) was applied at the lane 1 and 10 of the gel to identify the isolated genes. A negative control (methicillin susceptible S. aureus, ATCC 25923) was applied at the lane 13. PCR products of the test samples were applied on lane 2,3,4,5,6,7,8,9,11,12,14,15 and 16 which showed clear bands confirmed that all the isolates were Staphylococcus aureus.
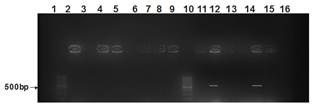
Figure 2. Representative agarose gel electrophoresis of PCR products. Lanes 12, 14 are positive for mecA as indicated by 532bp PCR product (Methicillin Resistant S. aureus isolates), Lane 2-9, 11, 13, 15, are negative for mecA (Methicillin Susceptible S. aureus isolates), Lane 16: negative control (methicillin susceptible S. aureus, ATCC 25923); Lane 1, 10: molecular weight size marker.
Table 2. Distribution of Staphylococcus aureus isolates according to the type of specimen.
| Specimen type | Staphylococcus aureus isolates | ||
| No. of mecA+ (%) | No. of mecA-(%) | Total (%) | |
| Wound swabs | 3 (9.7) | 28 (90.3) | 31 (31.0) |
| Ear swabs | 0 (0.0) | 9 (100) | 9 (9.0) |
| Blood culture | 0 (0.0) | 8 (100) | 8 (8.0) |
| Urine | 2 (7.7) | 24 (92.3) | 26 (26.0) |
| High vaginal swabs | 0 (0.0) | 12 (100) | 12 (12.0) |
| Sputum | 0 (0.0) | 11 (100) | 11 (11.0) |
| Semen | 0 (0.0) | 1 (100) | 1 (100) |
| Urethral swabs | 0 (0.0) | 2 (100) | 2 (100) |
| Total | 5 (5.0) | 95 (95.0) | 100 (100) |
Mean = 0.285714, SE = 0.285714, SD = 0.755929, CL (95.0%) =0.699118
4. Discussion
Since the introduction of semi synthetic penicillins, such as methicillin and oxacillin, for the therapy of infections caused by S. aureus, the occurrence of S. aureus strains resistant to methicillin has steadily increased and MRSA strains have become major nosocomial pathogens (Panlilio et al., 1992; Voss et al., 1994). Infections with MRSA strains require treatment with glycopeptide antibiotics, which can be nephro- and ototoxic. Additionally, a diagnosis of MRSA infection has important implications for the management of patients since an extensive set of hygienic precautions must be taken to limit the spread of MRSA (Boyce, 2001).
Therefore, a rapid and reliable diagnosis of infection by MRSA is of major importance. Although S. aureus is relatively easy to cultivate, conventional identification methods may yield false-positive or false-negative results (Wallet et al., 1996; Frebourg et al., 1998). Standard susceptibility tests are time-consuming. The correct identification of S. aureus and the detection of the mecA gene based on molecular methods have evolved as the method of choice for definitive identification. Earlier studies, however, involved more or less complicated manual DNA extraction protocols, followed by single or multiplex PCR with detection of amplification products on agarose gels (Barski et al., 1996; Brakstad et al., 1992; Tokue et al., 1991; Tokue et al., 1992; Unal et al., 1994; York et al., 1996; Martineau et al., 1998; Kearns et al., 1999; Kohner et al., 1999). Those assays, however, were time-consuming, prone to contamination, and not suitable for routine diagnostic laboratories because of the lack of a hybridization technique.
Recently, a real-time PCR technique for the detection of MRSA with two separate PCRs based on a manual DNA extraction protocol was described (Tal et al., 2001). In that study, however, no internal control was employed. (Reischl et al., 2000) described a manual DNA extraction protocol followed by multiplex real-time PCR for the simultaneous detection of the mecA gene and an S. aureus-specific gene which served as an internal control. In comparison to the conditions used in that study, primer compositions and concentrations had to be changed in our study to balance PCR efficiencies for both of the targets by optimization of primer concentrations and product lengths. Because variations in lot-to-lot primer concentrations may exist, it is advisable to adjust the concentrations for each primer lot prior to its first use in routine diagnostics.
In spite of the growing consensus for the use of molecular methods, they are not yet available in the majority of routine diagnostic laboratories because of their elevated technical requirements. In the present study, a new molecular assay that targets both an S. aureus-specific gene and the mecA gene within a single PCR was established and evaluated. This assay includes a rapid DNA extraction protocol and PCR on a Techne TC-5000 instrument.
