Carcinoma Cervix Presenting as Foot Drop - A Case Report
Gupta P.*, Sethi P. K., Batra A., Anand I.
Ganga Ram Institute of Post-Graduation Medical Education (GRIPMER), New Delhi, India
Abstract
Lumbosacral plexopathy is rare but one of the most disabling complications of pelvic tumors and is an initial presentation in only 15% of cases. Here we present the case of 72 year old female who presented to us with foot drop and severe pelvic pain. She was investigated thoroughly and she turned out be a case of cervical carcinoma (advanced stage). Interestingly, diagnostic laparoscopy had to be done to establish the diagnosis. Cervical carcinoma, although rare, should always be kept as possibility for every female patient who presents as foot drop associated with pelvic pain because many patients who don’t have menstrual symptoms may be missed.
Keywords
Plexopathy, Cervical Carcinoma, Foot Drop, Limbo Sacral
Received: March 20, 2015
Accepted: April 19, 2015
Published online: May 27, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Lumbosacral plexopathy is rare but one of the most disabling complications of pelvic tumors. Tumor plexopathy is symptomatic in approximately 1 of 100 patients with cancer. (1) It may manifest as leg weakness or incapacitating pain that immobilizes the patient, leading to infection, venous thrombosis, and decubitus ulcers. (2) However, Plexopathy is the initial presentation of cancer in only 15% of patients. Lumbosacral plexopathy may be due to primary tumor, metastasis, or may be a complication of radiation therapy in cancer patients (3). The most prevalent types of tumors are colorectal tumors (20%), sarcomas (16%), breast tumors (11%), lymphoma (9%), and cervical tumors (9%). (4). Here we present an interesting case of lumbo-sacral plexopathy manifesting as left foot drop, which turned out to be a complication of Cervical carcinoma.
2. Case Report
We present the case of a 72 year old, post-menopausal female presenting with history of pain in the left leg and left groin, associated with burning micturition off and on, starting 8 months back. She got investigated for it when it reappeared one month later. Ultrasound abdomen was done which was suggestive of ureteric calculus, for which Non-contrast CT of kidney Ureter Bladder (NCCT-KUB) was done but no calculus was detected. Incidentally she was detected to have left sided non-functioning kidney. After that she remained asymptomatic for two months, and then she started with swelling -Deep vein thrombosis (DVT) of the left lower limb and was started on Low Molecular Weight heparin and then shifted on oral anticoagulants. One month later she started to have numbness in the left lower limb which was ignored initially and was attributed to DVT only. But later she started to develop difficulty in moving left foot and was referred to us as a case of left foot drop with severe pain in the left lower limb. When we examined her, she was having DVT left lower limb, along with left foot drop (distal power grade 0/5), but we noticed that she had left proximal weakness (proximal power grade 3/5) along with sensory loss over L4, L5, S1 and S2 dermatomes also. MRI spine was already done and it was normal. In the past history, she had Chronic Lymphocytic Leukemia detected 8 years back for which she was on regular follow-up and was not on any chemotherapy. Also there was history of left hip fracture 14 years back for which dynamic hip screws were placed. Due to the involvement of multiple nerve roots, we suspected lumbosacral plexopathy and MRI hip was done which revealed marrow signal alteration involving the sacrum, left iliac bone and acetabulum with left epidural soft tissue at S1-S2 level resulting in marked compression of thecal sac and encasement of sacral nerve roots. Unfortunately we could not do a contrast study due to the single functioning kidney status of the patient. So considering a mitotic pathology, we did a PET-CT (without contrast) which revealed a large lobulated heterogenous soft tissue mass on left side of pelvis, possibly arising from uterus and cervix with sacral and lymph node involvement with distant metastasis in lung. Serum levels of tumour markers, CEA, CA 125, and CA 19-9 were normal. We tried to take a biopsy transvaginaly but TVS could not be done as the vagina was stenosed. So a CT guided FNAC was done from the left hemi-pelvis but the tissue was inadequate for making a diagnosis. Ultimately, we went for the Laparoscopic approach in which multiple peritoneal deposits were seen and biopsy was taken. Biopsy revealed poorly differentiated squamous cell carcinoma, primary in cervix, positive for P63 and negative for ER and PR. So our case was an unusual case of a Cervical carcinoma, that presented as foot drop and finally got detected on diagnostic laparoscopy. We learned two important things; first always try to investigate the cause of any pain especially if it is severe even if it subsides. We can miss many important diagnoses by simply managing pain symptomatically. Secondly screening of cervical carcinoma should be done regularly in all elderly females because not all patients present to gynaecologists with menstrual symptoms and it is a treatable cancer.
