Primary Endobronchial Carcinoid Tumour: Case Report and Review of Literature
Archana Kumari1, *, Pankaj Sharma1, Gargi Tikku2, Kriti Malhotra1
1Department of Radiodiagnosis, Delhi State Cancer Institutes, Dilshad Garden, Delhi, India
2Department of Pathology, Delhi State Cancer Institutes, Dilshad Garden, Delhi, India
Abstract
Bronchial carcinoid tumours are carcinoid tumours primarily occurring in relation to a bronchus. They are uncommon comprising only 1-2% of all lung tumours. This is case of 28 year old man with persistent wheezing, cough with expectoration, fever and chest pain on left side, for four to five months. All routine investigations were within normal limits. Chest roentgenogram demonstrated partial volume loss on left side. Contrast Enhanced Computed Tomography (CT) of thorax revealed lobulated intraluminal mass lesion completely occluding left main bronchus; approximately 1 cm from carina. On arterial phase of the scan, the lesion showed intense homogenous enhancement characteristic of carcinoid tumours. In addition, CT scan showed mediastinal lymphadenopathy and partial left lung collapse with multiple air filled cavities. Subsequent bronchoscopy revealed reddish lobulated tumour of let main bronchus. Bronchoscopy alveolar lavage (BAL) showed no abnormal cells. On Bronchoscopy biopsy, it came out to be typical carcinoid tumour of grade 1 type. Patient was initially unsuccessfully treated for bronchial asthma, as intrabronchial mass was not suspected. Further investigations revealed intrabronchial mass lesion completely occluding left main bronchus. This intrabronchial mass in our case was carcinoid tumour. Thus, due to lack of characteristic symptoms, diagnosis of intrabronchial carcinoid is usually delayed. We advocate that patient with refractory respiratory symptoms should undergo comprehensive Radiological and Pathological investigations for accurate and early diagnosis.
Keywords
Endobronchial Carcinoids, Computed Tomography, Bronchoscopy, Radiotherapy
Received: March 21, 2015 / Accepted: April 15, 2015 / Published online: May 5, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Bronchial Carcinoids are uncommon, slow growing, low grade malignant neoplasm comprising 1-2% of all primary lung cancers; although it is the commonest tumour of tracheobronchial tree. This tumour usually presents with hemoptysis. However sometimes presentation is somewhat unusual in form of refractory wheezing, breathlessness, cough and chest pain. Central bronchial carcinoids are more common than the peripheral type and are seen as endobronchial nodule or hilar/perihilar mass closely related to the adjacent bronchus. Mostly the clinicians miss the diagnosis and patient undergoes treatment for bronchial asthma for long time, before the actual diagnosis is established.
Early diagnosis is extremely important as patients benefit from surgical resection and prognosis is very good. We present a case of bronchial carcinoid initially misdiagnosed and treated for asthma prior to the final diagnosis. Patient underwent Chest Roentgenogram, CECT (Contrast Enhanced Computed Tomography) Thorax, PET-CT (Positron Emission Tomography-Computed Tomography) and Bronchoscopy biopsy to confirm the diagnosis.
2. Case Report
A 28 years old man presented in Oncology Out Patient Department (OPD) with persistent wheezing, left sided chest pain, fever and cough with expectoration, since last four to five months. There was no history of hemoptysis. Patient reported no other complaints for disease in his medical history. His family history was clinically insignificant. He was habituated Gutka chewer. His symptoms were not relieved with inhaled B2 agonist, steroid and antibiotics. On physical examination, wheeze was present. All routine laboratory investigations were unremarkable.
Chest roentgenogram revealed partial volume loss on left side. Contrast Enhanced Computed Tomography (CT) of thorax revealed lobulated intraluminal mass lesion completely occluding left main bronchus; approximately 1 cm from carina. On arterial phase of the scan, the lesion showed intense homogenous enhancement characteristic of carcinoid tumours. In addition, CT scan showed mediastinal lymphadenopathy and partial left lung collapse with multiple air filled cavities. Bronchoscopy revealed reddish lobulated tumour of let main bronchus. Bronchoscopy alveolar lavage (BAL) showed no abnormal cells. Patient underwent bronchoscopic removal of tumour. Biopsy revealed a very bland and monotonous population of tumor cells arranged in serpiginous cords and ribbons. The nuclei had a characteristic salt and pepper chromatin pattern. No increased mitotic activity/necrosis was seen. On Immunohistochemistry, tumor cells expressed CK, chromogranin and synaptophysin with a Ki-67 proliferation index of <1%. They were immunonegative for TTF-1. Thus a diagnosis of Grade 1 neuroendocrine carcinoma (NEC) was made.
