Emerging Role of Vascular Plug for Endovascular Management of Pulmonary Ateriovenous Malformation
Pankaj Sharma1, *, Thomas Pfammatter2
1Department of Radiodiagnosis, Delhi State Cancer Institutes, Delhi, India
2Institute of Diagnostic and Interventional Radiology, University Hospital Zurich, Rämistrasse, Switzerland
Abstract
Pulmonary arteriovenous malformations (PAVM) are rare vascular malformation, having direct communication between a pulmonary artery and pulmonary vein, bypassing intervening capillary bed. Traditionally, minimally invasive, endovascular Interventional treatment using coils has been the treatment of choice for PAVM. Our case report highlights emerging role of vascular plug in treating PAVM. Vascular plug have advantage of complete cessation of blood flow to aneurysmal sac along with decreased chances of recurrence or persistence of PAVM.
Keywords
Malformation, Aneurysmal, Embolization, Transcatheter
Received: March 29, 2015 / Accepted: April 20, 2015 / Published online: May 11, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Vascular plug are self expandable device indicated for arterial and venous embolisation in the peripheral vasculature. But now, vascular plug is increasingly been used for occluding Pulmonary arteriovenous malformations (PAVM)1,2,3.
PAVM can occur as isolated entity or in association with hereditary hemorrhagic telangiectasia (HHT)4. PAVM have increased risk of morbidity5,6 related to stroke, cerebral and systemic abscess, pulmonary haemorrhage and cause significant right to left shunt with resulting cyanosis, heart failure and serious neurological events related to paradoxical embolisation. Percutaneous transcatheter coil embolisation has been mainstay of management for last few years with high success rate. Our case report highlights role of vascular plug for managing PAVM.
2. Case Report
A 54 year old male presented with 3 week history of headaches and an episode of loss of consciousness. Head Computed Tomography (CT) showed a mass in his parietal lobe, which was proven to be an abscess at transcranial surgical drainage. His blood culture report revealed Streptococcus Viridans. As to his past history, he reported recurrent epistaxis events. His brother had undergone resection of a PAVM accompanied by a stroke at 46 years of age.
Chest CT of patient revealed Solitary PAVM in posterobasal segment right lower lobe fed by an enlarged 6 mm diameter subsegmental branch of right pulmonary artery. Under aseptic conditions, following local anaesthesia and intravenous heparin (5000 IU, unfractionated), venous access was done from right femoral vein. Pulmonary Angiography was done first using pigtail catheter (APC®,7Fr, Cook Inc, Bloomingdale, IN/USA). This Digital Subtraction Angiogram (DSA) confirmed the CTA-finding. Thereafter the pigtail catheter was exchanged for a 90 cm long introducer sheath (Flexor®,6Fr,CookInc, Bloomingdale, IN/USA). With the help of a coaxially introduced angled catheter (JB1®, 5Fr, Cook Inc, Bloomingdale, IN/USA) and a 0.035" Terumo-guidewire, the 6Fr sheath was advanced into the subsegmental pulmonary arterial branch to deploy anAmplatzer Vascular Plug 4® (St Jude Medical, St. Paul, MN/USA) of 8 mm diameter, after ensuring correct location just proximal to aneurysmal sac and after unscrewing delivery catheter. Post embolization angiogram revealed complete occlusion of PAVM. Post-embolization period was uneventful and patient was discharged in stable condition.
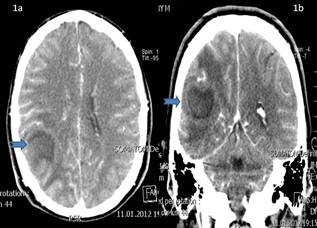
Fig 1a and 1b. Axial and coronal CT Head images showing right parietal lobe abscess with perilesional cerebral edema.
