Neoadjuvant Chemotherapy versus Primary Surgery in the Management of Advanced Stage Ovarian Cancer
Moawia E. Hummeida1, Howaida Sharif2, Duria A. Rais3, Khalid Yassin4, Azza Zulfo5, Kamal Hamad6, Abdel Aziem A. Ali7, *
1Department of Obstetrics and Gynaecology, Division of Gyno-oncology, School of Medicine, Alneelain University, Khartoum, Sudan
2Department of Obstetrics and Gynaecology, Khartoum Teaching Hospital, Khartoum, Sudan
3Department of Obstetrics and Gynaecology, Faculty of Medicine, Khartoum University, Khartoum, Sudan
4Department of Obstetrics and Gynaecology, School of Medicine, Alneelain University, Khartoum, Sudan
5Department of Pathology, Khartoum Teaching Hospital, Khartoum, Sudan
6Department of Clinical Oncology, Faculty of Medicine, Khartoum University, Khartoum, Sudan
7Department of Obstetrics and Gynaecology, Faculty of Medicine, Kassala University, Kasala, Sudan
Abstract
This was a prospective observational comparative hospital based study conducted in Khartoum Teaching Hospital, Sudan, during September 2011 and through February 2012, to evaluate the role of neoadjuvant chemotherapy (Paclitaxil and carboplatin) in the management of advanced ovarian cancer compared to primary surgery, and to determine the impact of neoadjuvant chemotherapy on the optimization of cytoreductive surgery. Chi-squaire and t tests were performed and P<0.05 was considered significant. A total of fifty patients were enrolled in this study, twenty patients received neoadjuvant chemotherapy and interval debulking surgery (IDS), and 30 patients underwent primary surgery (PS) and received adjuvant chemotherapy. In comparison with patients who received neoadjuvant chemotherapy there was higher proportion of patients showed intra-operative ascites (93.3% Vs 10%, P=<0.001), adhesion (66.6% Vs 0%, P=0.002), omental cake (53.3% Vs 15%, P=0.006) and distant metastasis (93.3% Vs 0%, P=<0.001) among the women who underwent primary surgery. This study showed optimal cyto-reductive surgery for the patients who received neoadjuvant chemotherapy in comparison with those who underwent primary surgery (100% Vs 50%, P=<0.001). The mean (SD) of hospital stay, ICU admission and units of blood transfusion was lower among patients who received neoadjuvant chemotherapy. Thus neoadjuvant chemotherapy is of more benefit than primary surgery in the management of advanced stage ovarian cancer.
Keywords
Ovarian, Cancer, Chemotherapy, Sudan
Received: February 24, 2015
Accepted: March 11, 2015
Published online: March 20, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Ovarian cancer is the second most common Gynecological cancer in women, and the leading cause of death. The current life time risk is 1 per 48, the incidence being approximately 22 per 100.000 populations [1]. Primary surgery for advanced ovarian cancer, has been the standard practice for more than 40 years; survival benefit is principally seen in patients who have optimal cytoreduction with no or small volume less than 1 cm residual tumor after surgery [2]. Frie in 1982 originally introduced the definition of Neoadjuvant chemotherapy to describe chemotherapy treatment of primary solid tumors before surgical ablation [3]. A recent clinical trial has shown that the survival of patients with operable advanced ovarian cancer is not disadvantaged by Neoadjuvant chemotherapy followed by surgery, thus complete cytoreduction could be achieved in a greater percentage of patients, if primary chemotherapy is used in women in whom optimal primary surgery would be difficult [4]. Neoadjuvant chemotherapy resulted in adequate tumor shrinkage and allowed for the surgical treatment of tumors previously considered unresectable [5]. There is a number of assumed advantage and potential disadvantages of neoadjuvant chemotherapy. The proposed advantages include: an increased rate of optimal residual disease, less extensive surgery, reduced blood loss, lower morbidity, shortened hospital stay, and improved quality of life which allow for more conservative surgery, or more cytoreductive surgery for unresectable tumors [5]. The potential disadvantage include the selection of resistant tumor cells clones, less complete tumor down staging, and higher local relapse as results of more conservative surgery and wound healing [5]. This study is designed and directed to evaluate the role of neoadjuvant chemotherapy in the management of advanced ovarian cancer in term of optimization of cytoreductive surgery.
2. Research Significance
Neoadjuvant chemotherapy resulted in adequate tumor shrinkage and allowed for the surgical treatment of tumors previously considered unresectable. This study confirmed that neoadjuvant chemotherapy followed by interval debulking surgery for the management of patients with stage III and IV ovarian cancer have improved the patient’ performance status, decrease need for transfusion, ICU admission and reduce hospital stay.