3. Discussion
In two retrospective reviews from cancer hospitals, based on 12,000 patient visits per year, the prevalence of Lumbosacral plexopathy was 0.71% (2, 5). This incidence is higher in patients with pelvic tumors. In one study, the Lumbosacral plexus was involved in 50 of 2261 cases of cervical cancer; however, it was involved in 38 of the 74 patients (51%) in the subgroup with proven retroperitoneal metastatic disease. (6) The actual prevalence may be higher, as not all patients with plexopathy accompanying terminal malignancy are reported. The Lumbosacral plexus lies in the retroperitoneal space just lateral to the cervix or prostate and on top of the ilio-psoas muscle. It is close to bony and soft tissues that are frequently involved by tumors, and may therefore be invaded directly by tumors or compressed against the rigid bony pelvis (2). It is anatomically divided into lumbar (L1-L4) and sacral (L5-S1) portions, at the border of the true pelvis. These portions are connected by the lumbosacral trunk (L4-L5), which courses over the sacral ala at the pelvic brim. In general, bulky tumors within the pelvis compress and invade the plexus directly. On occasion, tumor tracks along the connective tissue and epineurium of the nerve trunks (7). This tendency to infiltrate along the nerve may explain why some patients with findings of diffuse plexopathy do not have radiographically demonstrable mass lesions and why in some circumstances the location of the pelvic tumor seems unrelated to the principal site of neurologic involvement. Three clinical syndromes of lumbosacral plexopathy are identified (2): upper (L1-5), lower (L5-S3) and Pan plexopathy. The lower (sacral) plexus is involved most frequently (approximately 50%), followed by upper plexus involvement (more than 30%) and pan plexopathy (18%).Bilateral plexopathy occurs in 25% of cases and is usually caused by breast cancer metastases. Lower plexus involvement occurs generally with colorectal and cervical neoplasms. Our patient had both upper and lower plexus involvement, predominantly lower plexus involvement. The most prominent symptom for all locations is severe, burning and continuous leg pain which is minimally responsive to narcotics. Pain that worsens with movement or weight bearing generally implies nearby bony invasion, same was the case with our patient. Pain is so common (98%) that its absence should raise a red flag regarding this diagnosis. Symptomatic weakness and sensory complaints eventually develop in 60% of patients. (1) Rigid knee extension for ambulation and difficulty arising from sitting are observed in upper plexopathy while foot drop, pelvic tilt and pelvic lordosis are noted in lower plexopathy. (8) Incontinence and impotence are typically absent unless bilateral plexopathy is present. Tumors deep in the pelvis, in particular those accompanying Cervical cancers and tumors of the rectosigmoid region, present with numbness and dysesthesias in the perianal area and perineum (1) which was not seen in our patient. The clinical diagnosis of neoplastic lumbosacral plexopathy is confirmed by magnetic resonance imaging (MRI) or computed tomography (CT) scanning of the affected areas. In some patients, other techniques such as positron emission tomography (PET) or bone scintigraphy is required. In metastatic plexopathies, the CT scan is usually positive for a soft tissue mass with or without enlarged lymph nodes that may erode the sacrum on the side of involvement but patients with radiation-induced plexopathies have unremarkable CT scans (3). MRI is preferred, because it is more sensitive and provides better detail than CT scanning (9). PET scanning can aid in the detection of active malignancy in the plexus region. (10). However, the sensitivity or specificity of PET scanning in the diagnosis of tumor plexopathy is not yet clear. The findings of Electromyography (EMG) and nerve conduction studies (NCS) are variable. Evidence of active or chronic denervation is found in the EMG's of most patients and it often reveals more extensive denervation