An Overview and Insights into Osteochondroma – A Rare Tumor of Bone and Cartilage
Josphine Jenifer P., Narendra Nixon, Priyanka S., Amrit Rai, Seshadri B., Anusha K., Vasu R., Ravi Theaj Prakash U., Ramakrishnan M.*
PG Department of Bioscience, CMR Institute of Management Studies, OMBR Layout, Banasawadi, Bangalore, Karnataka, India
Abstract
Osteochondromas are the rare benign and malignant tumour of the growing bone, usually affecting the young adults. Solitary osteocartilaginous exostosis is more common than the hereditary multiple exostosis (HME). The first 3 decades of life has maximum chances of getting affected with osteochondroma and hardly occurs in craniofacial bones because of the fact that these bones are not formed by endochondral ossification. Most of the symptoms occur at the periphery of the bone tissues, with causes of osteochondroma being unknown. It involves in genetic condition and is associated with mutations of EXT1 or EXT2 genes. Diagnosis is difficult at symptomless stage, incidentally it is diagnosed when X-ray is carried out. Detection of tumor by ultra sound is accurate than other diagnosis process. No treatment is required other than regular monitoring of tumor. Standard allele specific PCR based techniques on osteochondroma showing both recombine and intact alleles were reported. The observation shows that osteochondroma complicated clonal growth is due to EXT-1-null chondrocytes, variation in the percentage of lacZ genes and researchers recommended that narrow follow ups are required for further developmental analysis with absolute certainty. In this review, a report on research and developments of osteochondroma is discussed with authors suggestions.
Keywords
Bone deformity, Bone Morphogenic Proteins, Gene mutation, Multiple Hereditary Exostosis, Osteochondroma,
Solitary Hereditary Exostosis
Received:August 14, 2016
Accepted: August 26, 2016
Published online: September 10, 2016
@ 2016 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY license. http://creativecommons.org/licenses/by/4.0/
1. Introduction
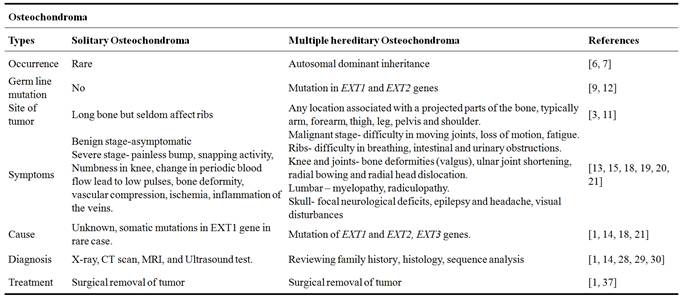
The term osteochondroma is originated from ancient Greek literature (ostoun: bone, chondros: thick, soft bone, cartilages in the region between the ribs and navel, oma: suffix denoting state of mass growth) which means ‘growth of bone and cartilage’. In the year 1891, the word ‘exostosis bursata’ was coined by Orlow to describe bursae developing between osteochondromas and surroundings soft tissues [1]. It is also known as osteocartilaginous exostosis and is a capped cartilage or ossein bony arising neoplasm on the external surface of bone containing a marrow cavity i.e., continuous underlining bone [2]. It arises in bones performed by endochondral ossification and the most usual site involved is the metaphyseal region of the longer bone of the limbs, like the distal femur, upper humerous, upper tibia and fibula [3]. Flat bones, specifically the ilium and scapula are the most common occurring area for ostochondroma. The observation manifest that the occurrence of this disease in male sex is predominance to female and the suggested ratio is 1.5:1. The first 3 decades of life has maximum chances of getting affected with osteochondroma and hardly occurs in craniofacial bones because of the fact that these bones are not formed by endochondral ossification [3,4]. Osteochondroma is not only the most common benign (not harmful in effect) bone tumor diagnosed incidentally and it contributes around 35% of benign bone tumors and 9% of all bone tumors. In many cases, it is asymptomatic but depending on location and size, it shows mechanical symptoms like pain, bone deformity and claudication (Table 1) [1, 5].
Table 1. Research progresses on study of osteochondroma in human.
2. Types of Osteochondroma
Solitary Osteocartilaginous exostosis of the cervical spine is rare phenomenon of usual bone tumor and the symptoms based on adjacent compression structure of the bone [6]. As a result patient suffering from osteochondroma affects the anterolateral C7 vertebrae of spinal cord. Solitary lesions are most common but multiple lesions are presented more usually with autosomal dominant inheritance and are termed as multiple exostoses [6,7]. Normally, long bones are the sites for osteochondroma but seldom affect ribs. Extension of the tumor necessitated total pediculectomy of T12, total facetectomy of T12-L1, and partial unilateral vertebrectomy of T12 with thoracolumbar fixation and fusion [3]. In middle-aged woman the causes like intraspinal extension, spinal cord compression are seen in case of solitary osteochondroma [6,9]. Mostly spinal osteochondromas or solitary lesions, usually affecting the lumbar segment and are rare tumors of maturing adolescent skeleton [6,7,8].