3. Procedures and Methods
This is a prospective observational comparative hospital based study conducted in Khartoum Teaching hospital, Sudan, during September 2011 and through February 2012 to evaluate the role of neoadjuvant chemotherapy (Paclitaxil and carboplatin) in the management of advanced ovarian cancer compared to primary surgery and to determine the impact of neoadjuvant chemotherapy on the optimization of Cytoreductive surgery. Khartoum Teaching Hospital provides tertiary care for women who receive reproductive health care at the hospital, as well as for referrals from other clinics and hospitals from different parts of Sudan. All women with risk factors or gynecological complications are referred to the hospital. The patients with gynecological cancers are collaboratively managed in this hospital and the Radio isotope center in Khartoum (RICK) neighboring the hospital. The standard therapy for patients with advanced disease is debulking surgery followed by platinium-based chemotherapy. After informed written consent all women with advanced ovarian cancer (according to the FIGO classification) [6]were included in this study to compare the women with advanced cervical cancer (stage III and IV) and who underwent primary surgery followed by chemotherapy to those who received neoadjuvant chemotherapy (Paclitaxil and carboplatin) followed by interval debulking surgery in term of intraoperative findings, need for blood transfusion, ICU admission, hospital stay, ability of chemotherapy to downstage the tumors and the rate of optimal cytoreduction. The selection of either modalities of treatment for each patient was made by the treating gynecologists based on clinical assessment, performance of patient and fitness for surgery. The neoadjuvant chemotherapy and interval debulking surgery was preceded by fine needle aspiration while those who underwent primary surgery tissue biopsy were taken for histo-pathological interpretation. Structured questionnaire was used to gather the relative data. Also the questionnaire included the demographic characteristics, menopausal status, presenting symptoms, and family history of other related malignancies. CA 125, Ultrasound findings, CT or MRI reports as well as intra-operative findings were obtained from the patients notes. Data relevant to chemotherapy treatment regimen and response were collected from patient’s records at the Radio isotope center in Khartoum RICK. To minimize the risk of chemotherapy-induced fibrosis, interval debulking surgery was performed after 3 cycles of neoadjuvant chemotherapy.
4. Analysis and Ethical Approval
Data were entered into a computer database and SPSS software (SPSS Inc., Chicago, IL, USA, version 16.0) and double checked before analysis. Chi-squaire and t tests were performed and P<0.05 was considered significant.
The study received ethical clearance from the Health Research Board at Khartoum Teaching Hospital, Sudan.
5. Results
A total of fifty patients were enrolled in this study, nearly one (30%), 15\50) and two (70%, 35\50) third were stage III and IV respectively. Twenty patients (40%) received neoadjuvant chemotherapy and interval debulking surgery (IDS), and 30patients (60%) underwent primary surgery (PS) and received adjuvant chemotherapy, figure 1.
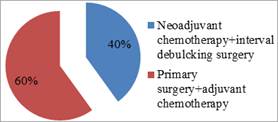
Figure 1. Distribution of patients according to the treatment modalities for advanced ovarian cancer in Khartoum hospital, Sudan: 2011-2012
Ten women (10%) were in the age group 21-40 years, 26 women (52%) were in age group 41-60 years and 14 women (28%) were above 60 years. 20% of the investigated women gave family history of ovarian cancer. Serum CA125 was normal (<35 u/ml) in 4 patients, levels between 35-200 u/ml were found in 9 patients (18%) and in 37 patients (74%) it was found to be more than 200 u/ml. Regarding histopathology, the results were in keeping with cystadenocarcinoma in 12 patients (24%), 10 patients (20%) were serous tumors, 8 patients (16%) were clear carcinoma, 4 patients (8%) showed mixed cell tumor, 8 patients (16%) had mucinous tumors, 4 patients poorly differentiated carcinoma, 2 patients(4%) showed endometrioid tumor and 2 patients (4%) transitional cell tumor. Analyzing the intra-operative findings and in comparison with patients received neoadjuvant chemotherapy there was higher proportion of patients showed intra-operative ascites (93.3% Vs 10%, P=<0.001) adhesion (66.6% Vs 0%, P=0.002), omental cake (53.3% Vs 15%, P=0.006) and distant metastasis (93.3% Vs 0%, P=<0.001) among the women who underwent primary surgery. This study showed optimal cyto-reductive surgery in a form of total abdominal hysterectomy\bilateral salpingopheracty plus partial omentectomy for the patients who received neoadjuvant chemotherapyin comparison with those who underwent primary surgery (100% Vs 50%, P=<0.001). The mean (SD) of hospital stay, ICU admission and units of blood transfusion was lower among patients who received neoadjuvant chemotherapy, table 1.
