Transcutaneous Implants in a Porcine Model: The Use of Highly Porous Tantalum
Ronald Hugate1, *, Rhonda Clarke2, Tim Hoeman3, Andrea Friedman4
1The Denver Clinic for Extremities at Risk at Presbyterian/St. Luke’s Medical Center, Denver, Colorado, USA
2Zimmer Biologics, Austin, Texas, USA
3Product Development and Global Brand Management, Zimmer Trabecular Metal Technology, Parsippany, New Jersey, USA
4Zimmer Trabecular Metal Technology, Parsippany, New Jersey, USA
Abstract
Porous tantalum has long been used in orthopedics for enhanced bone in-growth. The purpose was to evaluate soft tissue integration into transcutaneous porous tantalum implants. Eighteen porous tantalum and four solid titanium implants were placed within and passed through the subcutaneous tissues of swine. They were harvested after six weeks and examined microscopically to evaluate epidermal contact, soft tissue penetration into and onto the implant, and inflammation. Fifteen of sixteen porous implants demonstrated both soft tissue and vascular tissue penetration. Nine of sixteen porous implants demonstrated epidermal contact with the transcutaneous portion of the implant. A score of 0-4 was used to describe tissue ingrowth (0=none and 4=100%). Soft tissue penetration score averaged 1.25 at the post and 2.63 at the base of the implant. Vascular tissue penetration score averaged 1.0 at the post and 2.63 at the base. Inflammation was evaluated and scored from 0-4 (0=none and 4=marked inflammation). Acute inflammation was present in six of sixteen porous implants with an average score of 1.88 at the transcutaneous post and 0.81 at the subcutaneous implant base. Chronic inflammation was present in every porous implant with a mean score of 1.5 at the post and 1.56 at the base. Three of the four solid titanium implants extruded during the study. The one surviving implant did not demonstrate any epidermal contact on the implant post or tissue ingrowth with chronic and acute inflammation scores of 2 at the base. Porous tantalum transcutaneous implants experienced epidermal, soft tissue, and vascularized tissue adhesion and integration with minimal inflammation. This finding may help prevent deep infection in transcutaneous implants.
Keywords
Transcutaneous Implants, Highly Porous Tantalum, Implant Infection Prevention
Received: March 6, 2015 / Accepted: March 21, 2015 / Published online: May 11, 2015
@ 2015 The Authors. Published by American Institute of Science. This Open Access article is under the CC BY-NC license. http://creativecommons.org/licenses/by-nc/4.0/
1. Introduction
Implantable prosthetic devices have been a mainstay in the treatment of orthopedic problems for decades. Joint replacements are just one example. They have improved the quality of life of millions around the world. The durability and function of these implants are excellent and the complication rates are relatively low [2,8].
Efforts in the development of safe and effective transcutaneous implants, however, have not been as successful. Although implantable transcutaneous prosthetics could be of value (for example to the world’s amputee population), issues with infection originating at the skin/implant interface that subsequently permeate proximally into the bone/implant interface have precluded their routine use in the general population. Infection rates of up to 18% in healthy selected individuals who have received transcutaneous prostheses have been reported [16,21,22].
A number of strategies have been employed and are under current investigation as it relates to prevention of infection at the skin-implant interface with variable results. The use of topical antimicrobials, surface texturing, mechanical stabilization of the skin interface, and surface coatings are reported in the literature [4,15,19]. There have been few reports however, on the use of highly porous tantalum, and what limited reporting that is available is in a non-analogous rabbit skin model [19].
In an attempt to reduce the incidence of deep infection in transcutaneous implants, this study investigates the use of highly porous metal as a soft tissue in-growth medium to help create a ‘biologic barrier’ against infection at the skin/implant interface. A newer generation of highly porous, open cell ‘foam’ materials may hold some theoretic advantage in creating a vascular environment at the skin/implant interface.
