Hematologic Toxicity of Temozolomide and Radiation in Glioblastoma Patients – Correlation with Clinicopathological Factors
Martina E. Becker-Schiebe1, 3, *, Martina Wetzel2, Fabian Wetzel1, Hans Christansen3, Wolfgang Hoffmann1
1Department of Radiotherapy and Radio-Oncology, Klinikum Braunschweig, Hannover Medical School, Braunschweig, Germany
2Department of Geriatrics, Klinikum Braunschweig, Hannover Medical School, Braunschweig, Germany
3Radiation Oncology, Hannover Medical School, Hannover, Germany
Abstract
Purpose: The aim of this analysis was to assess the hematological toxicity profile of glioblastoma patients undergoing radiation and temozolomide treatment (RCT). Methods: A total of 69 patients were evaluated retrospectively. A correlation analysis was undertaken to explore factors predisposing for acute hematological toxicity. Results: The overall incidence of any clinically acute hematologic toxicity was 42%. Severe anemia (i.e. grade 3/4), leucopenia and thromobocytopenia was diagnosed in 5.8%, 7.2% and 8.6% of the patients respectively. MGMT methylation was described in 23 (35%) cases. Female gender and MGMT methylation seemed to be risk factors for grade 4 toxicity (p< 0.05). The mean irradiated volume for patients with any degree of hematotoxicity was 238.4 ccm compared to 211.9 ccm for patients without any toxicity reactions. Conclusions: Our results confirmed that the female gender, radiation volume and MGMT methylation were factors associated with severe hematotoxicity. To our knowledge this is the first report suggesting the relevance of the MGMT methylation status of glioblastoma cells to treatment-related toxicity.
Keywords
Malignant Glioma, Temozolomide, Myelosuppression
Received: April 8, 2015 / Accepted: April 29, 2015 / Published online: May 15, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Temozolomide (TMZ) is an effective and widely used cytotoxic drug for glioblastoma treatment [1,2]. It is a prodrug of a specific alkylating agent (5-(3 methyltriazen-1-yl) imidazole-4-carboximide). Its antitumor effects are mediated by methylating guanine and adenine. This induces DNA damage in tumor cells which results in apoptosis and cytotoxicity [1].
In 2005 Stupp et al. [2] demonstrated the efficacy of a simultaneous treatment with irradiation and TMZ for malignant glioma patients. The randomized analysis confirmed improved median and 2-year overall survival when TMZ was applied concurrently with radiation (median survival 12.1 months in the RT group vs 14.6 months in the RT/TMZ-treated cohort). Survival in the combined treatment group continued to exceed that of radiation alone throughout the 5-year follow-up (p< 0.0001) [3]. For all clinical prognostic subgroups the efficiency of the Stupp regimen could be shown. Therefore postoperative radiation combined with TMZ and adjuvant maintenance of 6 cycles TMZ is now recommended as the standard treatment for glioblastoma patients. Several studies confirmed that patients with a methylated promoter of the DNA-repair enzyme O6-methylguanine-DNA methyltransferase (MGMT) show a significantly better response to treatment with TMZ with a median survival of 21-24 months [3-5]. This data supports the hypothesis that MGMT-promoter methylation may allow selection of patients, who will benefit most from a treatment with TMZ and radiotherapy [5].
Although TMZ has proven to be well tolerated by glioma patients non-hematologic grade 1/2 toxicities are common [1-3,6]. Nausea, vomiting and diarrhea are the main toxicities in patients undergoing TMZ+/-RT and are described in 37 to 44% of cases. Further adverse events include fatigue, headache, pruritus/itching, skin rashes as well as pulmonary infections in rare cases [6].
