Colonic Esophageal Reconstruction by Substernal Approach for Caustic Stricture: What is the Impact of the Enlargement of the Thoracic Inlet on Cervical Anastomotic Leakage
A. Boukerrouche*
Department of Digestive Surgery, Hospital of Beni-Messous, University of Algiers, Algiers, Algeria
Abstract
Background: The two most commonly employed options for esophageal reconstruction are the posterior mediastinal route and the substernal route. Therefore, the biggest disadvantage of the retrosternal approach is the potential risk for compression of the graft at the site of the thoracic inlet. The purpose of this study is to report our results by analysing the impact of the enlargement of the thoracic inlet by removing the left half of manubrium and internal third of clavicle on the cervical anastomotic leakage. Methods: From 2005 to 2013, 82 left colonic interpositions for oesophageal caustic stricture were performed at our institution. There were 70 women and 12 men. Ten patients had a hypopharyngeal stricture that required also reconstructive surgery. Dilation was done in 56 patients. Results: An esophagocolic anastomosis was performed in 72 patients. A gastroenteroanastomosis was performed before reconstruction in 10 patients. A pharyngoplasty was associated in 10 patients. The thoracic inlet was enlarged in 35 patients .The colonic graft was anastomosed to the posterior surface of the stomach in 69 patients. The mortality rate was 2.43 %. Graft necrosis occurred in two patients. Cervical leakage was occurred in 25 patients. Eight patients developed a cervical stricture. statistical analysis revealed that the non-enlargement of the thoracic inlet was a predictive factor of cervical leak (OR; 3.63, CI; 1.06 -12.40, P= 0.039). Therefor the enlargement is associate with lower rate of cervical leak. The functional results was good. Conclusion: the non-enlargement of the thoracic inlet is a predisposing factor of cervical leak in substernal colonic interposition. Therefore the enlargement seems reduce the cervical leakage.
Keywords
Esophageal Reconstruction Left Colic Graft, Substernal Route, Cervical Leak, Enlargement of Thoracic Inlet
Received: March 4, 2015
Accepted: March 27, 2015
Published online: April 10, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
The construction of a long graft requires the sacrifice of the blood supply, leading to reduced circulation to the graft. The key point of Esophageal reconstruction is to ensure that the cervical anastomosis is without tension by using a graft with sufficient length and sufficient blood supply. Colon interposition is the method of choice to restore the digestive tract after esogastrectomie or for caustic stricture. Isoperistaltic left colic transplant supplied by the left colic pedicle and interposed by RS is an excellent long-term replacement organ for an esophageal caustic stricture. When performed by an experienced surgeon, it is an effective procedure with acceptable operative mortality, early morbidity, and good long-term functional results[1].
There are multiple options for the placement of the digestive conduit therefore the two most commonly employed options are the posterior mediastinal route and the retrosternal route.
The use of the mediastinal route needs the ablation of the native esophagus .this and other disadvantages of the posterior mediastinal (PM) route have prompted some surgeons to advocate an alternate route of reconstruction, namely the retrosternal (RS) approach. In 1955, Dale and Sherman firstly introduced colonic reconstruction by retrosternal approach [2]. Therefore, the biggest disadvantage of the retrosternal approach is the potential risk for compression of the graft at the site of the thoracic inlet, which can lead to mechanical ischemia. To prevent this event, some surgeons suggested to the enlarge of the thoracic inlet [3,4,5]. The aim of this study is to report the impact of the enlargement of the thoracic inlet on the cervical anastomotic leakage after substernal colonic interposition for esophageal caustic stricture. The purpose of this study is to report our results by analysing the impact of the enlargement of the thoracic inlet by removing the left half of manubrium and internal third of clavicle on the cervical anastomotic complications
2. Patients and Methods
2.1. Patients
In a continuous prospective study conducted from 2005 to 2013, 82 left colonic interpositions for oesophageal caustic stricture were performed at our institution. There were 70 women (85,3 %) and 12 men (14.6 %). The mean age of patients was 25 years (ranging 15 to 70). Ten patients (12.1 %) had a hypopharyngeal stricture that required also reconstructive surgery. Fifty five patients with esophageal caustic stricture had undergone previous dilation. Median delay from caustic injury to chirurgical reconstruction was 12 months (ranging 3 months to 10 years).