One such technology is highly porous tantalum (Trabecular Metal™ material or TM). This material is relatively inert and can be manufactured up to 80% porous by volume with open interconnecting dodecahedral shaped cells, allowing for rapid ingrowth of tissues. Tantalum is one of the most inert metals known to science. Tantalum is both biocompatible and corrosion resistant due to the chemical stability and tenacity of its natural surface oxide. When exposed to air, tantalum forms a very dense oxide layer (Ta2O5) which protects the base material from aggression. Tantalum’s oxide layer also does not denature proteins, producing an increasingly cellular and decreasingly fibrous reaction, which is a more vital response. TM has already been used for over a decade reliably on the bone ingrowth surfaces of orthopedic implants [6,7]. An interesting characteristic of highly porous materials is that when the cells are filled with living tissues, the implants become more biologic tissue (80%) than foreign material (20%). The resulting 80% living, vascularized implant should then theoretically hold an advantage against its solid metal counterpart in defending against infection because of this permeating biological tissue.
The objective of this study was to evaluate the interaction of the soft tissues and the degree of inflammation present when porous tantalum transcutaneous implants are implanted in the subcutaneous tissues of swine. The porcine model was chosen due to the analogous skin structure that swine share with humans. Specifically we ask the questions: Do the soft tissues permeate the porous tantalum implants, and if so to what degree? If so, do we see chronic and acute inflammation in or around the implants in the short term and in what depth patterns? A secondary goal of this study was to evaluate the soft tissue interaction with similarly sized solid titanium implants without porous tantalum material.
The authors hypothesized that the percutaneous porous tantalum implants would demonstrate soft tissue integration with the cutaneous and subcutaneous tissues at the interface providing a stable implant that is infiltrated with biologic materials and potentially more resistant to infection. In addition, we hypothesized that the degree of inflammation present would decrease with depth relative to the implant/skin interface.
2. Materials and Methods
Two groups of implants consisting of 18 porous tantalum implants and 4 solid titanium alloy implants were used in this study. The porous tantalum implants consisted of a 10mm tall by x 9mm diameter cylindrical percutaneous porous tantalum upright post with a solid 5mm diameter titanium alloy core atop a 5mm thick x 25mm diameter discoid porous tantalum base. The structure of the porous tantalum used was 80% porous with dodecahedral interconnecting cells. The average open pore diameter was 450um. Control implants consisted of polished solid titanium alloy with same outer geometry as the porous tantalum implants (Figure 1).
Four domestic female Yorkshire Cross-bread Swine, each at least 12 weeks of age and between 35-45kg in weight, were procured for use in this study. The animals were continuously housed at the research facility (MPI Research Facility, Mattawan, Michigan) and supervised by licensed veterinarians. The animals were each designated as healthy and fit for participation by the supervisory veterinarians upon arrival at the facility.
On day zero of our study, the animals were taken to a sterile operating theater. Each of the animals received perioperative antibiotics (preoperative dose of Cefazolin followed by 3 doses of IV Ceftiofur post-operatively) and was anesthetized with routine general anesthetics as outlined in our study protocol. Once anesthetized, the animals were placed in the prone position and the dorsum of the animals was shaved, prepared, and draped in a sterile fashion using Chlorhexadine skin preparation.
A total of 18 porous tantalum implants (6 per animal) were placed in the dorsal subcutaneous tissues of the three test animals designated 802, 804, and 806. Animal 805 received the 4 solid titanium alloy implants. In each animal, transcutaneous implants were placed at equally spaced intervals parallel to the spine caudal to the level of the scapulae and cranial to the level of the iliac crests. Implants were placed at least 5 cm off the midline and spaced at least 10 cm apart longitudinally.
First, a circular defect through the skin was created using a 9mm dermal punch at each pre-designated implant site to permit transcutaneous penetration of the implant post. Skin incisions were then created extending away from both ends of the circular defect by 1 cm in each direction parallel to the spine. A subcutaneous pocket was created by blunt finger dissection down to the level of the dorsal muscular fascia. The assigned implant was placed into each pocket with the base placed deep abutting the fascia and the post protruding percutaneously (Figures 2, 3). Once the implant was in position, the incision was closed with full thickness nylon sutures to approximate the edges of the longitudinal incision and ‘cinch up’ the skin against the implant post. The implant sites were dressed in a sterile fashion (Figure 4).