5. Conclusion
The new molecular assay was found to be rapid and robust. Because it is a largely automated assay, less hands-on work is needed and it can be incorporated into the workflow of a routine diagnostic laboratory. On the basis of this finding; establishment of molecular diagnostic laboratory in secondary and tertiary health units is urgently required.
Acknowledgments
I thank Dr. Muhammad Yalwa Gwarzo for his valuable technical help in this study.
References
- Barski, P., L. Piechowicz, J. Galinski, and J. Kur (1996). Rapid assay for detection of methicillin-resistant Staphylococcus aureus using multiplex PCR. Mol. Cell. Probes 10:471-475.
- Benner, E. J., and F. H. Kayser (1968). Growing clinical significance of methicillin-resistant Staphylococcus aureus. Lancetii:741-744.
- Boyce, J. M (2001). MRSA patients: proven methods to treat colonization and infection. J.Hosp. Infect.48:(Suppl. A):9-14.
- Brakstad, O. G., K. Aasbakk, and J. A. Maeland (1992). Detection of Staphylococcus aureus by polymerase chain reaction amplification of the nuc gene. J. Clin. Microbiol. 30:1654-1660.
- Chaix, C., I. Durand-Zaleski, C. Alberti, and C. Brun-Buisson (1999). Control of endemic methicillin-resistant Staphylococcus aureus: a cost-benefit analysis in an intensive care unit JAMA 18:1745-1751.
- Chambers, H. F(1993). Detection of methicillin-resistant staphylococci. Infect. Dis. Clin. N.Am. 7:425-433.
- Chambers, H. F (1997). Methicillin resistance in staphylococci: molecular and biochemical basis and clinical implications. Clin. Microbiol. Rev. 10:781-791.
- Fournier, J. M., A. Boutonnier, and A. Bouvet (1989). Staphylococcus aureus strains which are not identified by rapid agglutination methods are of capsular serotype 5. J. Clin. Microbiol. 27:1372-1374.
- Frebourg, N. B., D. Nouet, L. Lemée, E. Martin, and J.-F. Lemeland (1998). Comparison of ATB Staph, Rapid ATB Staph, Vitek, and E-test methods for detection of oxacillinheteroresistance in staphylococci possessing mecA. J. Clin. Microbiol. 36:52-57.
- Hartman, B. J., and A. Tomasz (1984). Low-affinity penicillin-binding protein associated withβ-lactam resistance in Staphylococcus aureus. J. Bacteriol. 158:513-516.
- Kearns, A. M., P. R. Seiders, J. Wheeler, R. Freeman, and M. Steward (1999). Rapid detection of methicillin-resistant staphylococci by multiplex PCR. J. Hosp. Infect. 43:33-37.
- Kessler, H. H., G. Muehlbauer, E. Stelzl, E. Daghofer, B. I. Santner, and E. Marth (2001). Fully automated nucleic acid extraction. MagNA Pure LC. Clin. Chem. 47:1124-1126.
- Kohner, P., J. Uhl, C. Kolbert, D. Persing, and F. Cockerill III (1999). Comparison of susceptibility testing methods with mecA gene analysis for determining oxacillin (methicillin) resistance in clinical isolates of Staphylococcus aureus and coagulase-negative Staphylococcus spp. J. Clin. Microbiol. 37:2952-2961.
- Lowy, F. D (1998). Staphylococcus aureus infections. N. Engl. J. Med. 339:520-532.
- Martineau, F., F. J. Picard, P. H. Roy, M. Ouellette, and M. G. Bergeron (1998). Species-specific and ubiquitous-DNA-based assays for rapid identification of Staphylococcus aureus. J.Clin. Microbiol. 36:618-623.
- National Committee for Clinical Laboratory Standards (1993). Approved standard M2-A5. Performance standards for antimicrobial disk susceptibility tests. National Committee for Clinical Laboratory Standards, Villanova, Pa.
- National Committee for Clinical Laboratory Standards (1999). Performance standards for antimicrobial susceptibility testing. Ninth informational supplement M100-S9. National Committee for Clinical Laboratory Standards, Wayne, Pa.
- Panlilio, A. L., D. H. Culver, R. P. Gaynes, S. Banerjee, T. S. Henderson, J. S. Tolson, and W. J. Martone (1992). Methicillin-resistant Staphylococcus aureus in U. S. hospitals, 1975-1991. Infect. Control Hosp. Epidemiol. 13:582-586.
