Malignant Gastrointestinal Stromal Tumour of the Prostate - a Case Report
S. Gopalswamy1, *, J. S. O’Rourke1, J. Mathew2
1Department of Urology, Royal Cornwall Hospital, Truro, United Kingdom
2Department of Pathology, Royal Cornwall Hospital, Truro, United Kingdom
Abstract
Gastrointestinal stromal tumour (GIST) of the prostate is a very rare entity and only two such cases are reported in the literature. We report a case of GIST of the prostate in a 69 year old gentleman who had transurethral resection of the prostate (TURP) for benign prostatic hyperplasia (BPH) 7 years ago and subsequently presented with acute urinary retention from re-growth of the prostate. The prostate specific antigen level was 4 ug/l. The re-do TURP specimen showed the characteristic features of GIST, both microscopic and immunoprofile analysis. The possibility of secondary gastrointestinal GIST was excluded by endoscopy, imaging and tumour markers.
Keywords
GIST, Prostate, Urinary Retention, Imatinib
Received: March 19, 2015
Accepted: April 2, 2015
Published online: April 7, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Case Report
A 69 year old gentleman presented to the emergency surgical admitting unit with urinary retention. He also gave history of prostatism, dysuria and often fecal incontinence. He was a type-2 diabetic and treated for hypercholesterolemia. He under went TURP in 2001 for BPH. He had lost one stone weight over a period of two months. On examination, he was apyrexial and other vital were stable. He had distended urinary bladder and digital rectal examination showed markedly enlarged prostate. He was catheterised. His PSA was 4ug/l. Urine culture grew Pseudomonas and Enterococcus which were treated with appropriate antibiotics. A clinical diagnosis of BPH was made and treatment was commenced with tamsulosin, but unfortunately he failed trial without catheter ten days latter. Subsequently he underwent re-do TURP. The specimen weighed 50 gms. The histology revealed over 90% of chippings composed of a proliferation of spindle cells resembling smooth muscle cells with foci of necrosis and fibrosis. There were upto five mitosis per ten high power field. The spindle cells were positive for smooth muscle markers (SMA and SM-HCM) but also positive for CD34 and CD117. The diagnosis was malignant GIST. Contrast enhanced staging CAT scan demonstrated a large, partly necrotic mass within the presacral region measuring 9.7 by 14 cms and was contiguous with the posterior aspect of the bladder with no evidence of distant metastasis. The mass displaced the rectum and sigmoid colon to the left. MRI scan confirmed the mass arising from prostate and infiltrating the bladder. Flexible sigmoidoscopy showed no mucosal or obvious sub-mucosal primary tumour.The rectum was not distensible up to 20 cms and looked like a tunnel because of extramural compression. CEA and CA19-9 were within normal range. Loop colostomy was performed for stool incontinence and treatment with imatinib (Glivec) commenced. The tumour partially responded to imatinib. He is awaiting a cystoprostatectomy.
2. Discussion
In men prostate adenocarcinoma is the most common malignancy and the second leading cause of solid cancer mortality. Sarcomas constitute 0.1 to 0.2% of all malignant prostate tumours. Rhabdomyosarcoma is the most frequent mesenchymal tumour within the prostate and is seen almost exclusively in children [1]. Leiomyosarcomas are the most common prostate sarcoma in adults. Prostatic spindle cell lesions that arise only within the prostate, generally represents entities that originate from the prostate epithelium or stroma, such as sclerosing adenosis, sarcomatoid carcinoma, stromal tumors of uncertain malignant potential (STUMP), and prostate stromal sarcoma (PSS). Another subset of spindle cell tumors that involve the prostate are also found at other sites and include solitary fibrous tumor, leiomyosarcoma, and neural lesions among others [2].