Hereditary multiple exostosis or Multiple hereditary exostoses (MHE), also known as multiple osteochondromatosis and are autosomal-dominant skeletal disorder which attacks nearly one in 50,000 counts [9,10]. In case of MHE, almost 96% of genetically heterogeneous disorder has been linked to mutations of the genes EXT1 and EXT2 [9,12]. Bony exostoses are the hallmark of multiple hereditary exostoses and have a widely variable clinical presentation [8,10]. Although they can appear at any location associated with projected parts of the bone, the lesions typically occur at the arm, forearm, thigh, and leg. They are also commonly found about the pelvis and shoulder. Patients often report problems resulting from compression or irritation of local tissues, deformation of joints, or limb-length discrepancies [11]. Complications of bony exostoses include compression of adjacent structures, such as nerves, blood vessels, and other soft tissues, leading to pain and sensory or motor deficits [6,10]. These symptomatic lesions often need surgical treatments [9,10]. Patients with MHE with minimal symptoms were discovered to have cervical spine stenosis and secondary to intracanal osteochondromas [12].
3. Symptoms
Most of the symptoms are fairly minor and in many cases they are symptomless or painless. Symptoms of osteochondroma are influenced only if tumor is pressing against another structure, in nerve or tendon. The common symptoms of osteochondroma include, a painless bump near joints, snapping sensation of overlying tendons, pain if the tumor is pressing on a nerve ending, usually present with painless hard mass which doesn’t move, neurovascular compression, lower than normal height for age, soreness of the nearby muscles, one leg and one arm may be longer than other, pressure or irritation while body movements [1].
Solitary osteochondroma does not show any symptoms for long period of time until tumor develops. The symptoms are painless bump (in shoulder and knee joints), pain developed during movement of bone in tendons (snapping activity), numbness found near the knee nerves, change in periodic blood flow rate due the presence of tumor on the blood vessels which lead to loss of pulses or change in limb color, injury of tumor lead to breakage in stalk of predunculated one cause pain and immediate swelling. In case of soft tissues, symptoms are due to direct mechanical mass effect. The major symptoms are fracture of the bone, bone deformity, vascular compression, arterial thrombosis, clotting of blood vessels (aneurysm), or pseudo aneurysm, discomfort or tiredness in the legs during walking (claudication), ischemia, inflammation of the veins [13].
In case of Multiple hereditary osteochondroma, the symptoms include difficulty in moving joints, loss of motion, fatigue due to irritation in muscles and tendons, motor and sensory difficulty caused by stretching and compression of nerve [15], tumor developed on ribs that causes difficulty in breathing, rare exostoses cause intestinal and urinary obstructions, limb and bone deformities like valgus (in knee it is known as knee valgus, in ankle as ankle valgus and hip as coxa valga), loss of function due to upper extremity deformities, ulnar joint shortening, radial bowing and radial head dislocation. Symptoms for lumbar osteochondroma are neurologic deficit in spinal cord (myelopathy), severe joint pains, radiculopathy (injury in nerve root) [18,19,20,21].
In case of skull osteochondroma, seen in skull base and non-skull base (found in the convexity and the falx). Symptoms in base of skull is focal neurological deficits and in non-skull base symptoms are epilepsy and headache in initial stage, visual disturbances, abducens nerve palsy are the most common cranial nerve deficit [17], bulging and hardened consistency will be increased [8], but they are painless, pain would be associated with complications of a mechanical origin that are promoted by the projection of hard tissue (bone) into the soft tissues. Multiple osteochondroma lead to malignant transformation [18].
4. Causes
As of now, the cause of osteochondroma is unknown, but the tumor thought to be related to an abnormality in the growth plate on the bone [1, 21]. A hereditary form of the disease may be related to one or more gene mutation. There are some possible causes like genetics, radiation treatment and injuries to the bone which are thought to lead to osteochondroma [14, 18]. There is a form that is inherited and a form that is not inherited. Inherited form a family member in a condition known as multiple hereditary osteochondromas, these frequently are identified earlier in childhood. It develops during childhood or adolescence, though they may not be noticed until adulthood. The reason for previous radiation is not entirely understood [15,16,17].
Genes involved in causing osteochondroma:
Hereditary multiple exostoses (HME) is known to be linked with three genes of mutations, EXT1, EXT2, EXT3. EXT1maps to chromosome 8q 24 [26], EXT2 maps to 11p13, and EXT3 maps to short arm of chromosome 19 [14]. In some cases, some families do not have any mutation in EXT1 and EXT2 genes, suggesting the involvement of other genes in the pathogenesis of the disease [24]. Many patients have an affected parent, while in some cases patients carry a de novo mutation. In almost all these cases the "mutation negative" patients do not have familial history for exostoses. EXT1 and EXT2 proteins are ubiquitously expressed transmembrane proteins which are heterodimers. On the contrary, in solitary osteochondroma, somatic mutations in EXT1 gene are rarely seen. These genes of mutations typically lead to the synthesis of truncated EXT protein which functions abnormally. These EXT proteins are important enzymes in the synthesis of Heparan sulfate [24,25].
Cause of solitary osteochondroma does not result from injury, both males and females are equally likely to develop [14, 16]. These are thought to be associated with gene EXT1. However, this tumor is currently poorly understood, with investigation still going on. Since the cause is unknown, physicians have not been able to find the way to prevent it [23].