than would have been predicted clinically (8).Treatment of cancer-related plexopathy is largely palliative and symptom directed. It involves radiation to the involved field, chemotherapy and pain control measures. In one study treatment with radiation was attempted in 26 plexopathy patients with a confirmed retroperitoneal mass. One month after therapy, nine (35%) patients noted diminished pain whereas ten (38%) patients noted no improvement or progression of their pains and none of the patients were documented to have improvement of neurologic signs after radiation therapy. Consultation with pain management specialists is recommended. Studies have shown that pain is often poorly controlled in patients with plexopathy. Dysesthesias and causalgia are resistant to therapy, but may respond to transcutaneous nerve stimulation, tricyclic antidepressants, anticonvulsants such as gabapentin, carbamazepine or phenytoin, or regional nerve or sympathetic ganglion blocks. Lymphedema may be treated with compressive devices and elevation. Preventative measures, including adequate pain management, initiation of physical rehabilitation, and assessment of home equipment needs may have a significant impact on preservation of quality of life in these patients.(1) The prognosis is poor. Thomas et al (11) reported 86% mortality within 3 years of the onset of neurologic symptoms. Jaeckle et al (2) reported that 40 of 85 patients died within an average of 5.5 months. Saphner et al (6) also reported a survival time of less than six months for all patients with lumbosacral plexopathy due to cervical carcinoma. For a number of years, radio-chemotherapy has been the treatment of choice in cervical cancer patients, starting from stage I-B2. One of the complications associated with cancer treatment that is extremely rare but, at the same time, provides many diagnostic and even more therapeutic problems is radiation induced plexopathy. The occurrence of symptoms as sensory loss in the lower extremities, muscular weakness, paresis and growing pain should raise, first of all, suspicion of nervous system involvement (pelvic nerves, spinal cord) by tumor, particularly in patients irradiated for advanced cervical cancer and then consider the possibility of radiation induced plexopathy.
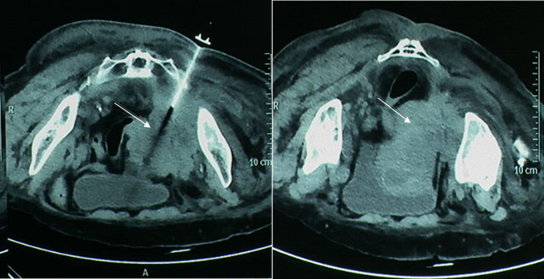
Figure 1A and 1B. CT images of the pelvic mass (Carcinoma Cervix) presenting as foot drop.
References
- Soc-neuro-onc.orghttp://soc-neuro-onc.org/levin/Levin_ch18_p413-422.pdf
- Jaeckle KA, Young DF, Foley KM. The natural history of lumbosacral plexopathy in cancer. Neurology. 1985; 35:8-15
- Pettigrew LC, Glass JP, Maor M, Zornoza J. Diagnosis and treatment of lumbosacral plexopathies in patients with cancer. Arch Neurol. 1984; 41:1282-1285
- Klimek M, Kosobucki R, Luczynska E, Bieda T, Urbanski K. Radiotherapy-induced lumbosacral plexopathy in a patient with cervical cancer: a case report and literature review. Contemp Oncol (Pozn). 2012;16(2):194-6
- Kori SH, Foley KM, Posner JB. Brachial plexus lesions in patients with cancer: 100 cases. Neurology.1981; 31:45–50.
- Saphner T, Gallion HH, Van Nagell JR, Kryscio R, Patchell RA. Neurologic complications of cervical cancer. A review of 2261 cases. Cancer.1989; 64:1147-1151
- Ebner I, Anderl H, Mikuz G, Frommhold H. [Plexus neuropathy: tumor infiltration or radiation damage]. ROFO Fortschr Geb Rontgenstr Neuen Bildgreb Verfahr. 1990; 152:662–666.
- Guzey FK, Guzey D, Cel AS, Aycan A, Kaplan R, Ozkan N. Lumbosacral Plexopathy in a Patient with Metastasis of Cervix Carcinoma: A Case Report. Turkish Neurosurgery 2006; 16(4): 204-207
- Taylor BV, Kimmel DW, Krecke KN, et al. Magnetic resonance imaging in cancer-related lumbosacral plexopathy. Mayo Clin Proc.1997;72(9):823-9
- Ahmad A, Barrington S, Maisey M, et al. Use of positron emission tomography in evaluation of brachial plexopathy in breast cancer patients. Br J Cancer.1999;79(3-4):478-82
- Thomas JE, Cascino TL, Earle JD. Differential diagnosis between radiation and tumor plexopathy of the pelvis. Neurology.1985; 35:1-7.