3. Discussion
PAVM occurs when there is direct communication between a pulmonary artery and a pulmonary vein, bypassing the capillary bed. An intervening aneurysmal sac or tangle of dilated tortuous vascular channels usually is present. PAVM are usually congenital, sometimes associated with HHT, but acquired PAVM are also possible. White RI Jretal7, classified PAVM into two categories: simple and complex. Simple PAVM have a single segmental feeding artery whereas complex PAVM have two or more segmental arteries supplying the malformation. Our patient had single segmental feeding artery, hence categorized as simple PAVM.
First transcatheterembolisation of a PAVM was done by Portsmann W in 19778. Minimally invasive endovascular treatment is now embolisation method of choice for symptomatic PAVM. PAVM has been embolised intra-arterially using various embolisation materials5,9 like pushable coils, detachable coils or detachable balloons. But now various authors like Trerotola S et al10, are advocating Amplatzer Vascular Plug alone and/or in combination with coils to treat symptomatic PAVM.
Vascular occluders have been used successfully to close atrial septal defects, ventricular septal defects and patent foramen ovale for long time11. Vascular plug is a self expanding, multilayerednitinol wire mesh and has advantage of high radial strength, ability to control placement of the device, better trackability and flexibility during placement around bends and curves, and rapid occlusion and haemostasis with a single device. Abdel Aal AK et al12, concluded mean occlusion time of Vascular plug to be 3 minutes 20 seconds (ranging from 1 minute 49 seconds to 5 minutes 16 seconds).

Fig 2. Axial CT Chest image showing single PAVM in posterobasal segment right lower lobe lung parenchyma. There is single feeding artery (arrow) and single draining vein (arrowhead).
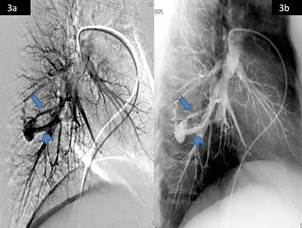
Fig 3a and 3b. DSA images showing PAVM in posterobasal segment right lower lobe lung parenchyma with single feeding artery (arrow) and single draining vein (arrowhead).
Percutaneous transcatheter embolisation with coils has been the mainstay of management of PAVM with a high success rate. Complications13,14 can occur with transcatheter embolisation using coils like paradoxical coil embolisation and recurrence. Persistence of flow in aneurysmal sac with coil surface acting as nidus for small clots to form, there is always chance of systemic embolisation with devastating complications related to it. Recurrence is secondary to recanalization of occluded vessels or interval growth of accessory vessels. Moreover, even for small size feeding arteries, atleast two to three coils are needed for embolisation, which adds substantially to cost, procedure time and associated risks. Also, placement of first and last coil is most difficult part in entire procedure.
Only single Vascular plug is needed for completely occluding feeding artery in PAVM. Moreover, complete vascular supply to aneurysmal sac is cut off using Vascular plug with less probability of paradoxical embolisation. Vascular plug can be retrieved back if placement is not satisfactory and Vascular plug would not be deployed until unscrewed, usually with three counterclockwise turns of the delivery catheter. We had to deploy only single Amplatzer Vascular plug 4 of size 8 x 13.5 mm in our patient with simple PAVM. Occlusion time was less than 4 minutes and patient had no significant post-procedural complication.
Tapping CR et al15, reported results of long term follow up of PAVM treated with vascular plug. Out of 19 PAVM, treated with Amplatzer Vascular Plug and Amplatzer Vascular Plug II, one PAVM had re-canalization 36 months after procedure with annual event rate of 0.03 recanalization per year. One patient had immediate complication of chest pain (likely due to pleurisy) and this resolved within 24 hours with simple analgesia.
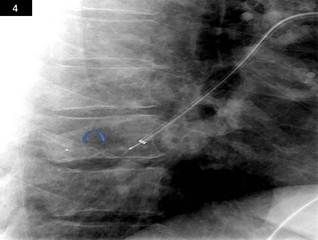
Fig 4. DSA images showing Amplatzer vascular plug 4 (curved arrow) placement in feeding artery proximal to aneurysmal sac.