Causes of multiple osteochondroma are mostly (70%) inherited from parents and 30% of cases occur randomly [14, 16]. It is also an alternation in genes EXT genes are thought to be the cause of this disease and research is being conducted.
Complications include osseous and cosmetic deformities, bursa formation, arthritis (14%) and impingement on adjacent nerves (22.6%), vessels (11.3%) or spinal cord (0.6%). Multiple osteochondroma does not have normal scar formation [14]. Osteochondromas bare the risk for fracture of the bony stalk during physical exercise. This is determined to occur in approximately 5% of osteochondromas [27] and may be the reason for surgical removal.
5. Diagnosis
Osteochondroma in benign stage does not cause any discomfort and is asymptomatic and is difficult to diagnose, but in certain case or incidently it is diagnosed when X-ray is carried out. The tests to diagnose the osteochondroma are X-ray [mostly done first], CT Scan, MRI, Ultrasound, Angiography, Sequence analysis, and biopsy [1].
X-ray is performed to characterize the tumor formed attached to the bone, the excess growth of bone would be observed. Plain radiography give only the charaterization of the tumor but classic radiography gives the position of the lesion, dense structure [1]. The tumor is observed like a flat or as stalk on the surface of bone, attached to tendons. Malignant tumors are found to be dense structure, irregularity, accumulation of calcium in bone will be scattered (calcification) in radiography (Figure 1. A) [28].
Computed Topography scanning (CT scan) are advised when tumor are found in pelvis, shoulder, and spinal cord. It diagnoses the thickness of the cartilage tumor, occurrence of calcification and difference between the osteochondroma and osteosarcroma [1]. It shows corticomedullary continuity of lesions, and its anatomy [29]. CT scan is performed before resection of tumor. PET-CT scan (Positron Emission Topography) is done in studying the osteochondroma transformation to sacromatous [30].
MRI (Magnetic Resonance Imaging) is used to predict morphology of the tumor, continuity with cortex of the affected bone, to observe vascular complication that occurred due to the tumor, to detect spinal column tumor, cartilage thickness, inflammation in bursa formation, detect the edema in bone, visualize the effect of tumor on the surrounding bone [28], dislocation, deformation and signal alternations in impingent syndromes (Figure 1. B).

Figure 1. A. Tumor like large cauliflower growing on knee arising from proximal fibula (anterior-posterior and lateral view) on plain radiograph [38]. B. Tumor on the distal femur viewed on MRI Scan [13].
Ultrasound (US) is performed to evaluate the cartilage cap and causes related to osteochondroma. Thickness of cartilage cap is determined, even bursa formation are easily recognized [30], detection of tumor by US is accurate than CT compared to MRI. The US detects the cartilage thin cap of benign tumor and thick malignant one [30]. During the tumor condition, ultrasound detects the low blood flow in lower leg dorsalispedis arteries [31], it visualizes the layers of the cartilage, as hypoechoic area on bone cortex which is usedfor studyingother complications such as aneurysms, thrombosis or bursitis [27].
Angiography is done to detect the vascular complications due to tumor in knee, compressed popliteal arteries [31]. Sequence analysis is the clinical test done to study the mutation in coding regions of both EXT1 and EXT2 and deletion analysis of genes [27,28]. Biopsy is also performed on tissue samples that can be tested for cancer.
Differential diagnosis are used to identify the malignant transformed osteochondromas like Dysplasia Epiphysealis Hemimelica (DEH, Trevor's disease, tarso-epiphysialaclasis) and metachondromatosis (MC) in both case of solitary(1%) and multiple hereditary(5-25%) [14]. It detects bone, cartilagionous, soft tissue tumors and cystic lesions. Subungal mass are diagnosed through Roentgenologic examination in differential diagnosis, cortical irregularity and popcorn-like calcifications [32].
MHE Diagnosis is done by reviewing the radiological documentation, histology, patient history and family history. Screening the germ line mutation of two genes by sequence analysis, MR imaging to detect the size of tumor, differential diagnosis are performed [14]. Solitary osteochondroma diagnosed by X-ray, CT scan, MRI, and Ultrasound test [1,28,29,30].
6. Treatment for Osteochondroma
It does not currently exist, but based on the asymptomatic or symptomatic complications there are few treatment which are followed, the mostly preferred/followed treatment is surgical removal of the bone, if they are malignant. There is no medicinal way of curing the tumor, but some commercial drugs are preferred by physician to relieve the pain which includes drugs like Analgesia [paracetamol, morphine], Acetaminophan, and Ibuprofen. If the tumor is malignant and pain exists for longer time, surgical treatment is done.
In treatment for solitary osteochondroma [benign tumor], no treatment for asymptomatic tumor is available, only careful observation of tumor is done by X-ray. In certain case like mechanical reasons or cosmetics reasons, the tumor is removed or operated [resection]. In case of prolong pain, pressure in nerve or blood vessel, formation of large cartilage cap, it can be ressected by process known as exicision, tumor is removed in benign stage [1].
In solitary osteochondroma, the surgical removal of tumor is done along with radiation therapy and chemotherapy,since the tumor is malignant. The lesions will extend from medullary bone, till beneath the bone. The resection should be complete, the incomplete removal leads to reccurences of the tumor and it will be malignant [1].