Gastrointestinal stromal tumors (GISTs) have been recognised as a biologically distinctive tumor type, different from smooth muscle and neural tumors of the gastrointestinal tract. They constitute the majority of gastrointestinal mesenchymal tumors[3]. GISTs occur predominantly in persons over 50 years of age with an equal sex incidence. Benign GISTs outnumber the malignant ones by a margin of 10:1 [4]. GISTs occur throughout the gastrointestinal tract and are most common in the stomach (60-70%) and small intestine (30%). GISTs are rare in the esophagus, colon and rectum and and rare cases of primary extraintestinal stromal tumours (EGIST) have occurred in the greater omentum, mesentery and retroperitoneum. Individual cases of EGIST are described in the bladder, urethra, appendix, and very rarely in prostate [5-7]. Five percent of GISTs occur in patients with neurofibromatosis type 1 syndrome (multiple small intestinal tumors) and in Carney triad (gastric epithelioid GISTs in young females) [8]. Familial GISTs occur in patients with inheritable germline c-kit or platelet-derived growth factor receptor alpha (PDGFRA) mutations Histologically they may show a spindle cell or epithelioid pattern (the former largely corresponds with the designation of cellular leiomyoma and the latter with that of leiomyoblastoma) and pleomorphic patterns [8]. It is now believed that GISTs originate from gastrointestinal pacemaker cells known as interstitial cells of Cajal, that control gut motility or from a precursor of these cells. Immunohistochemical studies revealed that GISTs have similar features to the interstitial cells of Cajal, being positive with CD34 and c-kit, located on chromosome 4q12 and negative or variably positive for other neural and smooth muscle markers [9]. The identification of mutations mostly in exon 11 and to a lesser extent in exons 9 and 13 of the c-kit proto-oncogene coding for c-kit (CD117) in GISTs, has resulted in a better understanding of their oncogenic mechanisms [3]. Desmoids can form large GIST-like masses, but are composed of spindled or stellate-shaped cells in a densely collagenous stroma. Negativity for c-kit and nuclear positivity for beta-catenin are differentiating features. GI schwannomas, melanoma, and rare primary clear cell sarcomas are S100-positive, usually with characteristic histology. The latter two can be c-kit positive. C-kit positive non-GISTs include some sarcomas, especially angiosarcoma and Ewing sarcoma, extramedullary myeloid tumor, seminoma, and a few carcinomas, notably small cell carcinoma of lung [10].
There are different schemes for classification of GISTs. GISTs can be classified into very low risk, low risk, intermediate risk and high risk, based on tumor size and mitotic count [11]. Alternatively, they may be classified according to site, size and mitotic activity into three categories: benign, malignant and uncertain or low malignant potential[12].Tumours with mitotic counts higher than 5/10 high power fields or larger than 10 cm have a significant risk for recurrence and metastasis and are considered histologically malignant; however, some tumours with mitotic activity < 1/10HPF may metastasize indicating some uncertainty in malignant potential of GISTs, especially those larger than 5 cm[4]. In a study, size > or = 10cm, necrosis and/or pure epithelioid cell morphology correlated significantly with adverse survival [13].
The main treatment for EGIST is surgical resection. Although it is necessary to expand the scope of surgical resection, extensive clearance of lymph nodes is not recommended because lymph node metastasis is very rare in EGIST. Imatinib mesylate (imatinib, Glivic/Gleevec), an orally administered 2-phenylaminopyrimidine derivative that is a competitive inhibitor of the tyrosine kinases associated with platelet-derived growth factor (PDGF) receptors, the Abelson (ABL) protein and the c-kit protein [14]. Hence imatinib is used as adjuvant treatment in EGIST. Now the second generation of tyrosine kinase inhibitors are available.
3. Conclusion
GISTs of the prostate are very rare. But their identification is very important because of specific targeted treatment with tyrosine kinase inhibitors and surgery. Hence the pathologist and clinician should be aware of this rare entity. We report a rare case of GIST prostate.

Fig. 1. CT showing necrotic mass from presacral area to bladder
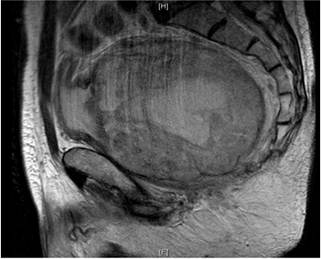
Fig. 2. MRI showing mass arising from prostate and displacing rectum and sigmoid colon.