Our case report highlights role of Vascular plug for endovascular management of PAVM. Moreover, Vascular plug would be cost effective as compared to use of multiple coils for embolisation and would have less chance of paradoxical embolisation and recurrence. However, further long term follow up comparison studies are needed with other treatment modalities to establish firmly role of Vascular plug for treating symptomatic PAVM.
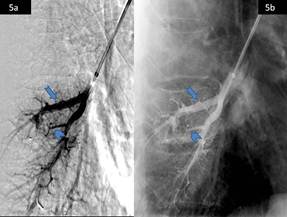
Fig 5a and 5b. Post embolization DSA images showing complete cessation of vascular flow to PAVM in posterobasal segment right lower lobe lung parenchyma. Also note dilated feeding artery (arrow) and small calibre draining vein (arrowhead).
References
- Ferro C, Rossi UG, Bovio G, et al.Percutaneous transcatheter embolization of a large pulmonary arteriovenousfistula with an Amplatzer vascular plug. CardiovascInterventRadiol 2007; 30: 328-331.
- Beck A, Dagan T, Matitiau A, et al.Transcatheter closure of pulmonary arteriovenous malformations with Amplatzer devices. Catheter CardiovascInterv 2006; 67: 932-937.
- Cil B, Canyigit M, Ozkan OS, et al.Bilateral multiple pulmonary arteriovenous malformations: endovascular treatment with the Amplatzer vascular plug. J VascIntervRadiol 2006; 17: 141-145.
- Gossage JR, Kanj G. Pulmonary arteriovenous malformations: a state of the art review. Am J RespirCrit Care Med 1998; 158: 643-661.
- Lee BB, Do YS, Yakes W, et al. Management of arteriovenous malformations: a multidisciplinary approach. J VascSurg 2004; 39: 590-600.
- Moussouttas M, Fayed P, Rosenblatt M, et al.Pulmonary arteriovenousmalformatio: cerebral ischemia and neurological manifestations. Neurology 2000; 55: 959-964.
- White RI Jr, PollakJS, Wirth JA. Pulmonary arteriovenous malformations: diagnosis and transcatheterembolotherapy. J Vas IntervRadiol 1996; 7: 787-804.
- Portsmann W. Therapeutic embolization of arterio-venous pulmonary fistula by catheter technique. In: Kelop O, ed. Current concepts in Pediatric Radiology. Berlin: Springer; 1977: 23-31.
- Pollack JS, Saluja S, Thabet A, et al. Clinical and anatomical outcomes after embolotherapy of pulmonary arteriovenous malformations. J VascIntervRadiol 2006; 17: 35-44.
- Trerotola S, Pyeritz RE. Does use of coils in addition to Amplatzer Vascular Plugs prevent recanalization? Am J Roentgenol 2010; 195: 766-771.
- Ferro C, Petrocelli F, Rossi UG, et al.Vascular percutaneous transcatheter embolization with a new device: Amplatzer vascular plug. Radiol Med 2007; 112: 239-251.
- Abdel Aal AK, Hamed MF, BioscaRF, et al. Occlusion time for Amplatzer vascular plug in the management of pulmonary arteriovenous malformations. Am J Roentgenol 2009; 192(3): 793-799.
- Magger JJ, Overtoom TT, Blauw H, et al.Embolotherapy of pulmonary arteriovenous malformations: long term results in 112 patients. J VascIntervRadiol 2004; 15: 451-456.
- Milic A, Chan RP, Cohen JH, et al. Reperfusion of pulmonary arteriovenous malformations after embolotherapy. J VascIntervRadiol 2005; 16: 1675-1683.
- Tapping CR, Ettles DF, Robinson GJ. Long-term follow-up of treatment of Pulmonary Arteriovenous Malformations with Amplatzer Vascular Plug and Amplatzer Vascular Plug II devices. J VascIntervRadiol 2011; 22: 1740-1746.