2.2. Methods
The preoperative evaluation of the colon was performed in patients aged 45 or older by only colonoscopy. No patients underwent preoperative angiography. Nutritional disorders of surgical patients were corrected by enteral nutritional support before date of surgery. The surgical technique of choice used was the left isoperistaltic colon graft based on the left colonic vessels and pulled up to the neck by substernal approach. The adequacy of colonic graft blood supply was judged by preoperative inspection, palpation, transillumination and it was ascertained by the presence of a pulsatile flow in the marginal artery. The colic transplant was positioned behind the sternum snugly, avoiding tension, twisting and redundancy by resection of the proximal portion in excess of the graft. The thoracic scared oesophagus was not resected. We enlarge the thoracic inlet by resection of the left half of the manubrium and the sternal head of the left clavicle to ease the acute angulation created when the esophagus substitute deviates from its normal course into the posterior mediastinum and turns superficially to pass under the sternum (FIG.1,2). The scarred cervical esophageal tissue was resected completely and the cervical anastomosis was performed on healthy tissue using a hand-suturing technique in one layer and end-to-end. A pharyngoplasty was performed when necessary with the proximal portion of the transplant. The distal anastomosis was performed at the posterior side of the gastric antrum when the stomach is available. The pyloroplasty was not performed routinely, and a gastric tube was inserted into the fundus through the colon transplant to avoid the dilation of the graft. The third jejuna loop is isolated and used to insert a tube of jejunostomy and an exclusive early postoperative enteral nutrition by jejunostomy was started 24 hours after surgical reconstruction. Between 8th and 10th postoperative day and in the absence of clinical cervical leak, a barium study was done to assess the oesophagocolique anastomotic integrity.
2.3. Statistical Analysis
Statistical analyses were performed using Student’s t-test or the chi-square test. The multivariate analysis was performed by SPSS 11.0 for Windows (SPSS, Chicago,IL, USA). A P value of less than 0.05 was considered significant.
3. Results
The Median operative time was 3 hours (ranging 2h30 to 6 hours). Emergency total esophagogastrectomy was required in three patients. A gastroenteroanastomosis was performed before reconstruction in 10 patients because of early gastric stenosis .An esophagocolic anastomosis was performed in 87.8% of patients (n=72). A pharyngoplasty was associated in 10 patients (12.1%) using the proximal portion of the transplant. The thoracic inlet was enlarged in 45.1 % of patients (n=37), by the resection of the left half of manubrium and the head of the left clavicle (table 1). The distal end of the colonic graft was anastomosed to the posterior surface of the stomach in 84.1% of patients (n=69) and to the anterior surface in 12.1 % (n=10) .A colojejunal anastomosis was performed in three patients because of emergency esophago-gastrectomy. Jejunostomy was performed either before or concomitant with reconstructive process. The median hospital stay was 14 days (ranging 12 to 27 days).
Table 1. The thoracic inlet
| Thoracic inlet | No. of patients (%) n = 82 | No. of Cervical leak (%) n=25 |
| Opening (+) | 37 (45.2) | 5 (13.) |
| Opening (-) | 45 (54.8) | 20 (44.4) |
There were two operative deaths at 2nd and 3rd day for a mortality rate of 2.4 %. The causes of death were pulmonary emboli and visceral failure.
The main postoperative complications was listed in table 2 .Graft necrosis occurred in two patients (2,4 %). The necrosis was partial and involved the proximal portion of the transplant. It was diagnosed on first and second postoperative day .Cervical anastomotic leakage was occurred in 25 patients (30.4 %), at median postoperative day 9 (ranging 7 to12days). The leakage was treated conservatively and the spontaneous closure was obtained in all patients, after a median delay of 7 days (ranging 5 to 10 days). Eight patients (9.7 %) developed a cervical anastomotic stricture after a median postoperative delay of 12 months (ranging 2 to 18months). Two of these patients had a previous postoperative cervical leakage. The cervical anastomotic stricture was firstly and successfully treated by endoscopic balloon dilation in six patients and in the two other patients reoperation was needed. The anastomotic revision consisted of resection of structured party and performing a new anastomosis. The symptomatic gastrocolic reflux was occurred in 2 patients. The reflux was minor and it was managed with medical treatment and life-style modification. So to prevent or to minimize the risk of reflux, we performed the cologastric anastomosis on the posterior side of the stomach.