Figure 2. A. Tumor of lumbar spine removed by intra operation [20] and B. Tumor from iliac crest removed by surgery [55].
Excision treatment is the treatment of choice for symptomatic lesions like growth retardation, deformity of bone in limbs, spinal cord compression, compression of tendons or lesions of the soft tissue, even in some case like hereditary multiple exotoses, fractures, deformity (cosmetic and osseous) vascular compromise, neurologic sequelae, overlying bursa formation and malignant transformation, the surgical excision of bone and tumor is done [28].
Removal of mass tumor by surgery prevents the recurrence of tumor. The elective surgery is done, in case of benign tumor at high complication rate, most common complication are peroneal neurapraxias (periphery nerve in foot is affected), arterial breakage and fibula fracture (Figure 2. A-B) [33].
Removal of exotoses, epiphyseal arrest, resection of radial head and osteoeomy are performed frequently to cure the deformity and dislocation of radial head in 32 HME patients [34]. The malignant transformation of osteochondroma to chondrosarcoma is treated by surgery and limb salvage, MR Imaging gives structure of mass tumor, stage of tumor for surgery. In 30% of 45 patients, the chondrosacroma arise from osteochonroma [35]. Surgical treatment of symptomatic osteochondroma, 3 to 8 year follow up study in 86 patients found that about 93.4% of tumors are resolved after surgical treatment [13].
Surgical treatment of osteochondroma in pediatric about 3 to 8 years, exicision of both solitary and multiple osteochondromatosis, classified the tumor according to locations, in which 16 patients were having restricted finger motion / angulatory deformity [36]. HME with multiple osteochondromas of bone in young girl was found and the surgical exicision is performed to remove the tumor from spinal cord, cervical along with adjuvant radiotherapy [37]. Benign tumor with cartilage bone growth which is projecting outward from the affected bone is diagnosed by CT scan andis surgically operated and removed [38]. In few cases except MHE, tumor growth around the ankle (distal tibia osteochondroma) or on the lateral malleolus (outer side of ankle), can be benign or malignant, are completely removed by surgery to avoid the future occurrence in case of 13 year old female [39].
In most of the literatures, authors preferred the surgical treatment, if it is a symptomatic tumor, the complete excision would prevent reccurences which will be more malignant than the previous one.
A study was carried out by King et al (2014) on Osteochondromas after Radiation for Pediatric Malignancies. The objective of their study was to characterize osteochondroma in children. The study was related between the total body irradiation (TBI) and later development of osteochondroma in children who are treated with radiation therapy conditioning before Hematopoietic Stem Cell Transplantation (HSCT). During this survey identification, children from 1 to 18 years received an allogeneic HSCT and TBI from 2000 to 2012 from Blood and Marrow transplant (BMT) Database. According to the recent research from 1996 to 2012 in pediatric orthopaedic clinical records, osteochondroma patients were affected by radiation exposures. Children were most likely to develop osteochondroma after early exposure to radiation therapy, which may cause body aches and may require surgery. According to the research this was the first case reported on Radiation-induced osteochondroma causing lower extremity misalignment [40].
Research was done on Bone Morphogenetic Protein (BMPs) and their cognate receptors (BMPRs) expression in osteochondroma. The survey determines the movement and distribution of BMP-2/4,-6 and -7, BMP receptors BMPR-IA,-IB and -2, signal transuding proteins phosphorylated Smad I/5/8 and comparsion was done between bovine growth and articular cartilage. BMP-6, -7, BMPR-IA and BMPR-2 had same variations and movement in the cartilage cap and growth plate. BMP-2/4 and BMPR-IA was observed throughout growth plate. Research on BMPs states that differentiation of chondrocytes leads to unbalance of BMP-2/4 and noggin reaction forms an abnormal regulation of chondrocyte proliferation and differentiation in the cartilage cap of human osteochondroma [41].
For detail understanding of osteochondroma, experiments and research was done mouse model. According to researches, osteochondroma was caused due to bone mutational growth, which leads to severe body pain, still further researches are going on. Exostosin 1 and 2 mutated genes leads to Multiple Hereditary Exostoses (MHE) glycosyl transferases involves in biosynthesis which is responsible for promoting heparin sulphate (HS) chains. These affect the signalling pathway cycle, as further research is going on HS biosynthesis, MHE and interaction of osteochondroma as further survey and researches are going on to get a clear idea on osteochondroma using mouse model [42].
Costotransversectomy helps accessing the rib cage, pedicle, neural foramen and spinal canal. Osteochondroma affecting the neural foramen was rare bone mutation which leads to bone compression in spinal cord. Surgery proved better results which decompress the spinal cord and rearrangement of cartilaginous portion of the osteochondroma. The rearrangement of proved perfect outcome, obviate spinal stability and requirement of fusion [43].
Research was done by 12 specialist bone-tumor pathologists, reviewing 40 cases, they found that many cures for cartilaginous tumors by isolating osteochondromas at multiple sites and later validated previous cases and found difference between the osteochondroma, low and high grade secondary chondrosarcomas as well. After the Histopathological Diagnosis of Cartilaginous Tumors survey, the researchers found that osteochondroma formation was complicate since cartilage cap had less thickness compared to low and high grade secondary peripheral chondrosarcoma and came with the solution for diagnosis of tumors [44].