Post-operatively, animals were single housed in runs with ample Aspen wood shavings and plexi-glass covering the chain link fencing, to prevent the animals from rubbing the externalized implants against the caging. Post-operative monitoring of the implant sites was conducted through Day 10-14, based on healing at the tissue-implant interface. Implant sites were bandaged Day 0-7 post-operatively with Xenofoam, dry, clean gauze, and VetWrap, or other suitable covering. Discontinuation of dressings was dependent on wound closure and healing around the implant post. Implant sites were cleaned daily. Dirt, debris, and dried exudates were wiped off the implants using clean gauze. Implant sites were then cleaned with chlorhexadine solution. Following cleansing, each implant site was then dried completely with gauze. Implant sites were each photographed weekly.
At the termination of the study (Day 42 ± 1), all animals were euthanized and the implant sites (18 porous tantalum implants and 4 solid titanium implants) were photo-documented and excised along with the surrounding soft tissues (Figure 5). Each specimen was embedded in plastic (Technovit 7200 VLC) and sectioned through the approximate longitudinal mid-line of the defect site. One ground and polished section was then created from each plastic block. All sections were stained with hematoxylin and eosin (H&E) and assessed microscopically for epidermal contact, depth of penetration of soft tissues into the implant, acute and chronic inflammation, and depth of demonstrable vascular invasion by a board certified veterinary pathologist.
Microscopic observation of epidermal contact with the implants was assessed as 0 if no contact was present, 1 if contact was present on one side of the implant post, and 2 if contact was present on both sides of the implant post.
The depth of penetration of soft tissue and vascular tissue through the porous tantalum on the implant post was assessed using a ‘penetration score’ of 0-4, where 0 = no penetration; 1 = penetration of 1-25% of the distance to the titanium post; 2 = penetration of 26-50% of the distance to the titanium post; 3 = penetration of 51-75% of the distance to the titanium post; and 4 = penetration of 76-100% of the distance to the titanium post.
A penetration score was also assigned to each implant at the implant base. The depth of penetration of soft tissue and vascular tissues into the implant base was scored on a scale of 0 to 4. No penetration was given a score of 0; penetration confined to the periphery of the implant was given a score of 1; penetration to the center of the implant was given a score of 4; scores of 2 and 3 denoted penetration to areas intermediate to the peripheral and central areas.
Chronic and acute inflammation were assessed and scored at both the post and base portions of the implants. Inflammation was assessed a score of 0-4, where 0 = finding not present, 1 = minimal, 2 = mild, 3 = moderate, and 4 = marked. Direct observation of bacterial invasion was impossible to assess based on the methods of fixation of the specimens in this study and therefore could not be measured reliably.
3. Results
All animals survived to study termination. Sixteen of the eighteen (88%) porous tantalum implants completely integrated with the surrounding soft tissues and were present in the operative sites at the time of study conclusion. One of the eighteen porous tantalum implants partially extruded and one completely extruded from the operative site Three of the four solid titanium implants completely extruded during the course of the study with only one remaining in situ.
Direct epidermal contact was found to be present in nine of the sixteen porous implants (56%) at the skin/post interface. Of the nine implants in which skin contact was observed, seven exhibited contact with the epidermis on both sides of the implant post while two showed unilateral contact. Each of the implants that did not exhibit direct dermal contact, did exhibit soft tissue ingrowth as described below. At the sites in which epidermis contacted the post, the epidermis grew to the outer edge of the trabeculae, but did not penetrate the pores (Figure 6). The only remaining solid titanium implant did not exhibit any dermal contact features microscopically (Figure 7).
We assessed the degree of soft tissue penetration into the implants. Soft tissues permeated fifteen of the sixteen (94%) porous tantalum implants. This soft tissue in-growth occurred in the post portion of the porous tantalum implant in six of sixteen (38%) implants and in the base portion in fifteen out of sixteen porous tantalum implants (94%). A soft tissue penetration score was assigned to each implant based on the scoring scheme described in the methods portion of this manuscript. The mean soft tissue penetration score at the porous tantalum post was 1.25 (Range 0-4, STD 1.81) and for tissues permeating the base was 2.63 (Range 0 to 4, STD 1.54). Soft tissue penetration was not seen in the solitary surviving solid titanium implant.