The result of the univariate and multivariate analysis revealed that the non-enlargement of the thoracic inlet was a predictive factor of cervical leak (OR;3.63, CI; 1.06 -12.40 ,P= 0.039 ). Therefor the rate of cervical leak was significantly lower (P =0.023 ) in the group of patients in whom the thoracic inlet was enlarged (Table 2, 3).
Table 2. Postoperative complications
| Complications | No. patients (%) |
| Graft necrosis | 2 (2,4) |
| Cervical leakage | 25 (30.4) |
| Cervical stricture | 8 (9.7) |
| Graft redundancy | 2( 2.4) |
Table 3. Results of univariate analysis
| Enlargement of thoracic inlet | No. Patients | p.value | signification |
| Yes | 37 | 0.072 | ns* |
| No | 45 | <0.0105 | s* |
ns*: non-significant
s*:significant
Table 4. Results of multivariate analysis
| variable | Odd ratio | 95 % | CI | P value | signification |
| Non- Enlargement of thoracic inlet | 3.63 | 1.06 | 12.40 | 0.039 | S* |
s*:significant
The graft redundancy was observed in two patients and it was treated by resection of the redundant portion and end -to -end colon anastomosis.
All the patients were reviewed regularly and evaluated to assess the functional results. The long term following up was ranged from 6 months to 9 years. All patients had exclusively an oral feeding with good swallowing except one patient who had experienced a minor difficulty to swallow. Body weight, as compared with the preoperative body weight increased in all patients. Dysphagie linked to cervical anastomotic stricture was occurred in eight patients. The improvement was obtained in six patients by dilation. The number needed was two to three dilations per year .Surgical revision needed in the tow others patients.
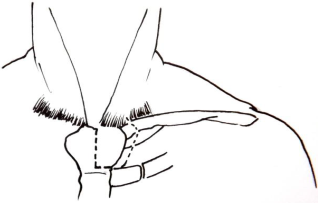
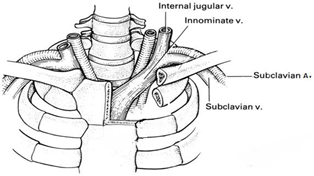
Fig. 1. Excision of the left half of the manubrium, the head of the left clavicle and first rib
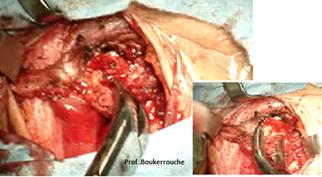
Fig. 2. Operative view of th enlargement of thoracic inlet
4. Discussion
Following esophagectomy or esophageal caustic stricture, there are a number of options to restore continuity of the upper gastrointestinal tract .Some considerations for reconstruction include: choice of conduit; technique of conduit construction; location of anastomosis; and the route of reconstruction are Important [4]. Each of these factors may have a significant impact on postoperative morbidity particularly the route of reconstruction. The substernal and the posterior mediastinal routes are most commonly applied. As reported in literature, the posterior mediastinum (PM) is preferred for immediate reconstruction after esophagectomy and the retrosternal route (RS) for delayed reconstruction of the upper gastrointestinal tract when access to the posterior mediastinum is difficult or technically not possible [6]. In case of esophageal caustic stricture, the scared esophagus adheres to adjacent organs which make its dissection risky and hemorrhagic, in addition patients with esophageal stenosis often are fed by jejunostomy and so they have a degree of malnutrition which represents an additional factor of operative complications[1]. Indeed we use exclusively the RS approach during esophageal reconstruction for caustic stenosis. The retrosternal route has been an alternative for oesophageal reconstruction after esophagectomy. But the longer route and the higher incidence for cervical anastomotic leakage compared with the posterior mediastinal approach have always hampered its wider use [7,8]. The biggest disadvantage of the substernal route is the potential risk for compression of the graft at the site of the thoracic inlet, which can lead to mechanical ischemia of the cervical portion of the graft causing a leakage or localized necrosis.