Bone-tumor pathologists treated 27 patients with age of 37 yrs. According to the survey, 23 cases were benign tumors (88%) (Tumor stage 1 to 3), 3 patients showed malignant changes (12%) (Stages IA - IIB). En Bloc treatment was given to patients by wide and marginal rearrangement and few patients treated with intralesional rearrangement. Surgical and EA (Enneking appropriate) surgical margin was successful and also the adjuvant therapy was not required. Recurrence was found in 2 patients having fixed spine and mobile spine and after therapy the risk of death was not observed [45].
In another study, research was based on the inactivation of osteochondroma active sites which prevent bone tumor without any surgery. Active site Ext1, DNA of interest was taken from cartilaginous cap of osteochondroma by method called laser capture micro dissection (LCM). Standard allele specific PCR was used and the analysis showed that osteochondroma consists of both recombined and intact alleles. The ratio between the recombined Ext 1F and intact Ext 1F vary in most samples. Mapping analysis by using mouse determined the research on Ext1-null chondrocytes to osteochondroma compound. The observation shows that osteochondroma complicated clonal growth of Ext1-null chondrocytes and there was variation in percentage of LacZ gene [46].
This is related to the bony pressure erosion in adults. It is caused due to the extrinsic pressure on the adjacent bones due to solitary and familiar forms. The individual experiences difficulty in walking and painlessness at the lateral portion of the knee. Radiographic studies revealed a large fibula osteocondroma of the knee and is associated with large fibular erosion. It is more likely to develop before skeletal maturity is reached [47].
The synovial osteochondroma and parosteal osteosacroma are rare musculo-sketetal tumors. The giant synovial osteochondroma is believed to originate from synovial chondromatosis and is localized in the vicinity of the knee. Physical examination showed a hard and tender mass. There were no inflammatory signs and shows limited range of motion. There were no symptoms such as during the rotation and in there was stability compression, and stability in the ligamentous structure. The radiograph analysis showed lobulated and fully calcified tumor which can be found mostly in intra-articulary in the vicinity of the hip joint and knee [48].
Osteochondroma is the most common benign bone tumor and the exophytic bone tumor is covered by a cap of cartilage. Metaphysis is the most commonly affected site. Neurologic symptoms and pain is developed due to compression. The recurrence of osteochondroma is rare. The most commonly resection tools used are flat chisel, a bone saw or wire saw. However the tool used to make complete resection of an osteochondroma in the metaphysic of a long bone is difficult because of the continuity of the osteochondroma. This is due to the anatomical concave shape of the metaphysic of the host bone. The use of curved chisel for transposition osteotomy of the acetabulum makes complete resection of osteochondroma in the long bone easier and reducing the possibility of malignant bone tumor development [49].
Vascular complications from osteochondroma are rare. There has been a report of intraoperative rupture of undiagnosed popliteal atery pseudoancurysm during resection surgery for distal femus osteochondroma vascular complications are infrequent. Acute rupture is rare, orthopedic and vascular surgery is undertaken when there is exostosic associated to false ancurysm [50].
A report on individual developed radial head dislocation with a progressive radius deformities which is caused by solitary osteochondroma which is originated from the proximal metaphysic of the radius. Radial head reduction and deformity correction was achieved after the tumor excision was performed, and the patient remained asymptomatic and regained a full range of motion [51].
There are several cases of osteochondroma originating from lumbosacral spine which is caused by radiculopathy. 4 cases were originated from the lumbar spine. A 57 year old individual after myelography showed high density mass with medullary continuity between the tumor and the vertebrate arising from right L4 inferior articular process, projecting into spinal canal. MRI showed a high intensity cancellous area in T2 weighed image [52].
Deep vein thrombosis is common condition which is caused by the impaired venous blood flow or hypercoagulate blood state. Deep vein thrombosis is formed in association with femoral osteochondroma and puplited artery pseudoanesurym. A 37 year old individual was admitted with symptoms such as acutely swollen, pain in right calf. On examination, the right calf was significantly swollen, hot, tense and tender. The knee showed full range of movement. The peripheral were nomal, but the popliteal vein was noted to be displaced laterally by an osteochondroma. Ultrasound scan of the popliteal fossa (diamond shaped depression located posterior to the knee joint) revealed a large pseudo aneurysm arising from the posterior aspect of the popliteal atery. The knee joint looked several femoral exostoses above the knee joint. The treatment for this is ligation of the popliteal artery and bypass grafting by using the long saphenous vein [53].
In chromosomes bands 12q14~15, visibly two cases of extrasketal osteochondroma were observed which were visibly rearranged through pericentric. The first tumor molecular analysis showed in two transcript express HMAG2. In second tumor fusion transcript in which 1-3 of HMAG2 were fused with intron 1 of SOX5 [54]. According to the researchers these are the work done so far on osteochondroma patients.