Regarding vascular permeation into the implants, fifteen of sixteen (94%) of the porous tantalum implants exhibited some degree of vascular permeation. The depth of ingrowth was measured using the same penetration score as that for soft tissue ingrowth. Most permeation occurred within the base where 94% of the bases experienced vascular ingrowth with a mean score of 2.63 (Range 0 to 4, STD 1.54). Five of the sixteen porous tantalum implants exhibited vascular ingrowth at the post level with a mean penetration score of 1.0 (Range 0 to 4, STD 1.63). There was no vascular permeation present in the sole solid titanium implant examined (Table 1).
Acute Inflammation (AI) was also evaluated in the retrieved implants both at the level of the post and at the level of the base. The degree of AI was scored on a scale from 0-4 as defined in the methods portion of this manuscript by the observing pathologist. Some degree of AI was found to be present at the post/soft tissue interface in all porous titanium implants with a mean score of 1.88 (Range 0 to 3, STD 0.72). AI was also found to be present in six out of sixteen porous tantalum implant bases (38%) with a mean score of 0.81 (Range 0 to 3, STD 1.22). In the only solid titanium implant, there was no acute inflammation at the post and the acute inflammation present at the base was scored 2.
Chronic inflammation (CI) was scored and recorded in a similar fashion using the same scheme as that for acute inflammation by the observing pathologist. CI was present at the post implant interface in fifteen of sixteen (94%) porous tantalum implants with a mean score of 1.5 (Range 0 to 3, STD 0.73). CI was also present in every base with a mean score of 1.56 (Range 1 to 3, STD 0.81). Chronic inflammation was not seen at the post of the sole solid titanium implant and was scored as a 2 at the base (Table 2).

Figure 1. Photograph of the porous tantalum implant and the solid titanium implant side by side.
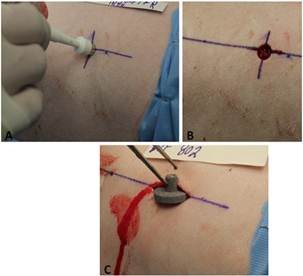
Figure 2. a: Photograph of Implant technique: a 9mm dermal punch is usd to create a full thickness circular skin defect. b: Photograph of Implant technique: the circular skin defect is extended using a scalpel 1cm cephalad and 1 cm caudad. A pocket is then created by bluntly dissecting down to the level of the dorsal muscular fascia. c: Photograph of Implant technique: Once the pocket is prepared, the implant is then placed within the pocket and the edges approximated with nylon sutures.
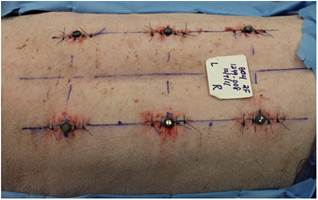
Figure 3. Photograph of the dorsum of the animal subject after implants have been placed showing the spacing scheme. They are each 5 cm off the midline and placed cephalad to the iliac crest/ caudal to the scapulae. Implant centers are spaced apart longitudinally by 10 cm.
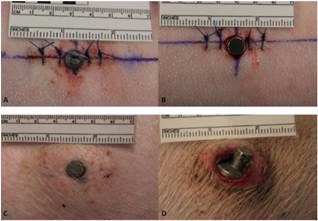
Figure 4. A: Photograph of implanted porous tantalum implant. B: Photograph of implanted solid titanium implant. C: Photograph of a porous tantalum implant at 42 days. D: Photograph of a solid titanium implant at 42 days. 3 of the 4 solid implants extruded prior to necropsy.
Figure 5. A: Animal 804, site 4. H&E stain at low power. A typical porous tantalum implant. The epidermis (E) grew up to the trabeculae of the post on both sides but did not penetrate into the pores. Trabecular pores of the base portion of the implant contain vascularized connective tissue or loosely arranged fibrin-like material. There was a mild amount of fibrous connective tissue (FCT) surrounding the implant base, except where portions of the base contacted the underlying muscle. B: Animal 804, site 4. H&E stain at high power (100X). A higher magnification photo at the post/base intersection. This shows epidermal contact with the porous tantalu. C: Animal 806, site 3. H&E stain at high power (100X). A typical cross section near the base/post interface in an in-grown porous tantalum implant. The epidermis is in contact with the deep implant post. Vascularized connective tissue (*) fills the pores of the tantalum implant.