The triggering of hematotoxic side effects has been described in several reports. The cumulative incidence of thrombocytopenia and anemia according to the RTOG-CTC Score [7] is reported in 11-38% of cases [1,3,6,8]. Stupp et al. [3] demonstrated that the simultaneous combination treatment led to grade 3/4 myelotoxicity in 3-5% of patients during RT/TMZ and in 11% during adjuvant TMZ application. Especially pronounced hematological toxicities may be dose limiting with regard to the RT and TMZ dose administered and may impede completion of treatment protocols. Furthermore it may lead to a severe deterioration of the patients`quality of life. A case of a glioblastoma patient suffering from severe prolonged myelotoxicity prompted us to conduct a clinical review. As far as we know, up until now, factors effecting a predisposition for hematologic toxicity have not been clearly determined [3,6,9,11]. Therefore the aim of this retrospective evaluation was to assess the hematological toxicity profile of patients undergoing combined RCT and correlate it to clinical and histopathological parameters.
2. Material and Methods
69 patients, who had been diagnosed with a histologically documented glioblastoma multiforme and treated with surgery and postoperative RCT, were selected for this retrospective analysis.
For each patient the extent of surgery, i.e. the degree to which the tumor could be removed, was reported by the neurosurgeons. For CT based-radiotherapy planning, the gross target volume (GTV) was defined as the contrast-enhancing tumor visible on the preoperative MRI images. The planning target volume (PTV) included the GTV + 20.0-mm expansion plus edema visible on the T2-weighted images. A total dose of 54 to 59.4 Gy was delivered in fractions of 1.8 Gy daily, 5 times per week. Systemic treatment consisted of oral TMZ at a daily dose of 75 mg/m² given 7 days per week from the first to the last day of RT. 4 weeks later, patients received 4 to 6 cycles of adjuvant oral TMZ (150–200 mg/m²) for 5 days every 28 days. As recommended by Stupp et al [2] Pneumocystis-prophylaxis with either pentamidine or trimethoprim-sulfamethoxazole was routinely administered. Clinical and histopathological data was collected from medical records. The clinical parameters included age, gender, medication, karnofsky index and concomitant diseases. Furthermore, the moleculargenetic data, from the histopathological reports, concerning MGMT methylation and p53 mutations was evaluated retrospectively. Laboratory parameters such as a complete blood count, liver function tests, kidney function tests, tests detecting inflammation and coagulation parameters were checked twice weekly. The acute hematological reactions and signs of toxicity were classified according to the RTOG-CTC Toxicity-Score [7].
The mean values were expressed as a mean and/or a range of values. The statistical evaluation of the retrospective data has been done by descriptive statistical methods. The primary variable was the CTC score regarding myelotoxicity [7].
The different variables were evaluated by contingency tables. Associations between toxicity grades and the different clinical and histopathological parameters were calculated using chi-square tests. P-value <0.05 was considered statistically significant. Due to the small number of severe hematologic events multivariate analysis could not be performed.
Approval of the study (no. 2266-2014) was given by the ethics committee of the Hannover Medical School.
Table 1. Patients baseline of the study cohort (n=69).
| Characteristics | number of patients (%)/mean value |
| Gender | |
| Female | 25 (36%) |
| Male | 44 (64%) |
| Age | 59.7 y. (35-75y.) |
| <60 years | 30 (43%) |
| >60 years | 39 (57%) |
| Karnofsky Performance index | 79.2 % (40%-100%) |
| Extent of surgery | |
| Total | 63 (91%) |
| Subtotal | 6 (9%) |
| Irradiated Volume | 221.6 ccm (48-534.8) |
| Moleculargenetic parameters | 66 (96%) |
| MGMT Methylation | 23 (35%) |
| P53 Mutation | 26/31 pts. (83%) |
3. Results
69 consecutive patients with histologically proven glioblastoma multiforme were enrolled in this retrospective study. All patients were treated with combined RCT postoperatively. Patients receiving a total dose of 59.4 Gy and at least one course of TMZ chemotherapy were evaluated in this analysis only. All patients regularly concluded radiation treatment and all patients received prophylactic steroids during RCT. Antiepileptic drugs were administered in 84% of patients. Adjuvant TMZ was given in 46 patients over a period of 4 to 6 cycles. In 23 patients the courses of TMZ could not be completed as intended due to a deterioration of hematologic parameters, deterioration of general health and /or patients’ preference.