7. Conclusion
Most of the existing reports refer to complications arising from sizable osteochondroma in patients with MHE. Common reasons for resections of osteochondromas are compression symptoms, pain, and limited range of motion or suspected malignancy. Till now, the differential diagnosis like histological analyses have not resulted in clear diagnosis in all the stages of tumor. Therefore, surgical therapy with complete excision and narrow follow-ups are recommended until the complete recovery for the tumor. Chemotherapy, targeted therapy (drugs to target the certain genes in cancer cells) and radiation by beam of X rays can also be done to inhibit the growth of cancer cells as well as to prevent the recurrence of the tumor.
References
- Kitsoulis, P., Galani, V., Stefanaki, K., Paraskevas, G., Karatzias, G., Agnantis, J.N, and Bai, M. (2008).Osteochondromas: Review of the Clinical, Radiological and Pathological Features. In Vivo.vol.22 (5),pp.633–646.
- Hameed, S., Nak, M.A., Safderi.,H. and Rao, S.K. (2011).Prepubertal Presentation of Solitary Osteochondroma of Thoracic Spine– A Case Report. Malaysian Orthopaedic Journal.vol. 5(2), pp. 34-36.
- Shim, H.J., Park, K.C., Shi, H.S., Jeong, H.S. and Hwang, H.J.(2012). Solitary osteochondroma of the twelfth rib with intraspinal extension and cord compression in a middle-aged patient. BioMed Central Musculoskeletal Disorders.vol.13(57), pp. 1-6.
- Fukunaga, S., Futani, H. and Yoshiya, S.(2007).Endoscopically assisted resection of a scapular osteochondroma causing snapping scapula syndrome.World Journal of Surgical Oncology. vol. 5(37), pp. 1-7.
- Bovée G.M.V.J.(2010).EXTra hit for mouse osteochondroma.Proceedings of the National Academy of Sciences(PNAS).vol. 107 (5), pp. 1813–1814.
- Watura, C. and Patel, S. (2012). Unusual presentation of more common disease/injury-Osteochondroma mimicking deep vein thrombosis in a young cricketer.BioMed Central Case Reports.pp.1-3.
- Grivas, B.T., Polyzois, D.V.,Xarchas, K., Liapi, G. and Korres, D.(2005). Seventh cervical vertebral body solitary osteochondroma. Report of a case and review of the literature.European Spine Journal.vol.14, pp. 795–798.
- Natale, M., Rotondo, M,Avanzo, D.R. andScuotto, A.(2013).CASE REPORT Solitary lumbar osteochondroma presenting with spinal cord compression.British Medical Journal(BMJ) Case Report.pp. 1-4.
- Cory, M.,Czajka, M.D., Matthew, R. and DiCaprio, M.D. (2015).What is the Proportion of Patients With Multiple Hereditary Exostoses Who Undergo Malignant Degeneration?Clinical Orthopaedics and Related Research.vol.473, pp. 2355–2361.
- Kevin, B. and Jones, M.D.(2011). Glycobiology and the Growth Plate: Current Concepts in Multiple Hereditary Exostoses. Journal of Pediatric Orthopaedics.vol. 31 (5), pp.577–586.
- Xia, P., Xu, H., Shi, Q. and Li, D.(2016). Identification of a novel frameshift mutation of the EXT2 gene in a family with multiple osteochondroma. ONCOLOGY LETTERS.vol.11, pp. 105-110.
- Ashraf, A., Larson, A.N., Wetjen, M.N., Guidera, J.K., Ferski, G. and Mielke, H.C.(2013). Spinal stenosis frequent in children with multiple hereditary exostoses, Journal of Children's Orthopaedics. vol.7, pp. 183–194.
- Bottner, F., Rodl, R., Kordish, I., Winklemann, W., Gosheger, G. and Lindner, N. (2003).Surgical treatment of symptomatic osteochondroma. A three-to eight-year follow- up study. Journal of Bone and Joint Surgery. vol.85, pp. 1161-1165.
- Bovée, G.M.V.J. and Hogendoorn, P.C.W.(2008).Multiple Osteochondromas. Orphanet Journal of Rare Diseases,vol.3(3), pp. 1-7.
- Wicklund, C.L., Pauli, R.M., Johnston, D. and Hecht, J.C.(1995). Natural history study of hereditary multiple exostoses. American Journal of Medical Genetics,vol.55, pp. 43–46.
- Bozzola,M., Gertosio, C.,Gnoli, M., Baronio, F., Pedrini, E., Meazza, C. and Sangiorgi, L.(2015). Hereditary multiple exostoses and solitary osteochondroma associated with growth hormone deficiency: to treat or not to treat?.Italian Journal of Pediatrics,vol.41(53), pp. 1-6.
- Hongo, H., Oya, S., Abe, A.and Matsui, T. (2015). Solitary Osteochondroma of the Skull Base: A Case Report and Literature Review. Journal of Neurological Surgery Reports,vol.76(1), pp.13–17.
- Pannier, S.and Legeai-Mallet, L. (2008).Hereditary multiple exostoses and enchondromatosis. Best Practice & Research Clinical Rheumatologyvol. 22(1), pp. 45-54.