Figure 6. A: Animal 805, site 1. H&E stain at low power. This is the sole surviving solid titanium implant. The implant is not in direct contact with the epidermis or dermis. The subcutaneous tissue is in contact with the base portion of the implant at the superficial corners and along the deep aspect of the base of the implant. The subcutis contains fibrous connective tissue (F) and mild inflammation (I). B: Animal 805, site 1. H&E stain at high power (100X). A higher magnification photo at the interface between the solid titanium and the surrounding tissues showing accumulation of neutrophils (N) and mononuclear cells (M) in the subcutis adjacent to the base portion of the implant. Note the gap (G) between the implant (IM) and the subcutis. C: Animal 802, site 4. H&E stain at low power. Some of the porous tantalum implants experienced epidermal down-growth such that the epidermis (E) contacted the base directly rather than the post. Most of the pores of the base portion of the implant are filled with vascularized connective tissue. Fibrous connective tissue (FCT) was present in the dermis adjacent to the implant on 3 sides. D: Animal 802, site 1. H&E stain at high power (100X). High magnification photo of the epidermal /dermal junction with porous tantalum implant post. Note the neutrophils (N) which are positioned superficial to the epidermis (E) showing a ‘barrier’ effect against inflammation of the soft tissues along the post of the implant.
Table 1. Soft tissue and vascular tissue penetration scores for porous tantalum implants. A measure of penetration to the solid core of the post or the center of the base. 0= no penetration, 1=25% penetration depth, 2=50% penetration depth, 3=75% penetration depth, 4=100% penetration depth. The solid titanium implant did not exhibit any soft tissue or vascular tissue penetration.
| Vascular Penetration Score | ||||
| Implant ID | Post Level | Base Level | Post Level | Base Level |
| 802-1 | 4 | 4 | 2 | 4 |
| 802-2 | 0 | 1 | 0 | 1 |
| 802-3 | 0 | 1 | 0 | 1 |
| 802-4 | 0 | 4 | 0 | 4 |
| 802-5 | 0 | 2 | 0 | 2 |
| 802-6 | 0 | 1 | 0 | 1 |
| 804-1 | 4 | 4 | 4 | 4 |
| 804-2 | 4 | 4 | 4 | 4 |
| 804-3 | 4 | 4 | 4 | 4 |
| 804-4 | 0 | 1 | 0 | 1 |
| 804-5 | 0 | 1 | 0 | 1 |
| 804-6 | Extruded | Extruded | Extruded | Extruded |
| 806-1 | Extruded | Extruded | Extruded | Extruded |
| 806-2 | 0 | 4 | 0 | 4 |
| 806-3 | 0 | 4 | 0 | 4 |
| 806-4 | 3 | 4 | 2 | 4 |
| 806-5 | 1 | 3 | 0 | 3 |
| 806-6 | 0 | 0 | 0 | 0 |
| Mean | 1.25 | 2.625 | 1 | 2.625 |
| STD | 1.807 | 1.544 | 1.633 | 1.544 |
Table 2. Acute and chronic inflammation scores in the porous tantalum implants. A measure of intensity of inflammation at the stem and base levels. Microscopic findings in the dermis and subcutis were assessed on a scale of 0-4, where 0 = no inflammation, 1 = minimal inflammation, 2 = mild inflammation, 3 = moderate inflammation, and 4 = marked inflammation.