Table 2. Hematologic findings during therapy.
| Hematologic findings | Nadir (mean value)[range] | mean value after radio-chemotherapy [range] |
| Leucocytes (100/µl) | 4.7 [0.1-12.0] | 5.1 [0.1-11] |
| Thrombocytes (1000/ µl) | 119 [5-289] | 178 [15-495] |
| Hemoglobin (g/dl) | 11.9 [6.0-12.9] | 12.4 [6.0-14.9] |
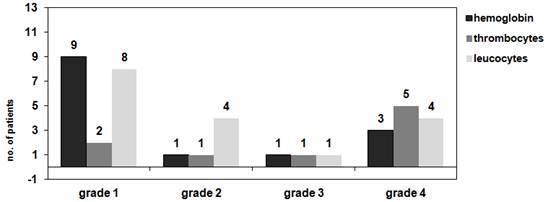
Figure 1. Maximum toxicity according to RTOG criteria (acute radiation morbidity scoring criteria) [7].
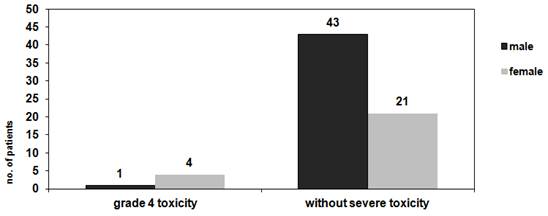
Figure 2a. Correlation of gender and severe hematologic toxicity grade 4, chi-square test p=0.03.
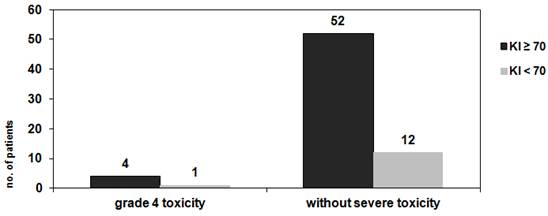
Figure 2b. Correlation of performance status (KI) ≥ and severe hematologic toxicity grade 4, chi-square test p=0.94.
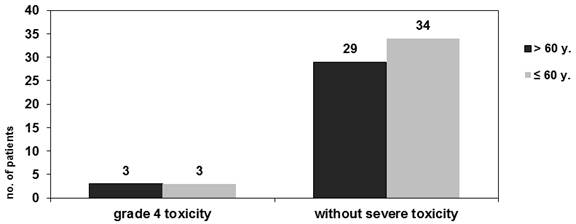
Figure 2c. Correlation of age and severe hematologic toxicity grade 4, chi-square test p=0.85.
Out of the 69 patients 44 were male and 25 were female. The overall mean age of this series was 59.7 years. Most patients underwent gross tumor resection (63/69 (91%)). Before treatment, baseline blood cell counts and laboratory findings for liver function were within the normal range. Medical records revealed tumorigenic data for 96% of patients. MGMT methylation was positive in 23 (35%) of cases, p53 positive tumors were identified in 26/31 patients. Further pretreatment characteristics are listed in table 1. The overall incidence of any clinically acute hematologic toxicity was 42% (29/69 pts.). Severe toxicity (grade 3/4) was seen in 7/69 (10%) cases with the most common high grade toxicity being thrombocytopenia grade 4 in 5/69 cases. High grade 3/4 anemia, leucopenia and thromobocytopenia was diagnosed in 5.8%, 7.2% and 8.6% respectively. The nadir and post therapeutic values of the hematologic parameters are described in table 2. Maximum toxicity according to RTOG common toxicity criteria is shown in figure 1.
5 patients suffered from severe pancytopenia grade 4 and needed blood and platelet transfusions as well as growth factor support. 1 patient developed a severely inhibited bone marrow function lasting more than 3 months. Bone marrow biopsy showed absence of megakaryocytes and myeloid precursors. This patient died due to pneumonia 4.5 months after primary therapy.