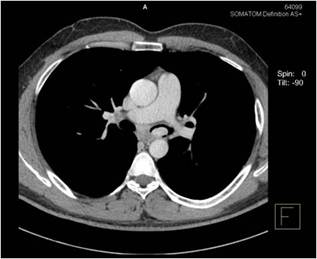
Figure 1(a). Contrast enhanced axial CT image show homogenously enhancing left main bronchus tumour.
Post tumour excision, CT of thorax showed a residual lobulated intraluminal mass lesion of approximately 1.5 X 2.2cm involving left main bronchus, almost 1 cm from carina. Lesion was partially occluding the left main bronchus. Lesion showed intense homogeneous enhancement in arterial phase CT thorax. Hilar and mediastinal lymph nodes were not enlarged. In Virtual Bronchoscopy, partially occluded left main bronchus tumour could be observed. Fluoro- deoxyglucose Positron Emission Tomography (FDG PET-CT) revealed intraluminal soft tissue mass with increased uptake (SUV max of 4.6) in left main bronchus and subcarinal lymph node metastasis. Patient is being planned further for Radiotherapy treatment.
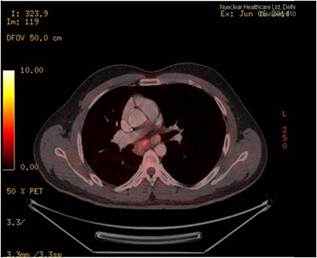
Figure 1(b). PET CT image demonstrates increase FDG uptake by the tumour with subcarinal lymph node metastasis.
3. Discussion
Bronchial carcinoid tumors are classified as neuroendocrine neoplasms of the lung. They arise in the bronchial and bronchiolar epithelium and may derive from existing Kulchitsky cells, neuroepithelial bodies, or pluripotential bronchial epithelial stem cells (1,2).
Carcinoids occur most frequently in the gastrointestinal tract (90% of cases). They can also occur in the lung, thymus, biliary tract, and ovary. Bronchial carcinoids are uncommon, comprising only 1%–2% of all lung tumors (3,4). Previously they were termed as bronchial adenoma, but now it is considered inaccurate because the tumors are neither uniformly glandular in origin nor consistently benign (5). Carcinoid tumours are classified as typical or atypical according to histopathological criteria. The division has a strict extrapolation to survival rates. In cases of typical pulmonary carcinoids, 5 years survival rate is over 90%. In atypical pulmonary carcinoid; it is within the range of 40-60% (6).
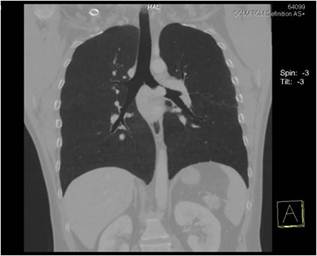
Figure 2(a). Minimal Intensity Projection coronal image shows the enhancing left main bronchus tumour.
Bronchial carcinoids affect male and female patients equally over a wide age range, with a mean patient age of 45 years. In general, patients with bronchial carcinoids are younger than those with common primary pulmonary neoplasms such as bronchogenic carcinoma. There is no association with cigarette smoking or the inhalation of other carcinogens. Presenting symptoms include cough, fever, expectoration, wheezing, hemoptysis, chest pain and symptoms simulating asthma (7). Due to lack of characteristic symptoms, diagnosis of pulmonary carcinoid is delayed and patient often misdiagnosed with asthma or chronic obstructive pulmonary disease. Similarly in our case, patient was having persistent wheezing, cough with expectorations and left sided chest pain and was being unsuccessfully treated by inhaled B2 agonist, steroid and antibiotics.