| Chronic Inflammation Score | ||||
| Implant ID | Post Level | Base Level | Post Level | Base Level |
| 802-1 | 2 | 0 | 1 | 1 |
| 802-2 | 3 | 0 | 1 | 1 |
| 802-3 | 2 | 0 | 2 | 1 |
| 802-4 | 2 | 1 | 2 | 1 |
| 802-5 | 1 | 0 | 0 | 1 |
| 802-6 | 3 | 0 | 1 | 1 |
| 804-1 | 1 | 0 | 1 | 1 |
| 804-2 | 2 | 0 | 2 | 1 |
| 804-3 | 2 | 0 | 1 | 2 |
| 804-4 | 1 | 0 | 1 | 1 |
| 804-5 | 1 | 3 | 3 | 3 |
| 804-6 | Extruded | Extruded | Extruded | Extruded |
| 806-1 | Extruded | Extruded | Extruded | Extruded |
| 806-2 | 3 | 3 | 2 | 2 |
| 806-3 | 2 | 0 | 2 | 1 |
| 806-4 | 2 | 1 | 2 | 2 |
| 806-5 | 1 | 2 | 1 | 3 |
| 806-6 | 2 | 3 | 2 | 3 |
| Mean | 1.875 | 0.8125 | 1.5 | 1.5625 |
| STD | 0.719 | 1.223 | 0.73 | 0.814 |
4. Discussion
The development of safe and effective percutaneous implants holds the potential to improve the lives of millions of amputees worldwide. The recent wars in Iraq and Afghanistan have added to the numbers of young, healthy, and previously active amputees. With advances in center of mass protection, battlefield injuries have become more survivable, but have unfortunately yielded more combatants with loss of limb [1,5]. Many injured combatants wish to return to active duty and continue the fight despite their injuries.
The predominant method of prosthetic fitting and attachment in amputees has long been the molded socket. Using this method, the residual limb is casted, and a custom molded socket interface is created and placed around the residual limb with a distal attachment point for the external prosthetic device. This technology dates back hundreds of years and, with the exception of changes in materials and techniques, has changed relatively little over that time. This is an expensive and perpetual process over the life of the amputee as their body shape and residual limb go through constant changes [13]. While for some patients, this provides an acceptable interface, depending on the location of the amputation and the body type of the individual, socket technology can have its limitations.
As an example, energy transfer is extremely inefficient with the current socket technology- especially in patients with above the knee amputations (AKA). In this subgroup, it takes a single leg amputee up to 50% more energy to perform the same task as a well-bodied individual and up to 250% more energy in double amputees at this level [7,20]. This is mostly due to the depth of the soft tissues that typically surrounds the femur and the energy lost in transferring motion from an amputees femur, through these soft tissues, and then on to the prosthetic socket and eventually the prosthesis itself.
Maintaining fit can also be an issue with the amputee population using traditional socket technology. The average individual fluctuates in weight over his adult lifetime by up to 10% [23]. Weight fluctuation of this magnitude can make a socket so loose it will fall off or so tight that it creates pressure and skin breakdown. In addition, active amputees who perspire can have difficulty with adherence of their prosthetic sockets. There is also a subgroup of amputees who have skin breakdown issues related to anything from skin conditions to underlying heterotopic bone [6,10,14]. Each of these issues would become irrelevant if there were a safe, reliable, percutaneous skeletal attachment available to amputees.
Although percutaneous implants have been used for many years in the treatment of amputees in Europe, infection remains an issue [16,21,22]. Unlike traditional prosthetic devices (such as hip and knee replacements which are implanted completely below the dermal barrier) transcutaneous prostheses, by definition, are exposed to the outside world and the exposed portion inevitably becomes colonized with bacterial flora. When that flora is allowed to migrate along the implant, it eventually infects the bone/implant interface causing deep-seated osteomyelitis and implant loosening.
Various surface coating and texturing strategies have been employed in an effort to reduce the transmigration of bacteria along the implant’s skin interface with some success. Puckett et al [18] have demonstrated that nano-texturing the surface of titanium alloy results in increase keratinocyte function (adhesion and spreading). Salinized fibronectin has also been found to promote adhesive surface cell alignment in vivo alone and when combned with hydroxyapatite coatings [4].
Antimicrobials have been investigated as well. The topical antimicrobial ceragenin was applied via an impregnated pad at the skin-implant interface of transcutaneous implants in sheep, but when compared to controls at 24 weeks, there was no advantage relating to prevention of infection [17]. Topical 1% pexiganan acetate was applied daily to a percutaneous implant in a rabbit model and was found to reduce int incidence of infection by up to 75% when compared to controls at 24 weeks [19].