Factors predisposing for acute hematologic side effects were examined by correlation analysis (chi square test; figures 2 a, b, c; 3). Female gender and MGMT methylation could be identified as risk factors for severe toxicity grade 4 (p< 0.05). Analysis of performance status (KI) and age did not reveal any significant differences for toxicity rates. For all patients radiotherapy treatment planning was reviewed. Mean treatment volume was 221.6 ccm (48-534.8 ccm). Correlations between radiation volume and myelotoxicity (maximum grade) are depicted in figure 4.
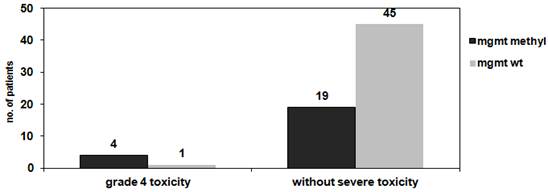
Figure 3. Correlation of MGMT methylation of tumor DNA and severe hematologic toxicity grade 4, chi-square test p=0.02.
The mean irradiated volume for patients suffering from grade 1-4 toxicity was 238.4ccm compared to 211.9 ccm for patients without any hematologic reactions.
Further associations with clinical factors could not be observed.
4. Discussion
Glioblastomas account for 60 to 70% of all gliomas and are the most frequent primary brain tumors in adults.
In general the incidence of malignant gliomas for males is higher than for females (6 % compared to 4%). Likewise, 65% of our glioblastoma patients were male. Further patient characteristics such as the mean age of 59.7 y. (35-75y.) and general performance status are comparable with other data reported in the literature such as the described peak incidence of the disease in the fifth and sixth decade of life [8]. Previous studies have identified numerous genetic alterations in glioblastomas including deletions of negative regulatory elements and oncogene amplification [9,10]. p53 mutations occur in approximately one third of glioblastomas. In addition more than 30-35% of malignant gliomas have inactivated MGMT-genes. Information of p53 mutations was available for 31 patients, it is noteworthy that we observed a much higher incidence of 83% mutated tumors in our series while MGMT methylation was seen in 35% of glioblastomas.
After the results of the EORTC-NCIC [2] regimen and following trials over the last decade concurrent RT and TMZ followed by at least 6 monthly adjuvant TMZ cycles became the standard of care for newly diagnosed glioblastomas.
The improved efficacy and favourable toxicity profile of TMZ led to its usage for anaplastic and oligodendrogliomas as well or as a salvage therapy in dose intensified schedules [11,12].
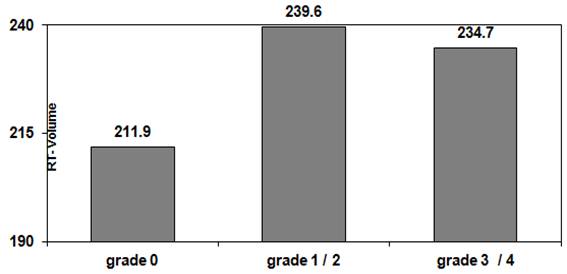
Figure 4. Correlation of radiation treatment volume (ccm, mean value) and myelotoxicity (maximum grade). Treatment volume for patients suffering from grade 1-4 toxicity: 238.4 ccm.Treatment volume for patients without toxicity 211.9 ccm
TMZ exerts its antitumor effects by methylating guanine and inducing apoptosis. While TMZ is considered to be a safe cytotoxic drug, severe myelotoxic side effects may occur. Bone marrow cells are particularly sensitive to TMZ treatment due to lower MGMT levels than in glioma tissues, resulting in myelosuppression.
The overall incidence of grade 3/4 myelotoxicity was 11 % in the entire EORTC study [3]. Some differences concerning the incidence of side effects are published in the literature. Recent case studies reported about a clinically significant toxicity with severe myelosuppression or leukemogenic potential of TMZ [13], which necessitates aggressive supportive care and interruption or termination of combined treatment. Kesari et al. [14] found leukopenia in 47.7% and neutropenia in 34.1% of TMZ treated glioma patients.