Figure 2(b). Coronal CECT shows the enhancing intrabronchial tumour.
Rarely, patients may exhibit syndromes related to ectopic hormone production by the tumor, specifically, ACTH. Cushing syndrome is seen in only about 2% of bronchial carcinoids (7, 8). Metastases occur in 15% of bronchial carcinoids and are typically located in the liver, bone, adrenal glands and brain (9). In our case there was no history of symptoms due to ectopic hormone production or metastases.
As the majority of pulmonary carcinoids (70%) are located in main or lobar bronchi (10), they are within the reach of a bronchoscope. In our case also intrabronchial tumour was seen in the left main bronchus. On bronchoscopy, they appear as smooth, cherry red, polypoid, endobronchial nodules. The histologic diagnosis is made with bronchoscopic biopsy. Histological diagnosis of peripheral tumors can be made with CT–guided transthoracic needle biopsy (9). In our case, the tumour was located in the left main bronchus. Hence, bronchoscopy guided biopsy was done; which was positive for typical carcinoid tumour, grade 1.
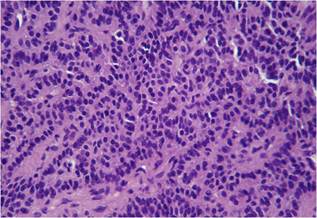
Figure 3. Haematoxylin and Eosin section shows Grade 1 neuroendocrine carcinoma (NEC).(10x).
4. Radiologic Features
Typical and atypical bronchial carcinoids have the same radiologic features, which depend largely on tumor location. About 80% of bronchial carcinoids arise centrally in the main, lobar, or segmental bronchi and demonstrate no specific lobar distribution (11). Radiologic findings include hilar or perihilar masses, endobronchial nodules, findings related to bronchial obstruction, and peripheral nodules. Hilar or perihilar masses is usually a well-defined, round or ovoid lesion and may be slightly lobulated at radiography and CT. The tumors range from 2 to 5 cm in size. Cavitations are rare. Multifocal tumors are rarely observed (11). CT demonstrates the endobronchial and extraluminal content of tumour. Sometimes, carcinoid may cause obstruction resulting in peripheral atelectasis and post-obstructive pneumonia. In approximately 20% of cases, a bronchial carcinoid may manifest as a solitary pulmonary nodule in the lung periphery, distal to segmental bronchi (11, 12). Some of them show calcification. In fact, it has been suggested that the diagnosis of bronchial carcinoid be made if there is a well-defined, centrally located tumor that narrows, deforms, or obstructs an adjacent airway and contains diffuse or punctuate calcification (12).
Carcinoids are characteristically highly vascular. At CT, a carcinoid is perihilar in location with marked, homogeneous contrast enhancement and may mimic a pulmonary varix or pulmonary artery aneurysm (13). However, not all carcinoids enhance, and enhancement alone neither allows bronchial carcinoid to be differentiated from bronchogenic carcinoma nor excludes the diagnosis (14). Furthermore, atypical carcinoids may have irregular contours and less uniform contrast enhancement.
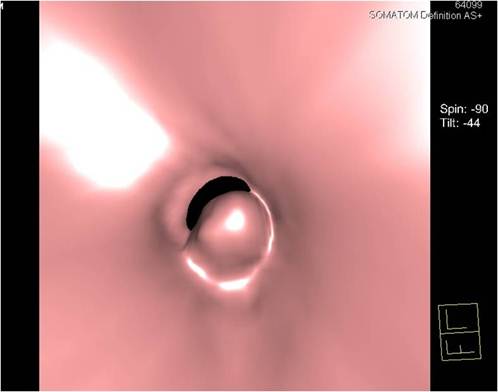
Figure 4. Virtual Bronchoscopy image demonstrates the partially occluded left main bronchus tumour with air cleft.
5. Management
The treatment is surgical with the focus on lung sparing or bronchoplastic surgery. Endoscopic resection of endobronchial tumours and endoscopic laser resection also has a role to play (15). Radiation therapy has a palliative role in disseminated disease, but its value of curative therapy is limited. In our case, first Bronchoscopic resection of tumour was done. Follow up CT thorax and PET-CT showed residual tumour which is being further planned for radiotherapy treatment.