Table 1. Comparison of neoadjuvant chemotherapy \interval debulcking surgery and primary surgery\adjuvant chemotherapy for the management of advanced ovarian cancer in Khartoum hospital, Sudan: 2011-2012
| Variable | Neoadjuvant chemotherapy(N=20) | Primary surgery(N=30) | P |
| Intra-operative findings | |||
| Ascites | 2(10) | 28(93.3) | <0.001 |
| Adhesion | 0(0) | 20 (66.6) | 0.002 |
| Omental cake | 3 (15) | 16 (53.3) | 0.006 |
| Distant metastasis | 0 (0) | 28 (93.3) | <0.001 |
| TAH+BSO+O | 20 (100) | 15 (50) | <0.001 |
| Hospital stay, days | 5.1 (0.4) | 6.8 (1) | 0.013 |
| ICU admission | 4 (20) | 15 (50) | 0.032 |
| Blood transfusion, unit | 1.3 (1.1) | 3.6 (1) | <0.001 |
| Death | 1 (5%) | 5 (16.7) | 0.054 |
Data was shown as number (%) and mean (SD) as applicable. Abbreviation: TAH, total abdominal hysterectomy; BSO, bilateral salpingoopherecty; O, omentectomy.
6. Discussion
In this study we compared the neoadjuvant approach with the conventional treatment of primary debulking surgery followed by chemotherapy for patients with FIGO stage III and IV ovarian cancer. As published studies are controversial considering benefit of the neoadjuvant treatment, the aim of this study was to evaluate the effect of this approach on optimization of surgical intervention, associated mortality, admission to ICU, blood transfusion and hospital stay. The rational of neoadjuvant approach lies in the higher cytoreductibility to "optimal" status forwarded and possibly facilitated by chemotherapy [7]. The main issue is how to evaluate resectability of stage III-IV ovarian cancer? Despite improvement in CT, MRI, and tumor markers, the resectability of intraperitoneal disease remain difficult to judge [8]. Several predictive models have been proposed, but false-positive rates range from 5% to 37% hence surgical evaluation is therefore crucial[6,8,9]. The total numbers of patients included in the study were 50 women. Thirty patients underwent primary debulking surgery and 20 patients received neoadjuvant chemotherapy followed by interval debulking surgery. A critical point in order to define indications to neoadjuvant chemotherapy for advanced ovarian cancer is the determination of uniform selection criteria that can consistently identify patients with surgically unresectable disease without depriving others from potential advantage associated with an optimal primary resection. Several studies have been done to determine markers which can reliably predict optimal resectability. CT-scan findings, Serum Ca125, pleural effusion and ascites have been assessed in different studies in order to predict optimal debulking preoperatively, but up to now the predictive performance of all previous tests and investigations have not demonstrated sufficient accuracy to achieve widespread applicability [10,11]. Thus further investigations concerning patient’s selection seems warranted. Some authors have advocated an initial assessment of disease extent via open laparoscopy in order to more accurately predict surgical outcome [12.In this study debulking surgery was performed after 3 rather than six cycles of neoadjuvant chemotherapy. Earlier studies investigating the role of debulking surgery at the time of second- look surgery after six courses of chemotherapy did not improve survival [10], furthermore a meta-analysis of 21 different studies done between 1989-2005 have shown that for each cycle of chemotherapy that was given before surgery, there was a median corresponding decrease in patient survival of 4.1 months [13]. This makes clinical sense that there are a certain number of cycles that will work before resistant and subsequent recurrence develop. Therefore, in case where patients have been treated with neoadjuvant chemotherapy, we preferred an interval cytoreduction after 2 or 3 cycles of chemotherapy rather than attempted cytoreduction after 6 or more cycles. In this study it was observed that, of the 30 patients targeted with primary surgery, optimal cytoreduction in the form of TAH/BSO, omentectomy was achieved in only 50% of patients. Our finding is similar to what is in the literature, where optimal Cytoreductive surgery is possible in only 40-50% of cases with advanced stage ovarian cancer [14]. In the other 50% suboptimal cytoreduction was performed; limitations in surgery were explained by the presence of dense adhesions, fixity of the tumor to adjacent structures and due to the presence of metastasis. In a study by Vergote et al [9], the range of cytoreduction rates at primary Laparotomy among the various recruiting countries was between 3.9% and 62.9%. Six of the seven countries, including UK, had a complete cytoreduction rate of less than 12%. Data from the SCOTROC prospective randomized chemotherapy trial also showed cytoreduction rates in UK were significantly lower than other countries [15]. It is clear that differences in surgical practices substantially reflecting a wide divergence in professional opinions on the value of primary surgery in the management of advance stage ovarian cancer.In this study the number of patients that received neoadjuvant chemotherapy (Carboplatin and Paclitaxil) was 20 patients. The Intra-operative finding after the administration of chemotherapy were surprisingly different:, no visible distant metastasis and omental infiltrations were found in 15% of patients. The need for blood transfusion, hospital stay and ICU admissions were less; in comparison with patients underwent primary surgery and adjuvant chemotherapy. These findings are in line with a case control study conducted by Morice et al where an optimal resection was achieved in 94% of patients [16]. Our findings were also consistent with finding reported by Le et al [17], where 61 patients were treated empirically with neoadjuvant chemotherapy and interval surgery.