In our retrospective analysis the overall incidence of any degree of clinically acute hematologic toxicity was 42%, which is comparable to the data of a series of 300 glioblastomas with hematologic side effects in 42 % of patients [15]. However, other studies reported about up to 82% of patients suffering from one or more hematologic adverse effects; especially severe leucopenia was seen in 32% of patients [16].
We observed grade 3/4 anemia, leucopenia and thromobocytopenia in 5.8%, 7.2% and 8.6% of cases respectively. In 2013 Gupta et al. [17] published a review of randomized trials evaluating severe TMZ induced toxicities. According to this data the overall incidence of grade 3/4 thrombocytopenia and neutropenia was 5 to 15.5% using the standard dose-schedule of TMZ in the Stupp protocol. The rates of severe lymphopenia were more variable and reached up to 40%. Long lasting immunosuppression following combined RT/TMZ treatment as risk factor for opportunistic infections is described in several studies [18]; but the cause of death is related to infections in 2.5% only. As shown on table 2 mean values of blood counts (nadir and post therapeutic levels) demonstrate, that the majority of patients did recover from any hematological side effects. In our cohort one female patient developed a severely inhibited bone marrow function lasting more than 3 months and died due to pneumonia 4.5 months after termination of primary therapy. We found comparable cases in the literature presenting with prolonged pancytopenia, aplastic anemia and secondary hematological malignancies [19]. Interestingly in all of these cases, patients were younger women (< 60 y.), without any prior treatment, who had been administered TMZ therapy for 4 to 5 weeks only. We also observed a significant correlation of grade 3/4 myelotoxicity with the female gender for our patient group. The susceptibility of the female gender to more pronounced side effects may be caused by pharmacokinetic and pharmacodynamic reasons. Different activities of hepatic enzymes, drug transporters and renal excretion of temozolomide drug metabolism in female patients are being discussed [20].
Some studies have tried to identify factors associated with an increased risk of acute temozolomide-induced toxicity. In the largest analysis of 680 malignant glioma patients a clinical risk formula for myelotoxicity was developed retrospectively which confirmed a higher risk of hematotoxicity for women [21]. For male patients risk factors were body surface area > 2m2and missing of steroid or bowel medication, while in women enhanced creatinin levels, reduced platelet counts before therapy and application of analgetics were predisposing parameters.
Additional risk factors for thrombocytopenia include trimethoprim-sulfamethoxazole medication for pneumonia-prophylaxis or anticonvulsants. Since all patients received prophylactic steroids during RCT and antiepileptic drugs were applied in 84% of our patients, we could not identify such a correlation. In some reports elderly patients have a higher rate of TMZ induced pancytopenia, but analysis of age revealed contradictory results [17,21,22]. In our patient cohort no meaningful differences in toxicities with regard to further clinical characteristics like age or performance status were found.
The concurrent application of cranial irradiation may also have a negative impact on blood cell counts. A trial including 101 high-grade astrocytoma patients demonstrated an increase in hematologic toxicity in the concurrent regimen compared to sequential RCT. It is postulated, that cranial irradiation fields deliver a myelotoxic and lymphotoxic dose to the bone marrow and circulating stem cells, which augmentates the hematologic toxicity of concurrent systemic treatment [23]. The impact of radiation volume was emphasized by our analysis with a mean radiation volume of 238.4 ccm for patients suffering from grade 1-4 toxicity compared to 211,9 ccm for patients without any side-effects.