6. Conclusion
Bronchial carcinoids are neuroendocrine tumors that range from low-grade typical carcinoids to more aggressive atypical carcinoids. The characteristic imaging features of these lesions are centrally located tumors, with well-defined borders and a clearly defined relationship with bronchi. Most of the cases are misdiagnosed as recurrent bronchial asthma. CT and Bronchoscopy should be considered in all cases of bronchial asthma or chronic obstructive pulmonary disease which do not respond to standard treatment. FDG PET-CT is important investigation in view of detection of concurrent small carcinoid tumour in the body, apart from endobronchial location. Radiologist has a pivotal role to play in early and accurate diagnosis of bronchial carcinoid. This would help to optimize surgical planning with complete resectibility.
References
- Colby TV, Koss MN, Travis WD. Carcinoid and other neuroendocrine tumors. In: Colby TV, Koss MN, Travis WD, eds. Atlas of tumorpathology: tumors of the lower respiratory tract, fasc 13, ser 3. Washington, DC: Armed Forces Institute of Pathology, 1995; 287–317.
- Paladugu RR, Benfield JR, Pak HY, Ross RK, TeplitzRL. BronchopulmonaryKulchitzky cell carcinoma: a new classification scheme for typical and atypical carcinoids. Cancer 1985; 55:1303–1311.
- Godwin JD II. Carcinoid tumors: an analysis of 2837 cases. Cancer 1975; 36:560–569.
- Buck JL, SobinLH. Carcinoids of the gastrointestinal tract. RadioGraphics 1990; 10:1081–1095.
- Fraser RG, Pare´ JAP, Pare´ PD, Fraser RS, Genereux GP. Neoplasms of pulmonary neuroendocrine cells. In: Fraser RG, Pare´ JAP, Pare´ PD, Fraser RS, Genereux GP, eds. Diagnosis of diseases of the chest. 3rd ed. Philadelphia, Pa: Saunders,1991; 1476–1497.
- Kulke MH, Mayer RJ. Carcinoid tumours. N Engl J Med. 1999;340:858–868 (doi: 10.1056/NEJM199903183401107).
- Dusmet ME, McKneally MF. Pulmonary and thymic carcinoid tumors. World J Surg 1996; 20: 189–195.
- Horton KM, Fishman EK. Cushing syndrome due to a pulmonary carcinoid tumor: multimodality imaging and diagnosis. J Comput Assist Tomogr 1998; 22:804–806.
- Rosado de Christenson ML, Abbott GF, KirejczykWM, Galvin JR, Travis WD. Thoracic carcinoids: radiologic-pathologic correlation. RadioGraphics 1999; 19:707–736.
- Hage R, de la Rivière AB, Seldenrijk CA, Bosch JMM van den. Update in pulmonary carcinoid tumours: a review article. Ann SurgOncol. 2003;10: 697–704 (doi: 10.1245/ASO.2003.09.019).
- Nessi R, Basso Ricci P, Basso Ricci S, BoscoM,Blanc M, Uslenghi C. Bronchial carcinoid tumors: radiologic observations in 49 cases. J ThoracImaging1991; 6:47–53.
- Magid D, Siegelman SS, Eggleston JC, FishmanEK, Zerhouni EA. Pulmonary carcinoid tumors: CT assessment. J Comput Assist Tomogr 1989; 13:244–247.
- Naidich DP. CT/MR correlation in the evaluation of tracheobronchial neoplasia. RadiolClin North Am 1990; 28:555–571.
- AronchickJM, Wexler JA, Christen B, Miller W, Epstein D, Gefter WB. Computed tomography of bronchial carcinoid. J Comput Assist Tomogr 1986; 10:71–74.
- AvecillasJF, Mehta AC. Flexible bronchoscopy and the use of lasers. In: Wang KP, Mehta AC, Turner JF, editors. FlexibleBronchoscopy. 2nd edition. Massachesselts: Blackwell Publishing, 2005; 157-173.