- Kadu, V., Saindane, A., Goghate, N. andGoghate. N. (2015).Osteochondroma of the Rib: a rare radiological appearance. Journal of Orthopaedic Case Reports, vol.5 (1), pp. 62-64.
- Rosa.B., Campos,P.,Barros, A.,Karmali, S., Ussene, E., Durão, C., Silva, D.A.J. and Coutinho, N.(2016).Spinous Process Osteochondroma as a Rare Cause of Lumbar Pain. Case Reports in Orthopedics, vol. 2016 (2016), pp. 1-4.
- Gaetani,P., Tancioni, F., Merlo, P., Villani, L., Spanu, G. and Baena, R.R.(1996). Spinal chondroma of the lumbar tract: case report. Surgical Neurology, vol. 46 (6), pp. 534–539.
- Peterson, H.A. (1989).Multiple hereditary osteochondromata. Clinical Orthopaedics and Related Research, vol.239, pp. 222-230.
- Adullah, F., Kanard, R., Femino, D., Ford, H. and Stein, J. (2006). Osteochondroma causing diaphragmatic ruputure and bowel obstruction in a 14 years old boy. Pediatric Surgery International, vol.22, pp. 401-403.
- Arai, T., Akiyama, Y., Nagasaki, H., Murase, N., Okabe, S., Ikeuchi, T., Saito, K., Iwai, T. and Yuasa, Y. (1999). EXTL23/EXTR1 alternations in colorectal cancer cell lines. International Journal of Oncology, vol.15, pp. 915-919.
- Clement, N.D., Duckworth, A.D, Baker, A.D. and Porter, D.E. (2012). Skeletal growth patterns in hereditary multiple exostoses: a natural history. Journal of pediatric orthopedics. Part B, vol. 21, pp. 150-154.
- Wicklund, L.C., Pauli, R.M, Johnston, D. and Hecht, J.T.(1995). Natural history study of hereditary multiple exostoses. American Journal of Medical Genetics, vol. 55, pp. 43-46.
- Cañete, P.M.D., Fontoira, M.E., José, S.G.B. and Mancheva, M.S. (2013).Osteochondroma: radiological diagnosis, complications and variants.Revista Chilena de Radiologia,vol.19 (2), pp. 73-81.
- Mark, D., Murphey, D.M., Choi, J.J., Kransdorf, J.M., Flemming, D.J. and Gannon, H.F.(2000).Imaging of Osteochondroma: Variants and Complications with Radiologic-Pathologic Correlation. AFIP ARCHIVES,vol. 20 (5), pp. 1407-1434.
- Purandare, N.C., Rangarajan, V., Agarwal, M., Sharma, A.R., Shah, S., Arora, A. and Parasar, D.S. (2009).Integrated PET/CT in evaluating sarcomatous transformation in osteochondromas.Clinical Nuclear Medicine, vol. 34(6), pp. 350-354. [pubmed]
- Malghem, J., Berg, B.V., Noel, H. and Maldague, B. (1992).Benign osteochondromas and exostoticchondro sarcomas: evaluation of cartilage cap thickness by ultrasound.Skeletal Radiology, vol.21, pp.33-37.
- Sakamoto, A., Tanaka, K., Matsuda, S., Harimaya, K. and Iwamoto, Y. (2002).Vascular compression caused by solitary osteochondroma: useful diagnostic methods of magnetic resonance angiography and Doppler ultrasonography. Journal of Orthopaedic Science, vol. 7 (4) pp. 439-443.
- Natale,M., Rotondo, M., D'Avanzo, R.and Scuotto,A.,(2013),Solitary lumbar osteochondroma presenting with spinal cord compression, British Medical Journal(BMJ) Case Report,Vol. 2013 (2013), pp. 1-4.
- Wirganowicz, P., Watts, Z. and Hugh, G.(1997). Surgical risk for elective excision of benign exostoses (tumors). Journal of Pediatric Orthopaedics, vol.17, pp. 455-459.
- Sharipo, F., Simon S. and Glimcber, M.J. (1979). Hereditary multiple exostoses. Anthropometric, Roentgenographic, and clinical aspects.The Journal of Bone & Joint Surgery, vol. 61, pp. 815-824.
- Canella, P., Gardin, F. and Borriani, S. (1981). Exostosis: development, evolution and relationship to malignant degeneration.Italian journal of orthopaedics and traumatology,Vol.7,pp. 293-298.
- Ohnishi, T.,Horii, E., Shukuki, K. andHattori, T.(2011). Surgical Treatment for Osteochondromas in Pediatric Digits. Journal of hand surgery, vol. 36(3), spp. 432-438.
- Landi,A.,Rocco, P., Mancarella,C., Tarantino, R. and Raco, A.(2012). Malignant transformation of cervical ostochondroma in patient with hereditary multiple exostoses (HME): Case report and review of the literature. Journal of Solid Tumors, vol. 2(3) pp.63-70.
- Kumar, M., Malgonde, M. and Jain, P. (2014).Osteochondroma Arising from the Proximal Fibula: A Rare Presentation. Journal of Clinical and Diagnostic Research.Vol.8(4) pp. 1-3.