The prognostic value of MGMT promoter-methylation for glioblastoma patients was confirmed by several trials [3-5]. Tumors without promoter methylation and consecutively high levels of MGMT are known to be associated with TMZ resistance, which supports the important impact of gene expression on treatment efficacy. Recent trials [19,21,22,24] correlate TMZ induced side-effects with genetic parameters of peripheral blood cells. In general bone marrow precursor cells express lower MGMT levels in comparison to other tissues [1]. MGMT expression may vary individually resulting in an increased cytotoxicity of alkylating agents. For TMZ-treated melanoma patients an association between low MGMT levels in mononuclear blood cells and thrombopenia/ neutropenia could be observed [24]. In the risk stratification of a subset of 187 glioblastoma patients Armstrong et al [21] defined genetic single nucleotide polymorphisms of MGMT, Glutathione S-transferase pi1 and NADPH dehydrogenase quinone-1 from peripheral blood cells as predisposing hematotoxic factors. MGMT promoter methylation of tumor-DNA was proven for approximately one third of our patients. Since we evaluated our patients retrospectively, we could not determine genetic polymorphism of paired blood samples. However we found a significant correlation between MGMT status of tumor cells and hematological side effects. Out of the five patients suffering from grade 4 toxicity, MGMT methylation was identified in 4 cases. In the relevant literature only one comparable case has been reported which describes MGMT promoter methylation of tumor DNA but unmethylated promoters in peripheral blood cells in a patient suffering from prolonged myelotoxicity following TMZ treatment [19]. Actually, a statistically significant association (p<0.05) between target gene mRNA expression in tumour tissue and blood cells was reported. This was found in particular for ERCC and MGMT in non small cell lung cancer and head and neck cancer patients [25]. Nevertheless, the relationship between the extent of MGMT depletion in blood and glioma tumor tissue and hematologic toxicities needs to be further validated.
In conclusion hematologic toxicity rates of our patient cohort were in the expected range of 5-10% known from randomized trials. Despite the limited power of a retrospective analysis we could confirm the female gender and radiation volume as factors associated with severe hematologic toxicity rates. The occurrence of hematologic reactions was associated with the size of radiation volume receiving total doses between 54 and 59.4 Gy. In addition to this, to our knowledge this is the first report suggesting the relevance of the MGMT status of glioblastoma cells to treatment-related toxicity. However the possible relationship between tumorigenic factors and severe side-effects has to be proven in larger trials.
References
- Sengupta S, Marrinan J, Frishman C, Sampath P. Impact of temozolomide on immune response during malignant glioma chemotherapy. Clin Dev Immunol. 2012; R, Hegi ME, Mason WP, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009; 10: 459–66.
- Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al.Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. European Organisation for Research and Treatment of Cancer Brain Tumor and Radiotherapy Groups; National Cancer Institute of Canada Clinical Trials Group. N Engl J Med 2005; 352(10): 987-96.
- Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 2009; 10: 459–66.
- Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, et al. MGMT gene silencing and benefit from temozolomide in glioblastoma. N Eng J Med 2005; 352(10): 997–1003.
- Wick W, Weller M, van den Bent M, Sanson M, Weiler M, von Deimling A, et al.MGMT testing--the challenges for biomarker-based glioma treatment. Nat Rev Neurol 2014; 10(7): 372-85.
- Bae SH, Park MJ, Lee MM, Kim TM, Lee SH, Cho SY, et al. Toxicity profile of temozolomide in the treatment of 300 malignant glioma patients in Korea. J Korean Med Sci 2014; 29(7): 980-84.
- CommonToxicityCriteria.2014.[http://www.rtog.org/ResearchAssociates/ AdverseEventReporting/CooperativeGroupCommonToxicityCriteria.aspx].
- Chakrabarti I, Cockburn M, Cozen W, Wang YP, Preston-Martin S. A population based description of glioblastoma multiforme in Los Angeles County, 1974-1999. Cancer 1999; 104: 2798-2806.
- Schiebe M, Ohneseit P, Hoffmann W, Meyermann R, Rodemann HP, Bamberg M. Loss of heterozygosity at 11p15 and p53 alterations in malignant gliomas. J Cancer Res Clin Oncol. 2001; 127(5): 325-328.
- Schiebe M, Ohneseit P, Hoffmann W, Meyermann R, Rodemann HP, Bamberg M.Analysis of mdm2 and p53 gene alterations in glioblastomas and its correlation with clinical factors. J Neurooncol 2000; 49(3): 197-203.