- Reischl, U., H.-J. Linde, M. Metz, B. Leppmeier, and N. Lehn (2000). Rapid identification of methicillin-resistant Staphylococcus aureus and simultaneous species confirmation using real-time fluorescence PCR. J. Clin. Microbiol. 38:2429-2433.
- Ribeiro, J., F. D. Vieira, T. King, J. B. D'Arezzo, and J. M. Boyce (1999). Misclassification of susceptible strains of Staphylococcus aureus as methicillin-resistant S. aureus by a rapid automated susceptibility testing system. J. Clin. Microbiol. 37:1619-1620.
- Ruane, P. J., M. A. Morgan, D. M. Citron, and M. E. Mulligan (1986). Failure of rapid agglutination methods to detect oxacillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 24:490-492.
- Tan, T. Y., S. Corden, R. Barnes, and B. Cookson (2001). Rapid identification of methicillin-resistant Staphylococcus aureus from positive blood cultures by real-time fluorescence PCR. J.Clin. Microbiol. 39:4529-4531.
- Tokue, Y., S. Shoji, K. Satoh, A. Watanabe, and M. Motomiya (1991). Detection of methicillin-resistant Staphylococcus aureus (MRSA) using polymerase chain reaction amplification. J. Exp.Med. 163:31-37.
- Tokue, Y., S. Shoji, K. Satoh, A. Watanabe, and M. Motomiya (1992). Comparison of a polymerase chain reaction assay and a conventional microbiolgic method for detection of methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother.36:6-9.
- Tomasz, A., H. B. Drugeon, H. M. de Lencastre, D. Jabes, L. McDougall, and J. Bille (1989). New mechanism for methicillin resistance in Staphylococcus aureus: clinical isolates that lack the PBP2a gene and contain normal penicillin-binding proteins with modified penicillin-binding capacity. Antimicrob. Agents Chemother. 33:1869-1874.
- Trees, D. L., and J. J. Iandolo (1988). Identification of a Staphylococcus aureus transposon (Tn4291) that carries the methicillin resistance gene(s). J. Bacteriol. 170:149-154.
- Ubukata, K., R. Nonoguchi, M. Matsuhashi, and M. Konno (1989). Expression and inducibility in Staphylococcus aureus of the mecA gene, which encodes a methicillin-resistant S. aureus-specific penicillin-binding protein. J. Bacteriol. 171:2882-2885.
- Ünal, S., J. Hoskins, J. E. Flokowitsch, C. Y. E. Wu, D. A. Preston, and P. L. Skatrud(1992). Detection of methicillin-resistant staphylococci by using the polymerase chain reaction. J. Clin.Microbiol. 30:1685-1691.
- Ünal, S., K. Werner, P. DeGirolami, F. Barsanti, and G. Eliopoulos (1994). Comparison of tests for detection of methicillin-resistant Staphylococcus aureus in a clinical microbiology laboratory. Antimicrob. Agents Chemother. 38:345-347.
- Voss, A., D. Milatovic, C. Wallrauch-Schwarz, V. T. Rosdahl, and I. Braveny (1994). Methicillin-resistant Staphylococcus aureus in Europe. Eur. J. Clin. Microbiol. Infect. Dis. 13:50-55.
- Wallet, F., M. Roussel-Delvallez, and R. J. Courcol (1996). Choice of a routine method for detecting methicillin-resistance in staphylococci. J. Antimicrob. Chemother.37:901-909.
- Waxman, D. J., and J. L. Strominger (1983). Penicillin-binding proteins and the mechanism of action of beta-lactam antibiotics. Annu. Rev. Biochem. 52:825-869.
- Weeres-Pothoff, G., C. E. M. Moolhuijzen, and G. P. A. Bongaerts (1987). Comparison of seven coagulase tests for identification of Staphylococcus aureus. Eur. J. Clin. Microbiol. 6:589-591.
- Wenzel, R. P., D. R. Reagan, J. S. Bertino, Jr., E. J. Baron, and K. Arias (1998). Methicillin-resistant Staphylococcus aureus outbreak: a consensus panel's definition and management guidelines. Am. J. Infect. Control 26:102-110.
- Wilkerson, M., S. McAllister, J. M. Miller, B. J. Heiter, and P. P. Bourbeau (1997). Comparison of five agglutination tests for identification of Staphylococcus aureus. J. Clin. Microbiol. 35:148-151.
- York, M. K., L. Gibbs, F. Chehab, and G. F. Brooks (1996). Comparison of PCR detection of mecA with standard susceptibility testing methods to determine resistance in coagulase-negative staphylococci. J. Clin. Microbiol. 34:249-253.