Cervical anastomotic leak has always been one of the major complications associated with the anterior reconstruction approach. The incidence of anastomotic leakage was higher than that of oesophageal reconstruction through the posterior mediastinum [9,10]. This incidence varied from 19 to 70% [11,12,13,14]. It has been reported that nearly 50% of cervical anastomotic leaks result from anastomotic strictures and the subsequent need for chronic dilatations, which negate the merits of an operation intended to restore comfortable swallowing [15]. Some authors have suggested that the increased risk of anastomotic leakage in patients who undergo retrosternal reconstruction is due to the additional length of reconstruction that is required if anastomosis is made over the neck and the tight angulation of the thoracic inlet [5,16] .When the graft is interposed via a RS, the position of the vessels must be checked constantly to ensure there is no compression on the transposed colon at the thoracic inlet because venous blood flow is very sensitive to a mechanical obstacle, which is thought to be the usual precipitating event for necrosis [1,2].
In order to facilitate exposure and to avoid compression of the interposed graft when it is brought up to the neck through the retrosternal route (RS) , some author favor removal of a portion of the manubrium, associated costal cartilage, and the medial portion of the left clavicle [2,5].
how to reduce the incidence of cervical anastomotic leaks has always been a priority for studies in the field of oesophageal surgery .Abo and colleagues [10,17], Orringer and Sloan [16] thought that the high rate of cervical leak in substernal esophageal reconstruction was caused by the increased pressure around the anastomosis stoma due to compression of the surrounding dense tissues, which deteriorates the blood supply in that region, leading to mechanical local ischemia and hypoxia. These authors used to expand the thoracic inlet by resecting the left sternoclavicular joint during the oesophageal reconstruction through the substernal approach [10,16.17] .
Our results of the multivariate analysis revealed that the non-enlargement of the thoracic inlet was a predictive factor for cervical leak ( OR;3.63 , CI; 1.06 -12.40 ,P= 0.039 ) . Therefore the enlargement by excision of the left half of manubrium and the head of the left clavicle was associated with statically significant lower rate ( P =0.023 )of cervical anastomotic leakage of patients in whom the thoracic inlet was enlarged. We remind that the enlargement is a non-invasive procedure without risk of secondary complications. It takes twenty minutes to achieve it without significant impact on the operative duration. In addition this procedure allows for sufficient access to the left internal thoracic vessels, which can be advantageous for successfully performing microvessel anastomosis of the graft when necessary.
At our institution and during colonic interposition through retrosternal approach, we expand systematically the thoracic inlet by by excision of the left half of the manubrium and the sternal head of the left clavicle in order to ensure there is no compression on the transposed conduit at the cervical level. Many surgeons recommend to associate this procedure to the substernal esophageal reconstruction [3,4,5,18,19,20,21,22]. Statistically our study has some bias. It is not randomized and has an unrepresentative sample number. So the results are not highly reliable however the study is ongoing and further results will be published later when the number of patients will be sufficient.
5. Conclusion
The non-enlargement of the thoracic inlet is a predisposing factor of cervical leak in substernal colonic interposition. Therefore the enlargement seems reduce the cervical leakage.
So we feel it is beneficial to expand the thoracic inlet during esophageal reconstructive surgery by substernal digestive graft interposition.
References
- Abdelkader Boukerrouche . Isoperistaltic left colic graft interposition via a retrosternal approach for esophageal reconstruction in patients with a caustic stricture: mortality, morbidity, and functional results. Surg Today (2014) 44:827-833.
- Dale and Sherman : interposition colique retrosternal .J Thorac Surg(1955)29:344-356
- DeMeester T R, Johansson K E, Franze I et al.(1988) ,Indications, surgical technique, and long-term functional results of colon interposition or bypass. Ann Surg; 208: 460-74.