7. Summary and Conclusion
Some patients with advanced ovarian cancer present with clinical feature that can preclude optimal surgical intervention. This study confirmed that the neoadjuvant chemotherapy followed by interval debulking surgery for the management of patients with stage III and IV ovarian cancer improved the patient’ performance status, decrease blood loss and transfusion, ICU admission and reduce hospital stay. The ability of chemotherapy to downstage the tumors increased the rate of optimal cytoreduction by almost 100% in this study.
Acknowledgement
We sincerely thank all women who participated in this study.
References
- Siegel R, Ward E, Beawley O,Jamal A: The impact of eliminating socioeconomic and racial disabilities on premature cancer death.CA cancer J clic 2011,62:212
- Markman M: Concept of optimal ctytoreduction in advanced ovarian cancer: a brief action. J clin Oncol 2007, 25: 4168-70.
- Mazzeo M, Berliere and Kerger et al: Neoadjuvant chemotherapy followed by surgery and adjuvant chemotherapy in patients with primarly unresected, advanced ovarian cancer. Gynecol Oncol 2003,90: 136-169.
- Vrscaj MU, S. Rakar S: Neoadjuvant chemotherapy in advanced epithelial ovarian cancer: a retrospective case control study. Eur J Gynaecol Oncol 2002, 23: 405-410
- Daly m, Abrams GI: Epidemiology and risk assessment of ovarian cancer. Semin Oncol 1998, 25: 255-64.
- Petru E, Luck HJ, Stuart G:Gynecologic cancer intergroup (GCIG), proposal for change of the current FIGO staging system. Eur J Obstet Gynecol report Biol 2009, 143:69-74
- Hennessy BT, Coleman RL, Markman M: Ovarian cancer.Lancet 2009, 374:1371-82.
- Bristow RE, Duscka L, Lambrou N, et al: A model of predicting surgical outcome in patients with advanced ovarian carcinoma using CT. Cancer 2000, 89:1532-40.
- Vergote I, De Wever I, Tjalma et al: Neoadjuvant chemotherapy or primary debulking surgery in advanced ovarian carcinoma: A retrospective analysis of 285 patients. Gynecol Oncol 1998,431-436
- Nelson BE, Rosenfeld AT, Schwardz PE: Preoperative abdominopelvic CT prediction of optimal cytoreduction in epithelial ovarian carcinoma. J Clin Oncol. 1993, 11:166-72
- Camaci A, Balat O:Neoadjuvant chemotherapy in ovarian cancer. Eur Gynecol Oncol. 2002, 23: 437-441.
- Torres JC,Derchain SF, Faundes A, Gontijo RC, Martinez EZ, Andrade LA:Risk of malignancy index in preoperative evaluation of clinically ovarian cancer. Sao Paulo Med J 2002, 120:72-6
- Huober A, Meyer U, Wagner A and Wallwiener D: The role of neoadjuvant chemotherapy and interval Laparotomy in advanced ovarian cancer.J Cancer Res Clinc 2000,128: 153-160.
- Jamal A, Thomas a, Murray T, Thun M: Critique, and a call for change.Cancer statistics 2002. CA Cancer J 2002, 52:32-47.
- Cawford SC, Vasey PA, Paul Jay et l: Does aggressive surgery only benefit patientswith less advanced ovarian cancer? Results from international comparison within the SCOTROC1, trial.J L Cline Oncol 2005, 23:8802-11.
- Morice P, Brehier Olive D, Rey A, et al:Results of interval debulking surgery in advanced stage ovarian cancer: an exposed non exposed study. Ann Oncol. 2003, 14:74-77.
- Le T, Giede C, Salem S, Lefebvre G et al: Society of Obstetrician and Gynaecologists of Canada. Initial evaluation and referral guidelines for management of of Pelvic/ovarian masssses.J Obstet Gynaecol Can 2009, 31:668-80.