Other authors have advocated mechanical stabilization of the skin interface as a method to promote skin adhesion and prevent infection. This has led in part to design elements with porous subcutaneous flanges which have been used with success in Europe [9,15].
A critical element of this study was to demonstrate that soft tissues in and below the skin can effectively integrate themselves into porous tantalum implants. The authors believe that the most effective defense against infection is biologic tissue adhesion and apposition. Biologic tissues have an inherent mechanism to defend against infection: the white blood cell. The vascularity within biologic tissues can also deliver antibiotics (if necessary) to sites of potential infection. We believe that by introducing vascularity into the implant, we can harness the body’s ability to defend against infection at the skin/implant interface, creating an effective barrier against deep infection, and increasing the likelihood of successful long-term transcutaneous implant survivability.
Each study has its strengths and weaknesses and ours is no exception. The strength of this study is that it demonstrates effective, consistent soft tissue and vascular penetration into porous tantalum implants with minimal inflammation in a skin structure model analogous to that of humans. Rather than being encapsulated and extruded as foreign materials usually are, the vast majority of the porous tantalum implants integrated with the tissues, becoming a part of them.
This study does not address a bone/implant interface as this will be addressed in future studies. Because there was no bone/implant interface, these implants lacked a stable base and therefore were subjected to small amounts of motion, which may have affected their ability to more fully in-grow. Although we contemplated starting our investigations in this model with a transcutaneous osse-ointegrated implant, our goal was to focus on the skin-implant interface here and prove the viability of this concept before moving on to add other elements such as osseous integration and reduction of infection - which we believe we have achieved.
We were also unfortunately unable to directly compare the porous tantalum implants to the solid implants due to the fact that three of the four solid implants extruded during the study leaving us only one solid implant to analyze. This made it impossible to provide meaningful statistical comparison. However, we do believe that this further demonstrates the advantage of porous materials over solid materials.
5. Conclusions
In this study, highly porous tantalum implants have demonstrated their ability to incorporate with soft tissues at the level of the dermis and subcutis. This finding may be important in improving a transcutaneous implant’s ability to resist retrograde migration of bacteria and subsequent infection in the long term. Further studies are required in an amputee model to better understand this process when it is coupled with a strong implant/bone base.
Conflict of Interest Statement
One or more of the authors (RH) is a research consultant for Zimmer, Inc.- manufacturers of porous tantalum ‘Trabecular Metal’ material used in this study.
One or more of the authors (TH, RC, AF) is employed by Zimmer, Inc.- manufacturers of porous tantalum ‘Trabecular Metal’ material used in this study.
This research study was funded by Zimmer, Inc.- manufacturers of porous tantalum ‘Trabecular Metal’ material used in this study.
Each author certifies that he or she has or may receive payments or benefits from a commercial entity related to this work.
Ethical Review Committee Statement
The study protocol used in this study was reviewed and approved by the IACUC (Institutional Animal Care and Use Committee) at MPI research laboratories (54943 North Main Street Mattawan, MI 49071-8353 U.S.A) under protocol number 1249-008 in November 2011.
Statement of Location of Work
This study was conducted entirely at MPI Research, Inc. 54943 North Main Street Mattawan, Michigan 49071-8353. The veterinary pathology services were provided by Vet Path Services, Inc. (VPS) 6450 Castle Drive Mason, OH 45040.
References
- Belmont PJ Jr, McCriskin BJ, Sieg RN, Burks R, Schoenfeld AJ. Combat wounds in Iraq and Afghanistan from 2005 to 2009. J Trauma Acute Care Surg. 2012; 73(1):3-12.
- Bjørg-Tilde S Fevang,Stein A Lie,Leif I Havelin,Lars B Engesæter,Ove Furnes. Improved results of primary total hip replacement. Acta Orthop. 2010; 81(6): 649–659.
- BobynJD,StackpoolGJ,HackingSA,TanzerM,KrygierJJ. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br. 1999; 81-B(5): 907-14.