- Takushi Yasuda and Hitoshi Shiozaki ,(2011) ,Esophageal Reconstruction with Colon Tissue, Surg Today 41:745–753
- Cattan P, Chiche P, Berney T, et al.(2001) Surgical approach by cervicosternolaparotomyn for the treatment of extended cervical stenoses after reconstruction for caustic injury. J Thorac Cardiovasc Surg;122:384–6. 6.
- Casson AG, Porter GA, Veugelers PJ.( 2002) Evolution and critical appraisal of anastomotic technique following resection of esophageal adenocarcinoma. Dis Esophagus;15:296–302.
- Ngan SY, Wong J. (1986 ) Lengths of different routes for esophageal replacement. J Thorac Cardiovasc Surg;91:790–2.
- Coral RP, Constant-Neto M, Silva IS, Kalil AN, Boose R, Beduschi T et al.( 2003 )Comparative anatomical study of the anterior and posterior mediastinum as access routes after esophagectomy. Dis Esophagus;16:236–8
- .Tilanus HW, Hop WC, Langenhorst BL, van Lanschot JJ. (1993) Esophagectomy with or without thoracotomy: is there any difference? J Thorac Cardiovasc Surg;105:898–903.
- Abo S, Fujiwara Y, Noto N. (1974) Sternal resection in cases of cancer of thoracic esophagus: method of esophageal reconstruction (in Japanese). Gekachiryou (Surg Therapy);30:597–601.
- Urschel JD, Urschel DM, Miller JD, Bennett WF, Young JE.( 2011),A meta-analysis of randomized controlled trials of route of reconstruction after esophagectomy for cancer. Am J Surg;182:470–5.
- Orringer MB, Marshall B, Stirling MC. (1993),Transhiatal esophagectomy for benign and malignant disease. J Thorac Cardiovasc Surg;105:265–76; discussion 276–277.
- Yoichi Hamai , Jun Hihara ,Manabu Emi , Yoshiro Aoki , Morihito Okada ,(2012), Esophageal reconstruction using the terminal ileum and right colon in esophageal cancer surgery. Surg Today 42:342–350
- Lerut T, Coosemans W, Decker G, et al.(2002) Anastomotic complications after esophagectomy. Dig Surg;19:92.
- Orringer MB, Marshall B, Iannettoni MD. (2000) Eliminating the esophagogastric anastomotic leak with a side-to-side stapled anastomosis.J Thorac Cardiovasc Surg;119: 277-88.
- Orringer MB, Sloan H. (1975) Substernal gastric bypass of the excluded thoracic esophagus for palliation of esophageal carcinoma. J Thorac Cardiovasc Surg;70:836–51.
- A.Boukerrouche .Left colonic graft in esophageal reconstruction for caustic stricture: mortality and morbidity
- Dis Esophagus.2013 Nov; 26(8):788-793.Abo S. Special issue on ‘my surgery.’ (1975) Sternal manubrium resection and anterior mediastinum esophageal reconstruction in cases of cancer of thoracic esophagus (in Japanese). Gekashinryo (Surg Therapy);171102–4.
- Cerfolio RJ, Allen MS, Deschamps C, Trastek VF, Pairolero PC. (1995) Esophageal replacement by colon interposition. Ann Thorac Surg;59:1382–4.
- Neville WE, Najem AZ. (1983) Colon replacement of the esophagus for congenital and benign disease. Ann Thorac Surg;36:626–33.
- Fujita H, Yamana H, Sueyoshi S, Shima I, Fujii T, Shirouzu K, et al. (1997) Impact on outcome of additional microvascular anastomosis —supercharge — on colon interposition for esophageal replacement: comparative and multivariate analysis. World J Surg;21:998–1003.
- Dowson HMP, Straus D, Ng R, Mason R. (2007) The acute management and surgical reconstruction following failed esophagectomy in malignant disease of the esophagus. Dis Espohagus;20: 135–40.
- Wain JC, Wright CD, Kuo EY, Moncure AC, Wilkins EW, Grillo HC, et al. (1999 )sLong-segment colon interposition for acquired Esophageal disease. Ann Thorac Surg;67:313–8.