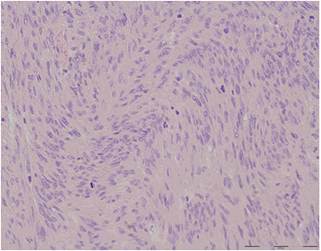
Fig. 3. Tumour composed of relatively bland spindle cells with faintly fascicular pattern. Note the numerous mitotic figures.
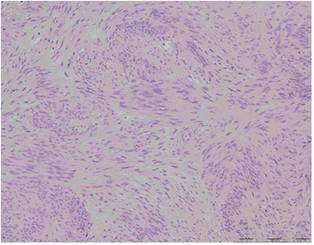
Fig. 4. Tumour with spindle cells and fascicular pattern
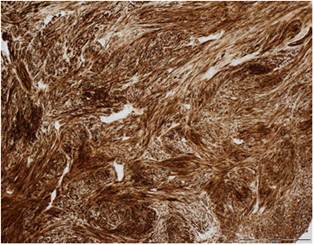
Fig. 5. Tumour cells stain strongly with CD117.
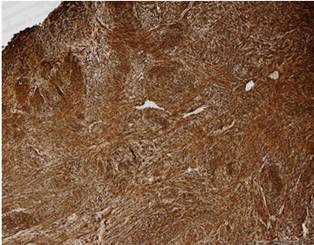
Fig. 6. Tumour cells stain strongly with CD34.
References
- Chii-Hong Lee, Yun-Ho Lin, Hsia-Yu Lin et al. Gastrointestinal stromal tumor of prostate: a case report. Human pathology (2006) 37, 1361-1365.
- Hansel DE, Herawi M, Epstein JI. Spindle cell lesions of the prostate. Mod Pathol. 2007 Jan;20(1):148-58.
- Miettinen M, Majidi M, Lasota J. Pathology and diagnostic criteria of gastrointestinal stromal tumours: a review. Eur J Cancer. 2002 sep; 38 Suppl 5:S39-51.
- Miettinen M, Lasota J. Gastrointestinal stromal tumours:pathology and prognosis at different sites. Semin Diagn Pathol.2006 may; 23(2):70-83.
- Miettinen M, Monihan JM, Sarlomo-Rikala M. Gastrointestinal stromal tumors/smooth muscle tumors (GISTs) primary in the omentum and mesentery: Clinicopathologic and immunohistochemical study of 26 cases. Am. J. Surg. Pathol. 1999; 23: 11098.
- Reith JD, Goldblum JR, Lyles RI. Extragastrointestinal (soft tissue) stromal tumors: An analysis of 48 cases with emphasis on histologic predictors of outcome. Mod. Pathol. 2000; 13: 5775.
- Van der Aa F, Sciot R, Blyweert W. Gastrointestinal stromal tumor of the prostate. Urology2005; 65: 388.
- Miettinen M, Lasota J. Gastrointestinal stromal tumours: review of morphology, molecular pathology, prognosis and differential diagnosis. Arch Pathol Lab Med. 2006 Oct;130(10):1466-78.
- Rosai J. Gist:an update. Int J Surg Pathol 2003;11:177-86.
- Dow N, Giblen G, Sobin LH, et al. GIST: differential diagnosis. Semin Diagn Pathol. 2006 may;23(2):111-9.
- Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 2002;33:45965.
- Miettinen M, El Rifai W, Sobin HL, et al. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol 2002;33:47883.
- Koay MH, Goh YW. Segal A et al. GISTs:a clinicopathological and molecular study of 66 cases. Pathology. 2005 Feb;37(1):22-31.
- Croom KF, Perry CM. Imatinib mesylate:in the treatment of GISTs. Drugs.2003;63(5):513-22.