- Chimutengwende-Gordon M, Pendegrass C, Blunn G. Enhancing the soft tissue seal around intraosseous transcutaneous amputation prostheses using salinized fibronectin titanium alloy. Biomed Mater 2011; 6: 1-11.
- Gawande A. Casualties of war: military care for the wounded from Iraq and Afghanistan. N Engl J Med 2004; 351:2471–5.
- Hagberg K, Brånemark R. Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int. 2001;25:186–194.
- Huang CT, Jackson JR, Moore NB, Fine PR, Kuhlemeier KV, Traugh GH, et al. Amputation: energy cost of ambulation. Arch Phys Med Rehabil. 1979; 60(1):18-24.
- Kane RL, Saleh KJ, Wilt TJ, Bershadsky B. The Functional Outcomes of Total Knee Arthroplasty. J Bone Joint Surg Am. 2005; 87(8):1719-24.
- Kang NV, Pendegrass C, Marks L, Blunn G. Osseocutaneous integration of an Intraosseous Transcutaneous Amputation Prosthesis Implant used for reconstruction of a transhumeral amputee: Case Report. J Hand Surg 2010; 35A:1130-34.
- Koc E,Tunca M,Akar A,Erbil AH,Demiralp B,Arca E. Skin problems in amputees: a descriptive study. Int J Dermatol. 2008; 47(5):463-6.
- Levine B, Della Valle CJ, Jacobs JJ. Applications of Porous Tantalum in Total Hip Arthroplasty. J Am Acad Orthop Surg. 2006; 14 (12): 646-55.
- Lyon CC, Kulkarni J, Zimerson E, Ross E, Beck MH. Skin disorders in amputees. J Am Acad Dermatol. 2000;42:501–7.
- MacKenzie EJ,Jones AS, Bosse MJ,Castillo RC,Pollak AN,Webb LX, et al. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J Bone Joint Surg Am. 2007;89(8):1685-92.
- Meulenbelt HE,Geertzen JH,Jonkman MF,Dijkstra PU. Skin problems of the stump in lower limb amputees: A clinical study. Acta Derm Venereol. 2011; 91(2):173-7.
- Pendegrass CJ, Goodship AE, Blunn GW. Development of a soft tissue seal around bone anchored transcutaneous amputation prostheses. Biomaterials. 2006; 27: 4183-91.
- Pendegrass CJ, Gordon D, Middleton CA, Sun SN, Blunn GW. Sealing the skin barrier around transcutaneous implants: in vitro study of keratinocyte proliferation and adhesion in response to surface modifications of titanium alloy. J Bone Joint Surg Br. 2008; 90(1):114-21.
- Perry EL, Beck PJ, Williams DL, Bloebaum RD. Assessing peri-implant tissue infection prevention in a percutaneous model. J Biomed Mater Res B Appl Biomater. 2010; 92(2): 397-408.
- Puckett SD, Lee PL, Ciombor DM, Aaron RK, Webster TJ. Nanotextured titanium surfaces for enhancing skin growth on transcutaneous Osseointegrated devices. Acta Biomaterialia. 2010; 6: 2352-62.
- Rosenbaum Chou TG, Petti CA, Szakacs J, Bloebaum RD. Evaluating antimicrobials and implant materials for infection prevention around transcutaneous Osseointegrated implants in rabbit model. J Biomed Mat Res A. 2010; 92(3): 942-52.
- Rowe DA, McMinn D, Peacock L, Buis A WP, Sutherland R, Henderson E, et al. Cadence, Energy Expenditure and Gait Symmetry During Music-Prompted and Self-Regulated Walking in Adults with Unilateral Transtibial Amputation. J Phys Act Health. 2013; [epub ahead of print]
- Sullivan, Uden M, Robinson KP. Rehabilitation of the Trans-Femoral amputee with an osseointegrated prosthesis: the United Kingdom experience. Orthotics International. 2003; 27: 114-20.
- Tillander J, Hagberg K, Hagberg L, Branemark R. Osseointegrated titanium implants for limb prostheses attachments. Clin Orthop Relat Res. 2010; 468: 2781-88.
- Williamson DF. Descriptive epidemiology of body weight and weight change in U.S. adults. Ann Intern Med.1993;119:646-49