- Macdonald DR. Temozolomide for recurrent high grade glioma. Sem in Oncol 2001; 28: 3-12.
- Wick W, Hartmann C, Engel C, Stoffels M, Felsberg J, Stockhammer F, et al.NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. Clin Oncol 2009; 27(35): 5874-80.
- Momota H, Narita Y, Miyakita Y, Shibui S. Secondary hematological malignancies associated with temozolomide in patients with glioma. Neuro Oncol 2013; 15: 1445-1450.
- Kesari S, Schiff D, Henson JW, Muzikansky A, Gigas DC, Doherty L, et al. Phase II study of temozolomide, thalidomide, and celecoxib for newly diagnosed glioblastoma in adults. Neuro Oncol 2008;10(3): 300.
- Bae SH, Park MJ, Lee MM, Kim TM, Lee SH, Cho SY, et al. Toxicity Profile of Temozolomide in the Treatment of 300 Malignant Glioma Patients in Korea. J Korean Med Sci 2014; 29: 980-984.
- Ishikawa E, Yamamoto T, Sakamoto N, Nakai K, Akutsu H, Tsuboi K, et al. Low peripheral lymphocyte count before focal radiotherapy plus concomitant temozolomide predicts severe lymphopenia during malignant glioma treatment. Neurol Med Chir (Tokyo) 2010; 50(8):638-44.
- Gupta T, Mohanty S, Moiyadi A, Jalali R. Factors predicting temozolomide induced clinically significant acute hematologic toxicity in patients with high-grade gliomas: a clinical audit. Clin Neurol Neurosurg 2013; 115(9): 1814-19.
- Grossman SA, Ye X, Lesser G, Sloan A, Carraway H, Desideri S, Piantadosi S; NABTT CNS Consortium. Immunosuppression in patients with high-grade gliomas treated with radiation and temozolomide. Clin Cancer Res 2011; 17(16): 5473-80.
- Nagane M, Nozue K, Shimizu S, Waha A, Miyazaki H, Kurita H, et al. Prolonged and severe thrombocytopenia with pancytopenia induced by radiation-combined temozolomide therapy in a patient with newly diagnosed glioblastoma--analysis of O6-methylguanine-DNA methyltransferase status. J Neurooncol 2009; 92(2): 227-32.
- Anderson G. Gender differences in pharmacological response. Int Rev Neurobiol 2008; 83: 1-10.
- Armstrong TS, Cao Y, Scheurer ME, Vera-Bolaños E, Manning R, Okcu MF, et al. Risk analysis of severe myelotoxicity with temozolomide: the effects of clinical and genetic factors. Neuro Oncol 2009; 11(6): 825-32.
- Lombardi G, Rumiato E, Bertorelle R, Saggioro D, Farina P, Della Puppa A, et al. Clinical and Genetic Factors Associated With Severe Hematological Toxicity in Glioblastoma Patients During Radiation Plus Temozolomide Treatment: A Prospective Study. Am J Clin Oncol 2013 Sep 21. [Epub ahead of print]
- Kleinberg L, Grossman SA, Piantadosi S, Zeltzman M, Wharam M. The effects of sequential versus concurrent chemotherapy and radiotherapy on survival and toxicity in patients with newly diagnosed high-grade astrocytoma. Int J Radiat Oncol Biol Phys 1999; 44(3): 535-43.
- Sabharwal A, Waters R, Danson S, Clamp A, Lorigan P, Thatcher N, et al. Predicting the myelotoxicity of chemotherapy: the use of pretreatment O6-methylguanine-DNA methyltransferase determination in peripheral blood mononuclear cells. Melanoma Res 2011; 21(6): 502-8.
- Schena M, Guarrera S, Buffoni L, Salvadori A, Voglino F, Allione A, et al. DNA repair gene expression level in peripheral blood and tumor tissue from non-small cell lung cancer and head and neck squamous cell cancer patients. DNA Repair (Amst) 2012; 11(4): 374-80.