- Herrera-Perez, M., Mendoza, D.A.M., Bergua-Domingo, D.M.J,and Pais-Brito, L.J. (2013),Osteochondromas around the ankle: Report of a case and literature review. International Journal of Surgery Case Reports, Vol. 4(11), pp. 1025–1027.
- King, A.E., Hamstra, A.D., Li, Y., Hanauer. A.D., C.hoi, W.S., Jong. N., Farley,AF.andCaird, S.M.(2014); Osteochondromas After Radiation for Pediatric Malignancies: A Role for Expanded Counseling for Skeletal Side Effects. Journal of Pediatric Orthopaedics, vol.34 (3), pp. 331–335.
- Cuellar, A.,Inui, A., James, A.M., Borys. M. and Reddi, H.A.(2014).Immunohistochemical Localization of Bone Morphogenetic Proteins (BMPs) and their Receptors in Solitary and Multiple Human Osteochondromas, Journal of Histochemistry & Cytochemistry, vol. 62(7), pp. 488–498.
- Cuellar,A.andReddi, H.(2013). Cell biology of osteochondromas: Bone morphogenic protein signalling and heparansulphates. International Orthopaedics Journal (InternationalSociety of Orthopaedic Surgery and Traumatology) vol. 37, pp.1591–1596.
- Mazur, D.M., Mumert. L.M. and Schmidt, H.M.(2015).Treatment of costal osteochondroma causing spinal cord compression by costotransversectomy: case report and review of the literature. Clinics and Practice Journal, vol. 5(734), pp.40-43.
- Andrea, D.E.C., Kroon, M.H., Wolterbeek, R., Romeo, S., Rosenberg, E.A., Young, D.R.B., Liegl, B., Inwards, Y.C., Hauben, E., McCarthy, F.E, Idoate, M., Nicholas, A., Athanasou, A.N. and Jones, B.K.(2012).Interobserver Reliability in the Histopathological Diagnosis of Cartilaginous Tumors in Patients with Multiple Osteochondromas. Modern Pathology Review,vol. 25(9), pp. 1275–1283.
- Sciubba, M.D., Macki, M., Germscheid, M.B., Wolinsky, P.J., Boriani, S., Bettegowda, C., Chou, D., Luzzati, A., Reynolds, J.J., Szövérfi, Z., Zadnik, P., Rhines, D.L., Gokaslan, L.Z., Fisher, G.C., Varga, P.P., Hogendoorn, W.C.P and Bovée, G.M.V.J.(2015). Long-term outcomes in primary spinal osteochondroma: a multicenter study of 27 patients. Journal of Neurosurgery: Spine, vol, 22 (6), pp.582–588.
- Matsumotoa, K., Iriea, F., Mackemb, S. and Yamaguchia, Y. (2010),A mouse model of chondrocyte-specific somatic mutation reveals a role for Ext1 loss of heterozygosity in multiple hereditary exostoses. Proceedings of the National Academy of Sciences(PNAS), vol. 107 (24), pp. 10932 – 10937.
- Davis, L.D. and Mulligan, E.M.(2015.Osteochondroma-Related Pressure Erosions in Bony Rings Below the Waist.The Open Orthopaedics Journal, vol. 9, pp.20-524.
- Toepfer, A., Pohlig, F., Mühlhofer, H., Lenze, F., Rothe, E.V.R. and Lenze, U.(2013).A popliteal giant synovial osteochondroma mimicking a parosteal osteosarcoma. World Journal of Surgical Oncology, vol.11(241), pp.1-7.
- Sakamoto,(2013).Usage of a Curved Chisel When Resecting Osteochondroma in the Long Bone.Clinics in Orthopedic Surgery, vol.5, pp. 87-88.
- Hajji, R., Jiber, H., Zrihni, Y., Zizi, O. Bouarroum, A.(2013),Case report Intraoperative rupture of popliteal artery pseudo aneurysm secondary to distal femur osteochondroma: case report and review of the literature,Pan African Medical Journal.pp.1-3.
- Niu,F.X., Yi. H.J., Hu, J. and Xiao, B.L. (2015) Chronic radial head dislocation caused by a rare solitary osteochondroma of the proximal radius in a child: a case report and review of the literature. BioMed Central Research Notes, vol. 8:131, pp.1-4.
- Kuraishi, K., Hanakita, J., Takahashi, T., Watanabe, M. and Honda, F., (2014). Symptomatic Osteochondroma of Lumbosacral Spine: Report of 5 Cases.Neurologia medico-chirurgica Journal(Tokyo),vol.54, pp.408–412.
- Scott, E,M., White, F.J. and Jennings, P,E. (1995),Popliteal vein thrombosis associated with Femoral osteochondroma and popliteal artery pseudoaneurysm. pp.441-442.
- Panagopoulos, I., Bjerkehagen, B., Gorunova, L., Taksdal, L. and Heim, S. (2015).Rearrangement of chromosome bands 12q14~15 causing HMGA2-SOX5 gene fusion and HMGA2 expression in extraskeletal osteochondroma.ONCOLOGY REPORTS,vol. 34, pp,577-584.
- Pal, P. and Chatterjee, G.(2015).Giant Solitary Osteochondroma of Iliac Crest - a Case Report.
- International Journal of Scientific Research(IJSR), vol.5: 3, pp.199-201.